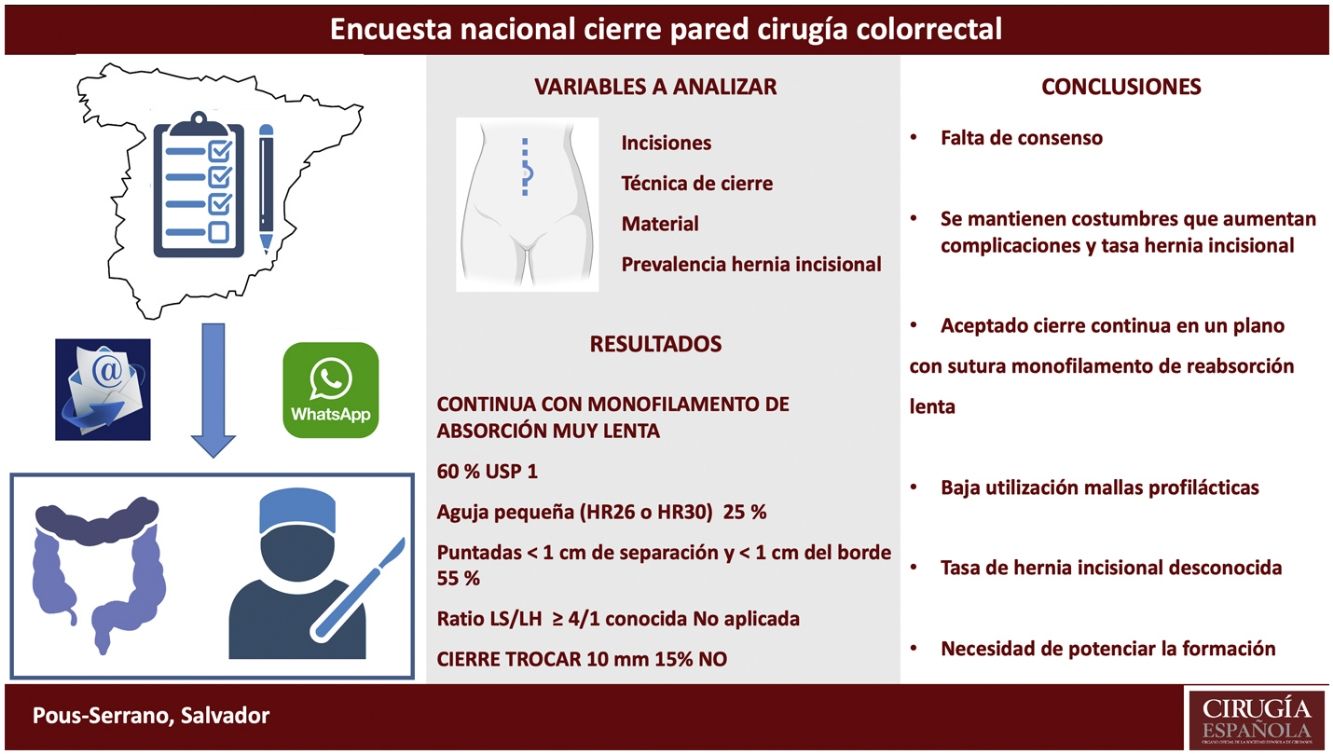
The purpose of this study is to assess the current status and knowledge of the Spanish colorectal surgeons on the wall closure.
MethodsA single answer questionnaire of 25 closed questions was conducted using specific software for online surveys that was distributed to a cohort of colorectal surgeons.
