Laparoscopic splenectomy (LS) is the preferred treatment of idiopathic thrombocytopenic purpura (ITP) when medical treatment fails. The objective was to evaluate the feasibility and safety of LS according to the preoperative platelet count.
MethodsThis study is a retrospective analysis of a series of 199 patients who underwent LS for ITP from 1993 to 2015. The patients were divided into 3 groups according to platelet count: group I (<10×109/L), group II (10–50×109/L) and group III (>50×109/L).
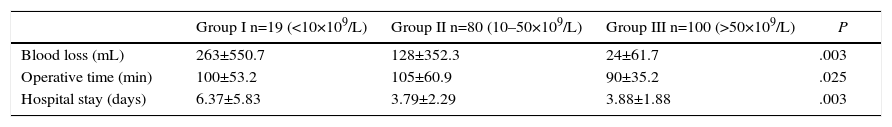
ResultsOperative time was significantly lower in Group III compared to Group I and II (100±53 and 105±61min, P<.025)). Intraoperative blood loss was statistically higher in group I (263±551ml) with respect to the other 2: group II (128±352ml) and group III (24±62ml) (P<.003). Hospital stay was 6.4±5.8 days in group I, significantly higher compared to groups II and III (3.8±2.3 and 3.2±1.8 days, respectively (P<.003)).
ConclusionConducting a LS in ITP patients with low platelet counts is effective and safe.
La esplenectomía laparoscópica (EL) es el tratamiento de elección de la púrpura trombocitopénica idiopática (PTI) cuando fracasa el tratamiento médico. El objetivo de este estudio ha sido evaluar la factibilidad y seguridad de la EL según el recuento preoperatorio de plaquetas.
MétodosAnálisis retrospectivo de una serie de 199 pacientes a los que se les realizó una EL por PTI durante el periodo 1993-2015. Los pacientes se dividieron en 3 grupos según las cifras de plaquetas: grupo I (<10×109/L), grupo II (10-50×109/L) y grupo III (>50×109/L).
ResultadosEl tiempo operatorio fue significativamente menor en el grupo III respecto a los grupos I y II (100±53 y 105±61min; p<0,025). La pérdida hemática intraoperatoria fue estadísticamente superior en el grupo I (263±551ml) respecto a los otros 2: grupo II (128±352ml) y grupo III (24±62ml) (p<0,003). La estancia hospitalaria de 6,4±5,8 días en el grupo I fue significativamente superior a la de los grupos II y III (3,8±2,3 y 3,2±1,8 días, respectivamente; p<0,003).
ConclusionesLa realización de una EL en pacientes con PTI con recuentos bajos es efectiva y segura.
The laparoscopic approach has become the technique of choice in hematologic diseases requiring splenectomy, and it is most frequently indicated for the treatment of idiopathic thrombocytopenic purpura (ITP). In these patients, the first lines of treatment are corticosteroid therapy and, more recently, anti-receptor treatment.1–4 Splenectomy is only indicated when medical treatment fails.
ITP is an autoimmune disease characterized by the destruction of platelets in the spleen, resulting in decreased peripheral levels, and it is associated with hemorrhagic clinical manifestations. Usually, platelet levels are optimized prior to surgery using corticosteroids or hyperimmune gammaglobulin. Intraoperative platelet transfusion is avoided due to the rapid destruction and because transfusion is not free of risks.6 However, it is not always possible to achieve normalized preoperative counts, and laparoscopic splenectomy (LS) sometimes needs to be done with very low platelet counts, even at levels below 30×10.9
The objective of this study was to evaluate perioperative evolution after LS in patients affected by ITP according to preoperative platelet counts.
MethodsWe analyzed patients who underwent LS for ITP and were registered in the prospective laparoscopic splenic surgery database compiled by the Surgery Department at the Hospital de Santa Creu y Sant Pau in Spain. Out of the 435 patients who had LS between 1993 and 2015, in 199 (67 males and 132 females) LS was used to treat ITP. Splenectomy was indicated in cases of thrombocytopenia associated with hemorrhagic manifestations in patients resistant to conservative treatment with steroids or immunoglobulin. The LS technique has been previously described in the literature.15
There is no consensus about the lower limit of safety of platelet counts for conducting laparoscopic procedures, although levels are usually between 30 and 50×109/L. Patients were divided empirically into 3 groups according to their preoperative platelet counts: group I, low, n=19 (<10×109/L); group II, intermediate, n=80 (10–50×109/L) and group III, high, n=100 (>50×109/L).
We collected demographic data (age and sex), analytical data (hemoglobin and platelet count), preoperative treatment used for increasing platelet count (hyperimmune immunoglobulin, corticosteroids), operative time, intraoperative blood loss, conversion to open surgery, transfusion of erythrocytes or platelets, postoperative morbidity according to the Clavien–Dindo8 classification and hospital stay.
