Adrenal carcinomas are rare tumours (0.7–2 cases per 1000000 inhabitants) that present as an endocrine hypersecretion syndrome in more than 50% of patients.1 Surgical treatment is the main therapeutic option in patients with non-metastatic disease.2 The first laparoscopic adrenalectomy was described by Michel Gagner et al. in 1992,3 and it has progressively become the treatment of choice for the majority of suprarenal diseases. In the case of carcinomas, there is still much controversy, as well as relative contraindications related with size and absolute contraindications when there is distant dissemination.4
We present the case of a 20-year-old patient who reported oligomenorrhoea for the previous 2 years, deep voice, weight gain and hirsutism of the face, chest and upper extremities (Fig. 1A). Physical examination identified a non-painful mass in the right flank and clitoromegaly. The genetic study was normal; blood and urine analyses revealed notably high levels of testosterone, cortisol, 17-dehydroepiandrosterone and androstenedione. Abdominal computed tomography (CT) and magnetic resonance imaging (MRI) studies (Fig. 1A and B) detected a right adrenal mass measuring 6×7cm that was well encapsulated and showed no infiltration of neighbouring structures.
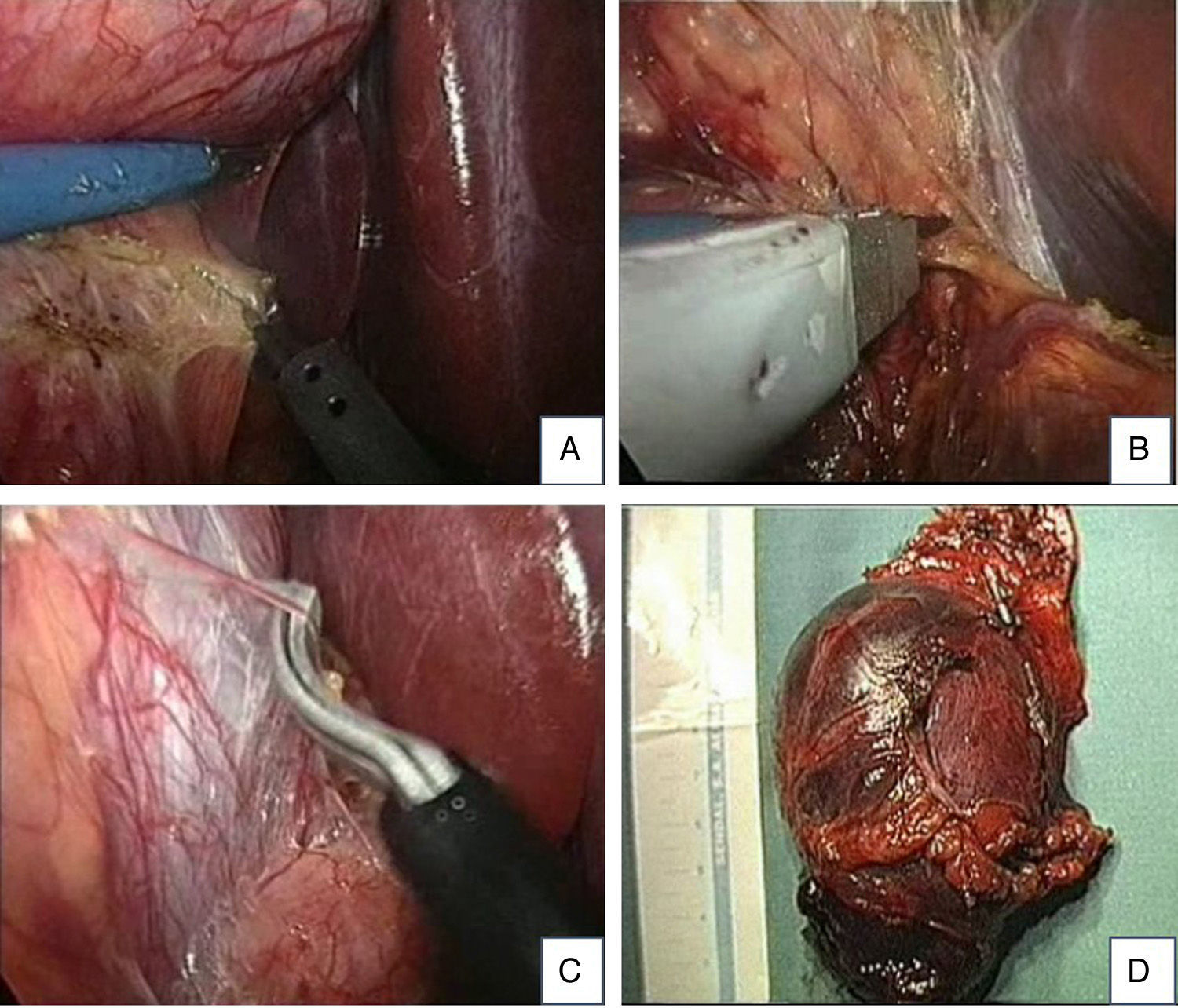
Given its size and delimitation, we opted to conduct laparoscopic right adrenalectomy using a transperitoneal lateral approach. The surgical technique was performed with the patient in left lateral decubitus. We inserted 2 10-mm trocars and 2 5-mm trocars in the right hypochondrium and flank, respectively, following the lower edge of the right ribcage. After reviewing the peritoneal cavity, the triangular ligament was divided and the Kocher manoeuvre was used to expose the inferior vena cava and the right adrenal vein (Fig. 2A–C). Afterwards, we continued with the dissection of the adrenal gland after adequate vascular control and the extraction of the surgical specimen, inserted in a protective bag (Fig. 2D). The surgical time was 110min.