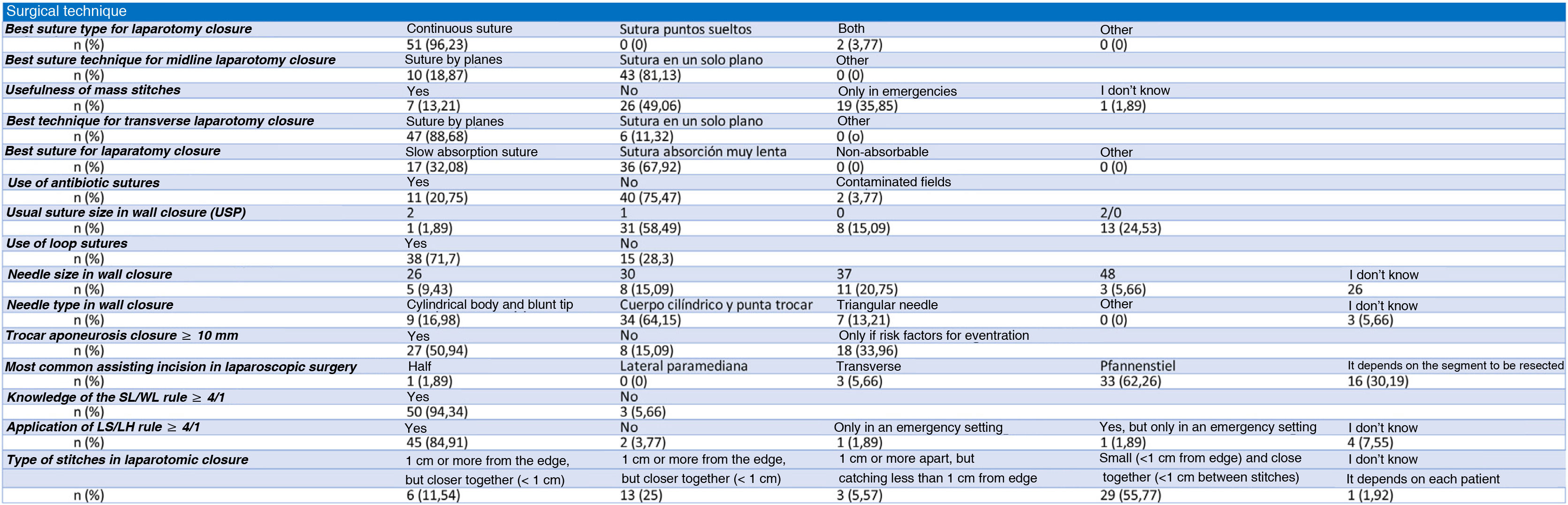
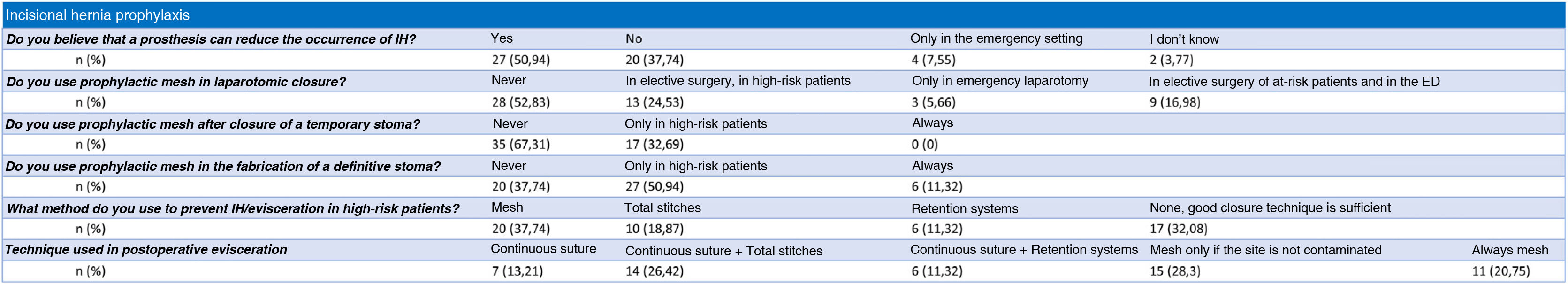
Results53 surgeons replied to the survey. The vast majority prefer a closure of the midlaparotomy with a very slow absorbing monofilament (67.92%) continuous suture (96.23%) in a single plane (81.13%). Mass stitches, retention systems, and loop sutures continue to be used. The most commonly used suture gauge was USP 1 (United States Pharmacopeia) (58.49%). The most commonly used needle is with a cylindrical body and a trocar tip. Only 50%, routinely perform wall closure after placement of a trocar equal to or greater than 10 mm. Almost everyone knows the 4:1 rule and thinks it should be applied, but the small bites technique is not performed. 50% would never place a prophylactic prosthesis. The closure is usually performed by the same surgeon who has performed the entire procedure. One out of five confesses not knowing the rate of incisional hernias in his unit.