Statistical AnalysisSPSS version 16 statistical software was used. The differences between the variables of the 3 groups were compared by ANOVA, Kruskall–Wallis and Mann–Whitney tests, as necessary. A P<.05 was considered statistically significant, and means and standard deviation were used to represent the results.
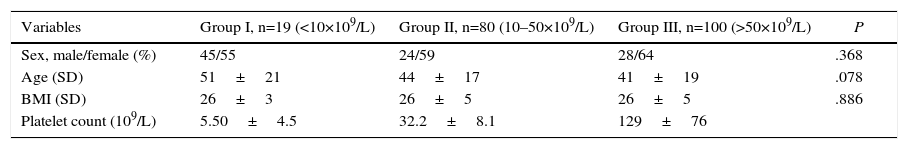
ResultsIn the cohort of 199 patients, 68% were women and 31% men. Mean age was 43±18 years (Table 1). The 3 groups were similar from a demographic standpoint and the mean preoperative platelet count was 69×109/L.
Demographic Characteristics.
| Variables | Group I, n=19 (<10×109/L) | Group II, n=80 (10–50×109/L) | Group III, n=100 (>50×109/L) | P |
|---|---|---|---|---|
| Sex, male/female (%) | 45/55 | 24/59 | 28/64 | .368 |
| Age (SD) | 51±21 | 44±17 | 41±19 | .078 |
| BMI (SD) | 26±3 | 26±5 | 26±5 | .886 |
| Platelet count (109/L) | 5.50±4.5 | 32.2±8.1 | 129±76 |
SD: standard deviation.
Mean. ANOVA value of P.
A total of 31 patients required an attempt at platelet count optimization by administering intravenous hyperimmune immunoglobulin (1g/kg, single dose) 24–48h before surgery.
The operative time of group III (90±35min) was significantly shorter (P=.025) than that of the other 2 groups (group I: 100±53min and group II: 105±61min).
Intraoperative blood loss in group I was 263±551mL, which was significantly higher than that of groups II (128±352mL) and III (24±62mL) (P<.003).
Hospital stay was longer in group I (6.4±5.8 days) compared to other groups (group II: 3.8±2.3 days; group III: 3.9±1.9 days; P<.003). Group I patients had ASA classifications higher than those in group II (10.5 vs 3.7% ASA III; P=.23).
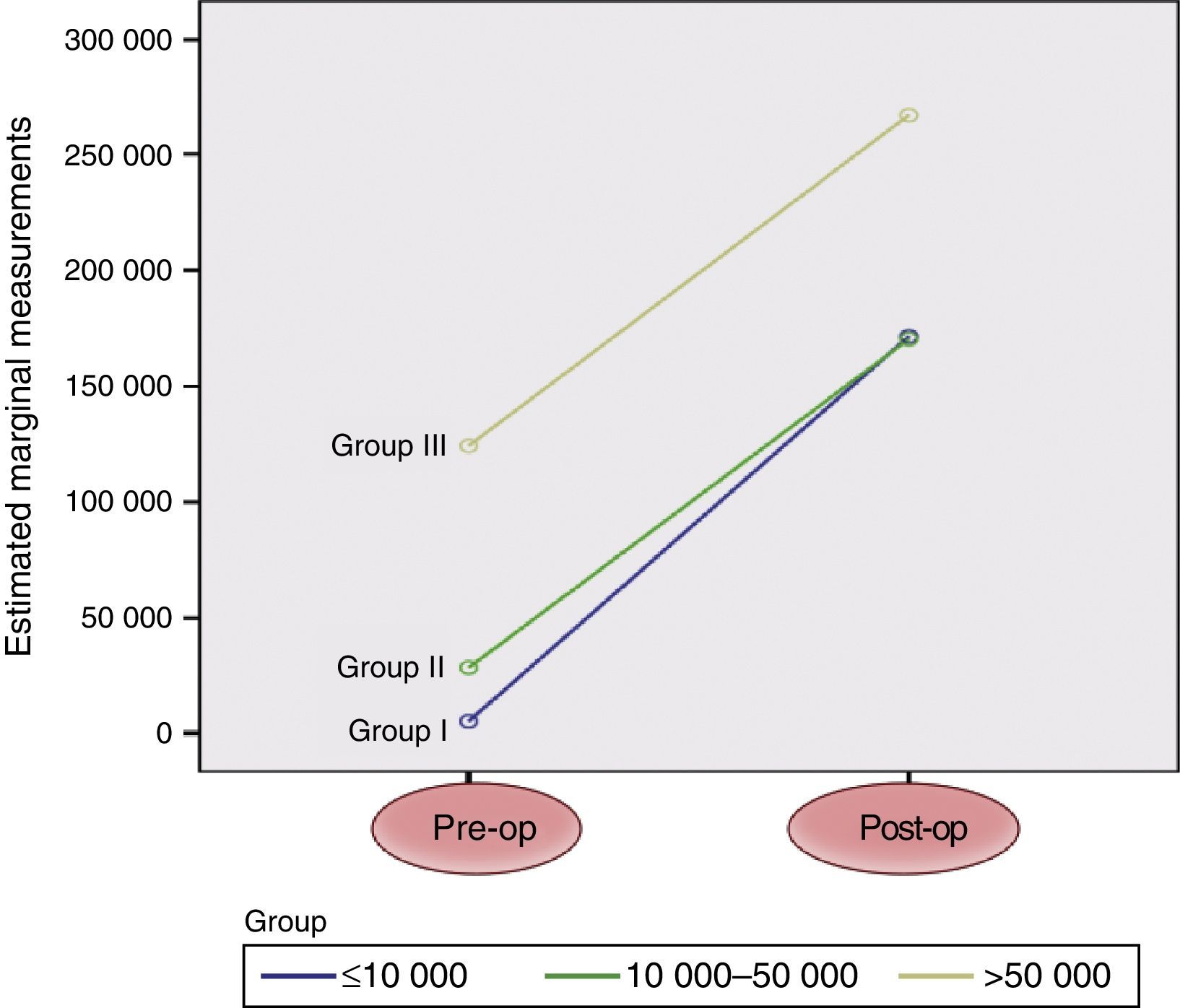
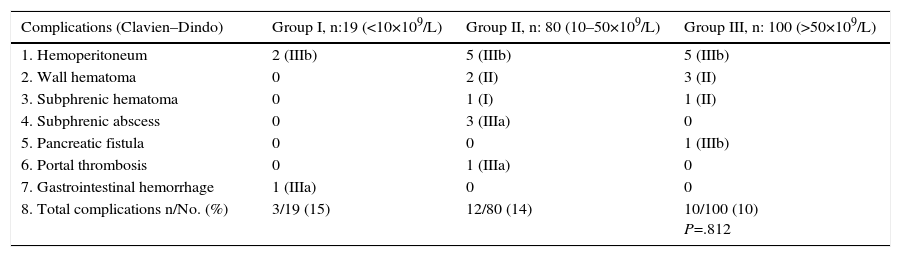
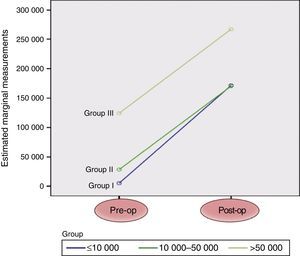
