Perforation of the gallbladder during cholecystectomy occurs in approximately 20% of the cases, and gallstones are lost in about 40% of these procedures.1 Complications are rare, and the most frequent are intraabdominal or abdominal wall infections. We report the case of a patient who had developed an abdominal wall mass 3 years after cholecystectomy. The final histologic diagnosis was adenocarcinoma of gallbladder origin.
Case ReportThe patient is a 69-year-old male who was admitted to our hospital due to constitutional symptoms and an abdominal mass that required further study. His medical history included type 2 DM, HTN, diverticulosis of the colon, and bipolar disorder. Previous surgical history included traumatic amputation of a lower limb and laparoscopic cholecystectomy due to chronic cholecystitis 3 years previously.
Clinical symptoms were abdominal pain of a month duration located in the mesogastrium and a weight loss of 24kg, with no vomiting or changes in bowel habit. Physical examination with palpation detected a painful, non-pulsatile mass in the umbilical region that seemed to be attached to the abdominal wall. Lab workup upon hospitalization was normal. Abdominal CT with contrast demonstrated a round lesion with a hypodense (necrotic) center in the abdominal wall of the umbilical region, with an approximate size of 3.6cm and apparent intraluminal extension (Fig. 1). MRI confirmed a tumor measuring 4cm×3.3cm×3.5cm with peritoneal involvement, but no relationship was observed with the intestinal loops. Images of satellite lesions were also detected, which were suggestive of small peritoneal tumor implants. Core needle biopsy was positive for malignant cells and suggested adenocarcinoma of intestinal origin (Fig. 2).
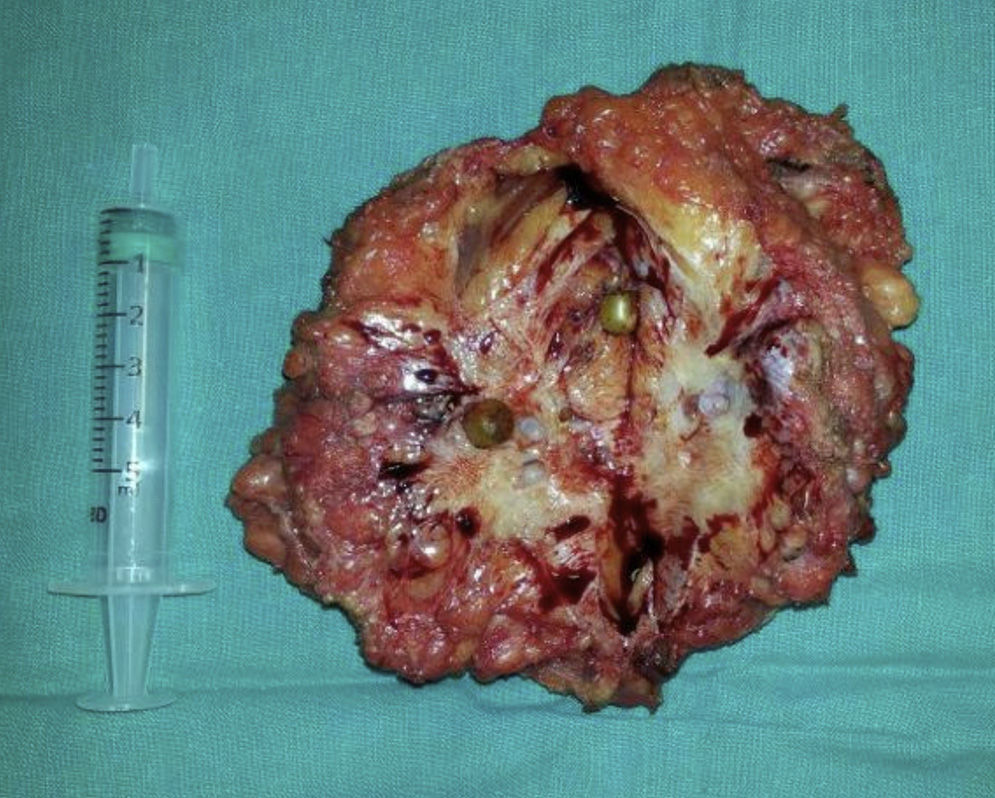
Gastroscopy and colonoscopy ruled out further malignancy. CEA levels were normal, but CA 19.9 was elevated at 2000. PET-CT did not identify any lesions other than the abdominal mass. With these findings, we decided to operate and performed a midline sub- and supra-umbilical laparotomy. An umbilical tumor was observed, which was granulomatous in appearance and contained several rounded inner lesions, giving the impression of gallstones. The lesion had focal contact with the greater omentum, and tumor implants were identified. Extensive tumor resection was carried out, including the greater omentum and peritonectomy. For wall closure, we used several continuous monofilament sutures, and it was not necessary to add mesh, which was also ruled out due to the risk of tumor recurrence.
The patient presented an uneventful recovery, and was discharged on the 7th postoperative day. Six months later, however, the patient died due to intestinal obstruction secondary to carcinomatosis.
The final pathology report confirmed that the lesion was a poorly differentiated infiltrating adenocarcinoma with predominant micropapillary features (positive for CK 7, 20, 19, CEA, and CD X2), suggestive of an extrahepatic primary gallbladder tumor.
DiscussionLaparoscopic cholecystectomy has become the treatment of choice in symptomatic cholelithiasis, with an incidence of occult cancer of 1%–2%.2 Incidental perforation of the gallbladder during the intervention can cause bile and gallstones to be released into the abdominal cavity, which even become lost in one-third of the cases.
Approximately 7%–8.5% of these lost gallstones can cause complications. The most frequent is the formation of abdominal wall and intraabdominal abscesses, although other complications include the formation of cutaneous or interloop fistulae, granulomas, or obstruction symptoms.3–6 Cases of empyemas and bronchopleural fistulas have also been reported, although they are uncommon.
Certain factors, such as signs of cholecystitis, the presence of multiple calculi (>15), pigment gallstones, large stones (>15mm), or age, increase the risk for complications.1,6 Treatment is based on the drainage of abscesses and antibiotics, and gallstone extraction is recommended.
One of the most uncommon complications, but with a poorer prognosis, is the development of tumor implants in the laparoscopy ports when the gallbladder tumor is not diagnosed preoperatively, with an incidence between 14% and 30%.7,8 This may occur in localized tumors (T1/T2) as well as in advanced stages (T3/T4). Perforation during cholecystectomy or injury to the parietal peritoneum during surgery can increase the risk of implants.9
The time interval between the intervention and relapse can range between 2 weeks and 4 years and, in most cases, at the time of diagnosis there is also carcinomatosis or distant metastasis. In general, prognosis is poor, with a mean survival of 10 months, and 5-year survival is 10%.
In the case that we describe, the cholecystectomy was difficult due to chronic inflammation and intense adherences, so the gallbladder was not bagged and was removed in fragments. As no mass was detected macroscopically, the pathology study was done routinely, which reported a gallbladder with signs of chronic cholecystitis, and no occult carcinoma was identified.
Based on the possible complications, the authors recommend extracting all free calculi and always performing complete gallbladder extraction with an endo-bag.
Conflict of InterestThe authors have no conflict of interests.
Please cite this article as: Cases-Baldo MJ, Menarguez Pina FJ, Moltó Aguado M, Navarro Rodríguez JM, Morcillo Rodenas MÁ. Diagnóstico tardío de carcinoma oculto de vesícula biliar por implante en puerto laparoscópico. Cir Esp. 2015;93:258–260.