ConclusionThere is a lack of consensus and basic knowledge regarding the technical aspects of closure and the prevention of the appearance of incisional hernias. The use of slow absorbing monofilament continuous suture in a single plane seems well accepted.
El objetivo de este estudio es valorar el estado actual y conocimiento de los cirujanos colorrectales españoles en el cierre de pared abdominal.
MétodosSe realizó un cuestionario de 25 preguntas cerradas de respuesta única utilizando un software específico para encuestas online que se distribuyó a cirujanos que se dedican, principalmente, a la cirugía colorrectal en su servicio o pertenecen a una Unidad de Cirugía Colorrectal.
ResultadosRespondieron la encuesta 53 cirujanos. La mayoría prefiere el cierre de la laparotomía media con una sutura continua (96,23%) de monofilamento de absorción muy lenta (67,92%) en un solo plano (81,13%). Los puntos en masa, los sistemas de retención y las suturas loop siguen utilizándose. El calibre de sutura habitualmente más utilizado fue del 1 USP (United States Pharmacopeia) (58,49%). La aguja más utilizada es de cuerpo cilíndrico y punta trocar. Solo el 50% realiza habitualmente cierre de la pared tras colocación de un trocar igual o mayor de 10 mm. Prácticamente todos conocen la regla del 4:1 y creen que se debe aplicar, pero la técnica de puntos cortos no se realiza. El 50% no colocaría nunca una prótesis profiláctica. El cierre lo suele realizar el mismo cirujano que ha llevado a cabo todo el procedimiento. Uno de cada 5 confiesa desconocer la tasa de hernias incisionales de su unidad.
ConclusionesSe evidencia una falta de consenso y conocimientos básicos en cuanto a los aspectos técnicos de cierre y a la prevención de la aparición de hernias incisionales. Parece aceptado el uso de sutura continua, en un solo plano, con sutura monofilamento de reabsorción lenta.
The possibility of complications arising from abdominal wall closure after colorectal surgery, such as incisional hernia, infection and/or wound dehiscence, sinus or fistula formation, is high.1,2
The rate of incisional hernia after colorectal surgery described in the literature is 14.5%–39.9%.3–6 When subgroups of patients with risk factors, such as obesity, are analysed, the figures are even higher than 50%.6
Patients undergoing colorectal surgery often have risk factors for the development of wall closure complications (advanced age, smoking, previous abdominal surgery, obesity, malnutrition, contamination during surgery, etc.).7
As this is a basic technique, but one with a major health and economic impact, measures should be put in place to monitor its safety, effectiveness and results.
An appropriate choice of incision and meticulous and careful closure of the abdominal wall, including the techniques and materials that scientific evidence indicates provide the best results, would considerably reduce the figures described.8
Prophylactic measures such as mesh placement in selected patients at high risk of developing incisional hernias could also contribute to this improved outcome.7
The aim of this study is to assess, by means of a national survey of surgeons involved in colorectal surgery, their knowledge of abdominal wall closure and their preferences regarding materials, needle types, closure technique, etc.
MethodsA questionnaire of 25 closed-ended single-response questions was drafted, a modification of one previously published by other authors.9 For its dissemination and analysis, a specific software for online surveys was used (2021 Questionpro survey software by Survey Analytics LLC 548 Market St #62790 San Francisco, CA 94104-5401 United States).