No significant differences were observed between the 3 groups in terms of the need for conversion to open surgery, postoperative complications (Table 2) or postoperative increase in platelet count (Fig. 1).
Intraoperative and Postoperative Complications.
| Complications (Clavien–Dindo) | Group I, n:19 (<10×109/L) | Group II, n: 80 (10–50×109/L) | Group III, n: 100 (>50×109/L) |
|---|---|---|---|
| 1. Hemoperitoneum | 2 (IIIb) | 5 (IIIb) | 5 (IIIb) |
| 2. Wall hematoma | 0 | 2 (II) | 3 (II) |
| 3. Subphrenic hematoma | 0 | 1 (I) | 1 (II) |
| 4. Subphrenic abscess | 0 | 3 (IIIa) | 0 |
| 5. Pancreatic fistula | 0 | 0 | 1 (IIIb) |
| 6. Portal thrombosis | 0 | 1 (IIIa) | 0 |
| 7. Gastrointestinal hemorrhage | 1 (IIIa) | 0 | 0 |
| 8. Total complications n/No. (%) | 3/19 (15) | 12/80 (14) | 10/100 (10) P=.812 |
The first line of treatment of ITP is corticosteroid therapy, and in recent years medical options have been added (thrombopoietin agonist, rituximab) to avoid the secondary effects of steroids or to avoid/postpone splenectomy. Nonetheless, splenectomy continues to be the second line of treatment in patients who do not respond to medical treatment.9,10 The British Committee for Standards in Haemathology (BCSH) recommends splenectomy in patients with platelet counts of 30×109/L that do not increase after medical treatment.11 Currently, LS in patients with ITP is a safe, effective technique,3–6 even though it was traditionally thought that severe coagulation alterations or platelet counts below 50×109/L were absolute contraindications for laparoscopic treatment. Therefore, a priority objective in the preoperative preparation of patients is the optimization of the platelet count using corticosteroids or immunoglobulin, although, in some cases, the patient's clinical condition or response to medical treatment do not allow for normalization.