The postoperative progress was correct and without incident, and the patient was discharged after 48h. The pathology study result was suprarenal adenocarcinoma without capsular infiltration. Two months after the intervention, the patient presented total remission of the adrenogenital symptoms and normalised hormone parameters. Both in the follow-up CT scan after 6 months as well as later follow-up studies, no evidence has been seen of tumour recurrence. Currently, the patient is disease-free after more than 8 years of follow-up and has presented no difficulties for gestation.
Adrenal carcinomas represent 0.2% of all cancer cases and present 2 incidence peaks in the first and fifth decades of life; they are more frequent in women.5 Although suprarenal carcinomas are potentially curable in the initial stages, only one-third are confined to the suprarenal gland when diagnosed.1 Diagnostic tests include blood tests with complete hormone profile and imaging tests (CT and/or MRI). Diagnostic biopsy taken by fine-needle aspiration (FNA) is not recommended due to the risk of dissemination or rupture.2
Adrenal virilising tumours represent 20% of hypersecretory adrenal carcinomas. They are more common in women and their manifestations include hirsutism, amenorrhoea or irregular menstrual cycles, changes in voice tone and clitoromegaly.6 Hormone studies reveal elevated serum levels of testosterone, 17-dehydroepiandrosterone sulfate and androstenedione, with increased urinary secretion of 17-ketosteroids and perhaps elevated glucocorticoids in blood.6 The differential diagnosis includes Sertoli-Leydig cell ovarian tumours, ectopic tumours and ganglioneuromas.7
In patients with localised malignancy, radical surgical excision is the treatment of choice as it is the only treatment that can achieve long-term disease-free survival.8 Although randomised studies are necessary, it seems that radical resection with lymphadenectomy (including the celiac lymph nodes, hilar lymph nodes and ipsilateral lateral aortic lymph nodes) can increase survival in these patients.9 The long-term overall prognosis continues to be poor, with an estimated 5-year survival of 16%–38%.8 Local or distant recurrences can affect 85% of cases after surgery, as determined by tumour size and stage.10
There are also no randomised studies about the indication for laparoscopic management, and this point is still being debated. The approach of choice should provide the best possibility for complete resection without rupture of the mass. The main indication for the laparoscopic approach is in stage I–II ENSATtumours (European Network for the Study of Adrenal Tumours) with a size of up to 10cm.9 Tumours larger than 10–12cm, those with adhesions, and the existence of lymphadenopathies or metastasis are considered relative contraindications (ENSAT stage III).9 Absolute contraindications include invasive adrenal carcinomas that require en bloc resections and extensive lymphadenectomy, venous thrombosis, patients with major coagulopathies or important comorbidities and malignant phaeochromocytomas.
It is currently recommended that laparoscopic surgery should only be done by expert surgical teams at reference hospitals.1 Furthermore, in cases with evidence of local invasion or technical difficulties that put the tumour capsule at risk for rupture, conversion to laparotomy is necessary for correct en bloc resection with adequate surgical margins in order to ensure greater patient survival.1
Please cite this article as: Del Castillo Déjardin D, Cabrera Vilanova A, Vives Espelta M, Prieto Butillé MR, Sabench Pereferrer F. Resección laparoscópica de un tumor virilizante suprarrenal derecho. Cir Esp. 2016;94:605–607.