The survey was distributed to colorectal surgeons in Spain, after contacting the respondents through various means such as email and WhatsApp (https://www.questionpro.com/t/ATfPCZoQCS) (Appendix B Appendix 1 and Appendix 2). The selection of respondents was obtained by taking advantage of the contacts among colorectal surgeons of one of the authors (SPS), in addition, the board of the Coloproctology section of the Spanish Association of Surgeons was contacted to request information on surgeons from the different autonomous communities and thus obtain a nationally representative sample. All interviewees are mainly involved in colorectal surgery in their department or belong to a Colorectal or Coloproctology Surgery Unit. Only one member of these units or services was interviewed.
When contacting the interviewees, they were informed of the aim of the study and the convenience of trying to reflect in their answers the most common practice in the unit or department where they performed their surgical activity. In this way, the survey was intended to reflect the reality of wall closure in a group of colorectal surgeons in a hospital rather than a personal opinion.
Surgeons in training and surgeons whose usual activity does not focus on colorectal surgery were excluded from the study.
Respondent data were collected anonymously.
Statistical analysisFor the descriptive analysis of the results, the same software was used as for the creation and distribution of the survey and the results are presented in absolute numbers and percentages.
ResultsNo questionnaires were excluded from the analysis as there were no deficiencies that prevented the recording of the data.
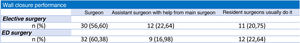
The survey was sent to 68 units or services. Fifty-three surgeons responded, i.e. 78%. It took an average time of 7 min to complete the survey.
The best suture type for median laparotomy according to the survey was continuous suture (96.23%) and the best technique for median laparotomy closure was single-plane suture (81.13%). In the case of transverse laparotomies, the majority opted for plane closure. Mass stitches continue to be used by 13.21% and 35.85% use them for closure of emergency laparotomies. Almost 50% thought they were useless.
No respondent opted for closure using non-absorbable sutures. Very slow absorbing sutures are considered the best by 67.92% of colorectal surgeons. Only 20.75% of respondents used antiseptic impregnated sutures.
The most commonly used suture gauge was USP 1 (58.49%). Almost half do not know the size of the needle they use. Large needles (37 and 48 mm) are used by one in four of the surgeons analysed. Triangular needles are still used by 13.21%. The most commonly used needle is the cylindrical body needle with trocar tip. Loop sutures are frequently used during closure by 71.1% of the respondents.
As for laparoscopic surgery, only 50% usually perform wall closure when using trocars equal to or larger than 10 mm. Fifteen per cent never close the wall. The most commonly used assist incision was the Pfannenstiel incision (62.26%).
Almost all were aware of the 4:1 rule for closure (94.34%) and believed that it should be applied (84.91%). Only 55.77% performed stitches less than 1 cm apart and less than 1 cm from the edge of the tissue.
Half believe that the placement of a prophylactic prosthesis at laparotomic closure may decrease the incidence of incisional hernia and would use it in emergency surgery and/or patients at high risk of incisional hernia. The remaining 50% would never use it. After closure of a temporary stoma, 32.69% would use it only if the patient is at high risk. The rest would never use it. The placement of a prophylactic stoma mesh to prevent para-stomal hernia is recommended by half of the respondents, but only if the patient is at high risk. Only 11.32% of the respondents usually use a prosthesis.
During the laparotomic closure procedure and in high-risk patients, 11.32% use Ventrofil® type retention systems to try to prevent incisional hernia or evisceration. If evisceration occurs, it is usually repaired with continuous suture plus total stitches, and if the surgical field is not contaminated, 28.3% use mesh.