In this study, we have observed that platelet counts under 50×109/L, and even as low as 10×109/L (which is a level far below the limit that, to date, had been considered empirically safe, as also reported by other authors), do not impede performing a safe LS. At the same time, LS carried out at platelet counts between 10 and 50×109/L was no different than conducting LS at counts greater than 50×109/L in terms of blood loss, operative time or postoperative complications. However, platelet counts lower than 10×109/L had an important impact on perioperative outcome, with significantly greater intraoperative blood loss, longer operative time and prolonged hospital stay (Table 3).
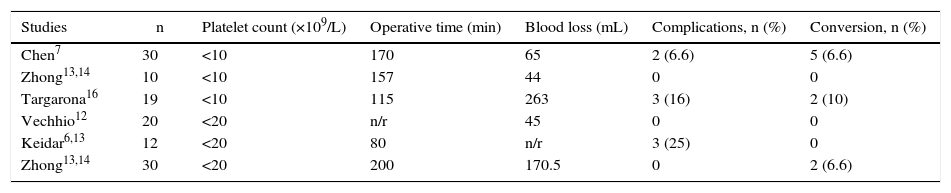
Other authors have also evaluated the impact of platelet count on perioperative patient progress after LS (Table 4). Vecchio et al.12 and Keidar et al.5,6,13 concluded that LS is a safe procedure in high-risk patients, with platelet counts >20×109/L, in whom they observed low morbidity and need for conversion to open surgery. Likewise, in patients with counts lower than 10×109/L, Chen and Zhong7,14,15 reported that LS does not cause significant bleeding compared to our results, in which the patients with lower platelet counts presented greater blood loss, with the need for blood transfusion, and longer operative time compared to the other 2 groups with higher platelet counts. As for the correlation between conversion rate and low platelet count, in our series we have found no significant relationship. This finding is similar to other authors, like Keidar,6 who also reported that platelet count did not affect conversion. However, as in our series, the Keidar series had a small number of patients in this group; therefore, it is possible that low platelet count could play a role in conversion.
Laparoscopic Splenectomy With Low Platelet Count: Review of the Literature.
| Studies | n | Platelet count (×109/L) | Operative time (min) | Blood loss (mL) | Complications, n (%) | Conversion, n (%) |
|---|---|---|---|---|---|---|
| Chen7 | 30 | <10 | 170 | 65 | 2 (6.6) | 5 (6.6) |
| Zhong13,14 | 10 | <10 | 157 | 44 | 0 | 0 |
| Targarona16 | 19 | <10 | 115 | 263 | 3 (16) | 2 (10) |
| Vechhio12 | 20 | <20 | n/r | 45 | 0 | 0 |
| Keidar6,13 | 12 | <20 | 80 | n/r | 3 (25) | 0 |
| Zhong13,14 | 30 | <20 | 200 | 170.5 | 0 | 2 (6.6) |
n/r: not recorded.
Another aspect mentioned by some authors is the use of drains. In a recent publication by Yunquiang of patient groups with very low platelet counts (like group I in our series, <10×109/L), drainage is a useful postoperative method to detect bleeding, so drain catheters are placed in all their patients.17
Currently, when LS is performed, the surgeon has resources and surgical tools that minimize the risk of bleeding: (1) the position of the patient in lateral decubitus, which medializes the spleen, thereby making its mobilization and dissection easier; (2) early ligation of the splenic artery, which reduces intrasplenic platelet destruction and favors self-transfusion; and (3) the use of instruments for vascular sealing and dissection, as well as articulated endostaplers to simplify the division of the splenic hilum and achieve better vascular control and less bleeding. The previously mentioned authors also concur on these aspects.16
To conclude, our opinion is that LS in ITP patients can be done with any platelet count in a safe manner, even at levels lower than 10×109/L. Nevertheless, low platelet counts can have an important clinical impact, with increased blood loss, operative time and hospital stay.
Authorship/CollaboratorsThe following authors have contributed to the composition of the article, critical review and approval of the final version: B. Martin, E. Targarona, J. Bollo and M. Trias.
These authors have contributed to the study design, data acquisition and collection, analysis and interpretation of the results: B. Martin, E. Tartaglia and V. Turrado.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Martin Arnau B, Turrado Rodriguez V, Tartaglia E, Bollo Rodriguez J, Targarona EM, Trias Folch M. Impacto del recuento plaquetario preoperatorio en la evolución perioperatoria tras la esplenectomía laparoscópica por púrpura trombocitopénica idiopática. Cir Esp. 2016;94:399–403.