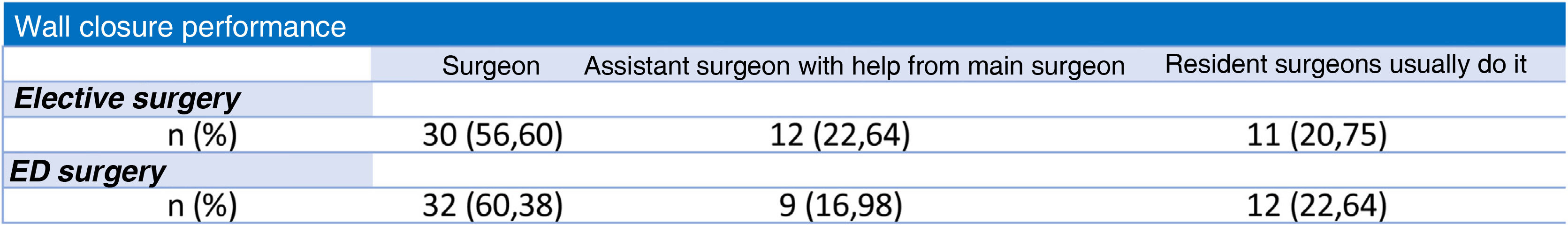
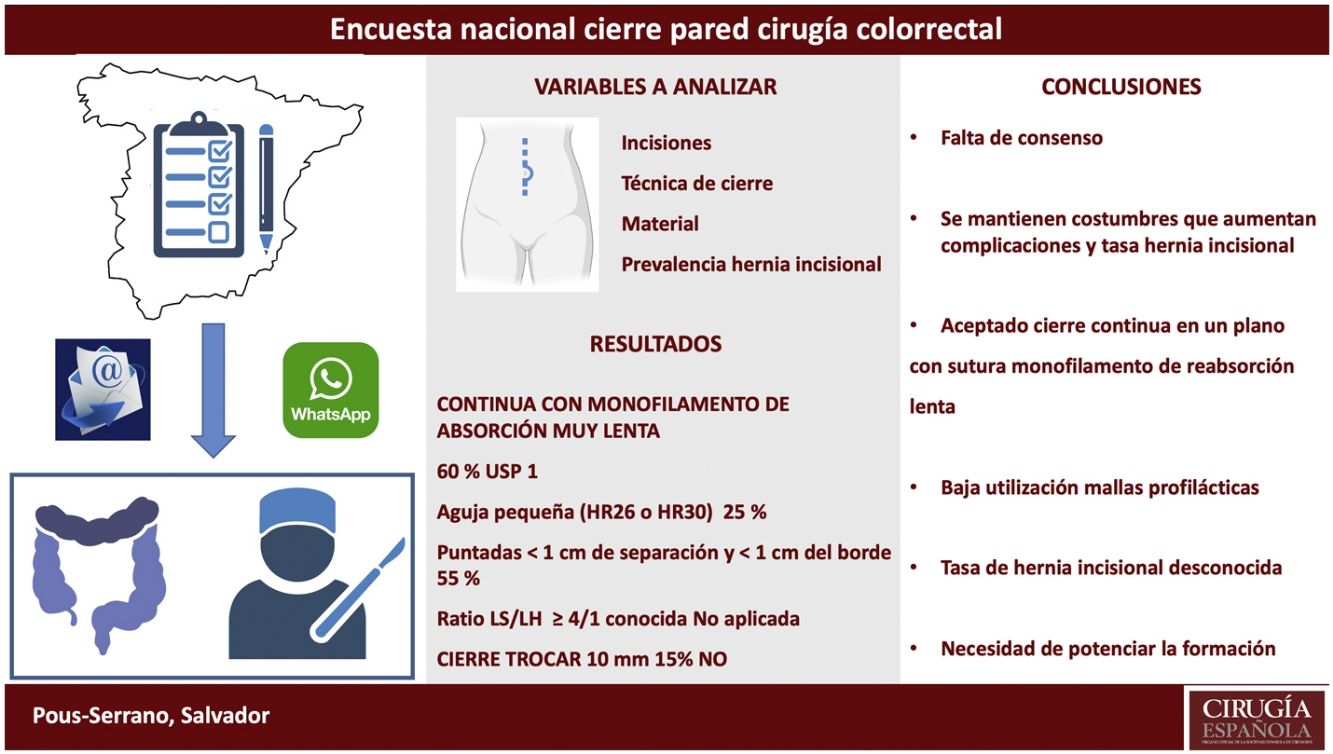
Wall closure is usually performed by the same surgeon who has carried out the entire procedure in both emergency and scheduled surgery.
One in 5 confesses that they do not know the rate of incisional hernias in their unit or department. Almost 40% say that their rate is between 5% and 10% of patients.
Detailed results are shown in Figs. 1–3.
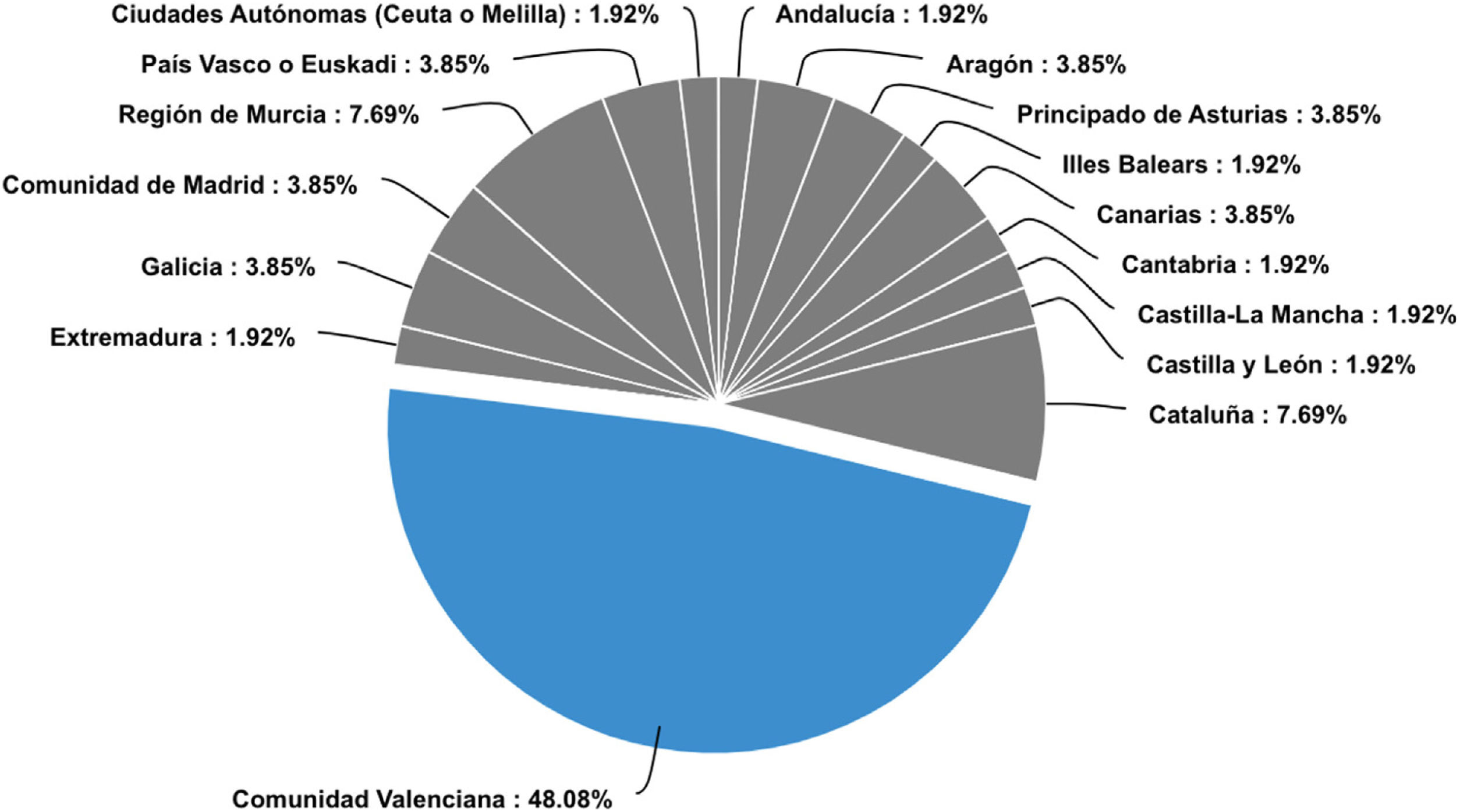
The only communities where no respondents were obtained were the Autonomous Community of Navarra and La Rioja (Fig. 4). Practically half of the respondents belong to the Community of Valencia. There are many Autonomous Communities where only one or two units responded to the questionnaire.
DiscussionThe appearance of software for online forms or surveys (QuestionPro, Google Forms, etc.) has greatly helped this type of study, as they not only allow the creation and design of the questions, but also their easy dissemination by e-mail or WhatsApp messaging and their subsequent statistical analysis. By deciding that only one member of each of the units or services would answer the survey, 53 respondents represent a significant number of colorectal surgeons in Spain.
The prevalence of incisional hernia published in previous studies is very high,3–6 although the true incidence is probably underestimated. It is important to note that one in five of the respondents reported not knowing the percentage of eventrations after mid-laparotomy in their colorectal surgery unit or service and that those who answered with a figure were far from the figures published in the literature.
Proper surgical technique and the material used to close an abdominal wall incision are crucial to reduce the risk of incisional hernia. For this reason, in 2015 the European Hernia Society (EHS) published a guide of recommendations that include avoiding midline incisions whenever possible, closure with continuous suture of the aponeurosis in a single layer without separate closure of the peritoneum, avoiding fast-absorbing sutures, using monofilament sutures with the short stitch technique and following the strand length/incision length ratio ≥ 4:110 rule. There are still many issues that are not covered by the EHS guideline, such as laparotomy closure in emergency surgery, contaminated fields or other types of laparotomies (transverse, assist incisions, trocar). The EHS also does not make recommendations on suture gauge, the use or not of loop sutures, the type or size of needle and the appropriateness of the use of retaining sutures due to lack of published scientific evidence. An experimental study in rats demonstrates a worse performance in the use of loop sutures versus the traditional continuous suture in laparotomic closure.11
In line with current recommendations, for the closure of a median laparotomy, almost everyone answered that the best type of suture was a continuous suture and that this should be done in a single plane. In contrast, most transverse laparotomies are closed in planes. Mass or total stitches, discouraged in experimental studies, are still routinely used by 13.21% of respondents and a fairly high percentage use them in the emergency setting (35.85%).12
Following current trends, no respondent opted for the use of non-absorbable sutures. Very slowly absorbed absorbable sutures were preferred. Sutures impregnated with antiseptics such as Triclosan® are not used by the majority, although a small percentage use them in contaminated fields.
The latest systematic reviews on wall closure methods only find differences in incisional hernia and complication rates in favour of using monofilament sutures but not in the other variables (layered suture, absorbable sutures, continuous versus loose sutures, slow versus fast-absorbing sutures).1,2 But these reviews do not determine the best combination of material and techniques, they only compare individual components and also exclude studies in which the interventions compared differed in more than one component.
Less than 40% use USP 0 or 2/0 suture gauges, the most commonly used being USP 1.
In addition, only one in four colorectal surgeons uses a small needle (HR26 or HR30) and almost half of the respondents did not know the size of the needle they use. These data on suture gauge, as well as the needle size used by the majority, make it difficult to believe that colorectal surgeons use the recommended small bites13 as a closure technique. Only slightly more than half report that closure is performed with small stitches (<1 cm from the edge) and together (<1 cm between stitches).
The rule of suture length in relation to wound length greater than or equal to 4:1 is known to almost everyone and they believe it should be used, but there is no evidence that this technique is performed, let alone checked at the end of closure.8,10,13
A significant percentage continue to use triangular needles (13.21%) and there are currently no publications showing worse results with their use.14 Loop sutures are used by the majority and there are no clinical publications advising against their use.11
Midline incisions for removal of the specimen in laparoscopic colorectal surgery have a higher risk of incisional hernia (10.6%) than those made outside the midline such as the transverse (3.7%) or Pfannenstiel (0.9%).15,16 The most commonly used assist incision by respondents is the Pfannenstiel incision which, although it is transverse in the skin and subcutaneous cellular tissue, the entry into the cavity is made through the median opening by separating both rectus abdominis muscles. It is true that some surgeons perform the transverse fascial section and the medial peritoneal section. Current recommendations are to try to avoid, as far as possible, assisting incisions in midline colorectal surgery.10,17
Fifteen per cent of respondents do not close the fascial opening produced by trocars of 10 mm or more. The use of bladeless trocars in recent years has decreased the incidence of trocar herniation.18 Leaving the fascia open may reduce operative time, the risk of needle stick injury and the overall cost of the procedure. Trocars in midline locations result in higher incidence rates of trocar herniation.18 Although future research is still needed to evaluate other factors that may influence hernia formation and how they can be minimised, it seems sensible to perform closure in trocars located midline.18
In the study published by Argudo et al., the use of a decision algorithm for prophylactic mesh placement after median laparotomy for colorectal cancer reduces the incidence of IH in at-risk patients.7 In our study, contrary to current recommendations, half of the colorectal surgeons would never place prophylactic mesh.
The EHS Guidelines for the Management and Prevention of Parastomal Hernia recommend, with a high quality of evidence, the use of prophylactic non-absorbable synthetic mesh when performing a terminal colostomy to reduce the incidence of the development of a parastomal hernia.19 In our survey, only 50% of respondents used prophylactic mesh in at-risk patients.
Our results indicate that a very high percentage would never place a prophylactic mesh after closure of a temporary stoma. A recent prospective multicentre randomised prospective study (ROCSS) indicates that abdominal wall reinforcement with a biological mesh at the time of stoma closure reduced clinically detectable incisional hernia within 24 months after surgery and with an acceptable safety profile.20
Although it is widely believed that wall closure is relegated to resident surgeons, this study reveals that this is not the case. Most wall closures are performed by the same surgeon who has done the entire operation. Therefore, the high incidence of incisional hernia in this subspecialty cannot be attributed to closure by trainees.
There does not seem to be adequate follow-up and recording of the occurrence of eventration after colorectal surgery as a very high percentage of respondents do not know the actual rate of incisional hernia.
The data provided by our study show that among the cohort of surgeons surveyed there is a lack of consensus and basic knowledge regarding the technical aspects of closure and the prevention of incisional hernias, with some ignoring the scientific evidence and continuing with closure practices that are associated with a higher probability of complications and incisional hernias. The use of continuous suturing, in a single plane, with slow-absorbing monofilament suture seems to be accepted. The short stitch technique is only used by 55% of respondents and the rule of the ratio of suture length to wound length ≥ 4/1 is known, but of doubtful use, so it should probably be compulsory to check it. There is also a probable low use of prophylactic meshes despite current recommendations. These facts, together with the high frequency of long and complex operations in colorectal surgery that leave the surgical team tired at the time of wall closure, also associating patients with significant risk factors (elderly, obese, neoplastic, immunocompromised, etc.), do seem to justify the high rate of incisional hernias in this type of surgery.
Limitations of this study include: 1) the possibility of approaching the wrong surgeons (who would have answered their preferences rather than those of the group to which they belong which is what they were asked); 2) the authors asking the wrong questions as some would need some nuance clarification; 3) researcher bias with some questions aimed at one type of response; 4) misinterpretation of the results of the data (the results would probably have been more reliable if the questions were multiple choice) and finally, 5) almost 50% of the respondents belong to the same Autonomous Community as the authors.
It is essential to continue to promote training in wall closure, as has been done for years by the Spanish Association of Surgeons, and even to transfer this training to other colorectal associations.
Conflict of interestsThe authors have no conflict of interests to declare related to the content of this publication.