Today, free margin surgery is the gold-standard management for soft-tissue sarcoma patients and one of the most important predictors of recurrence and survival. To obtain optimal results, a multidisciplinary approach is necessary. The aim of this study was to evaluate the evolution of patients with RPS treated by “en bloc” surgical resection versus those treated with enucleation in the first surgery.
MethodsFifty-six adult patients were divided into 2 groups. Patients in Group A underwent enucleation surgery, and patients in Group B underwent en bloc surgery. The endpoints of the study were survival time and time to recurrence, according to histological type and first surgical strategy.
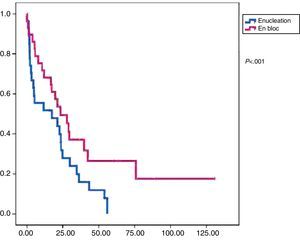
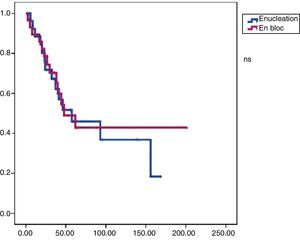
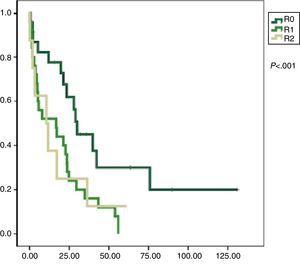
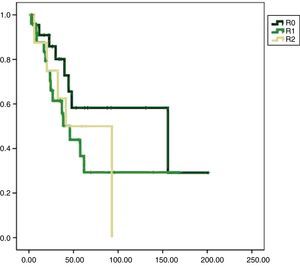
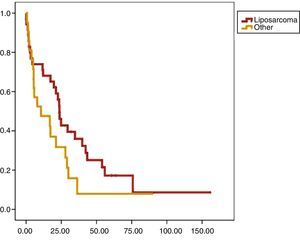
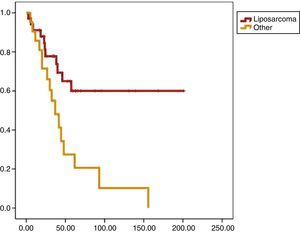
ResultsDisease-free survival was longer for en bloc surgery (P<.05), but there was no difference in overall survival. When comparing the histology of patients who underwent enucleation surgery and en bloc resection surgery, the disease-free survival and overall survival rates were longer for liposarcoma. In the multivariate analysis, only free margins and histology of liposarcoma were significantly associated with a better survival.
ConclusionsThe surgical management of patients with retroperitoneal sarcoma must be very aggressive, often requiring multivisceral resection. Considering the disease-free survival and overall survival rates obtained, it is clear that it is critical to manage patients as early as possible by a radical en bloc surgery.
La cirugía R0 con márgenes libres es el «gold-standard» en el tratamiento de los sarcomas de partes blandas, así como el mejor predictor de su recurrencia y de la supervivencia de estos pacientes. El objetivo del presente trabajo fue evaluar la evolución de los pacientes afectos de un SRP tratados mediante cirugía de resección «en bloque» frente a los tratados con enucleación en la primera cirugía.
MétodosUna serie de 56 pacientes adultos fueron divididos en 2 grupos según la resección quirúrgica. El grupo A mediante una cirugía de enucleación y el grupo B mediante una cirugía «en bloque». Se valoran la supervivencia global (SG) y el tiempo a la recurrencia (SLE), de acuerdo al tipo histológico y a la estrategia quirúrgica inicial.
ResultadosEl tiempo libre de enfermedad fue más prolongado tras una cirugía en bloque (p<0,05); no hubo diferencias con relación a la supervivencia global. Cuando comparamos el tipo histológico con una cirugía de enucleación versus una cirugía en bloque, la SLE y la SG fueron superiores en el liposarcoma. En el análisis multivariado, solo la presencia de márgenes libres y la histología liposarcoma se asociaron significativamente con una mejor supervivencia.
ConclusiónEl tratamiento de los pacientes con un sarcoma retroperitoneal debe ser claramente agresivo, requiriendo exéresis múltiviscerales. A partir de los resultados de SG y SLE, es importante que el tratamiento de estos pacientes se base en una primera cirugía lo más radical posible.
Soft tissue sarcomas are a rare entity. They represent less than 1% of tumors in adults and only 15% of cases have a retroperitoneal location (RPS).1 Their link to risk factors has been described, such as a history of extensive prior irradiation, favorable genetic conditions or the presence of chronic lymphedema.2 In most cases, their etiology is still unknown. Metastases preferentially appear in the lung and liver; they are rare in lymph node regions, and most disseminations are hematogenous.3
Currently, R0 radical surgery with free margins is the “gold-standard” treatment for these patients. According to some authors, the quality of this surgery is the most important predictor of recurrence and survival.4 Also, there is a clear association between histological grade and relapse.5 Achieving optimal therapeutic results requires multidisciplinary care, involving surgeons and specialists in radiology, pathology, oncology, and radiotherapy.6,7
This study aims to evaluate the progression of patients with RPS treated by “en bloc” resection surgery compared to those treated with enucleation in the first surgery.
MethodsA consecutive case series of 56 patients with RPS, treated surgically between June 2000 and January 2010, was reviewed. Some patients were treated primarily at our center and others, from other institutions, were referred to our center for follow-up due to recurrences or to properly complete the surgery. All patients were initially evaluated by a multidisciplinary committee.
The study protocol included a 3-phase CT and percutaneous biopsy if there were diagnosis-related doubts.
Patients were divided into 2 groups based on the type of initial surgery. The selection of the technique was based on locoregional tumor characteristics assessed intraoperatively in cases operated at our center, and at the discretion of the surgeons involved in the cases operated in other centers.
All patients had preoperative resectability criteria (tumor that affects or contacts non-vital or substitutable structures), whether or not they received neo-adjuvant radiotherapy or chemotherapy.
Two surgical strategies were studied: enucleation (group A), consisting of the removal of the tumor with its pseudocapsule without resection of the structures in contact with it (by definition, this technique is considered as an R1 resection as it lacks healthy tissue margin in the pathological examination), and en bloc resection of the tumor and contact structures, regardless of infiltration (group B).
All clinical and pathological data were recorded from the first surgery if the patient was initially treated at our center or at another institution.
The variables considered were age, sex, type, and histological grade of the RPS, the surgical technique used (with special attention to organs resected with the tumor), type of resection (R0, R1, and R2), the pathological report on resection margins, the hospital where the initial surgery was performed, morbidity according to the Clavien-Dindo scale, disease-free survival (DFS), overall survival (OS), and adjuvant treatments.8
Neo-adjuvant treatment was prescribed for patients with aggressive RPS, especially non-liposarcoma (malignant fibrous histiocytoma, leiomyosarcoma, malignant schwannoma, fibrosarcoma, and Ewing sarcoma). Intraoperative radiotherapy is not included in our protocol. For cases in which en bloc excision was not possible due to the proximity or invasion of vital structures (root of the mesentery, both kidneys, spine, etc.) or by an overly aggressive surgery not tolerated by the patient, a thorough enucleation was prescribed. According to the guidelines of the National Comprehensive Cancer Network (NCCN), patients with large and aggressive tumors such as malignant fibrous histiocytoma, leiomyosarcoma, malignant schwannoma, fibrosarcoma, and extraskeletal Ewing's sarcoma were considered for adjuvant chemotherapy or radiotherapy.9
Data was collected by a single investigator and analyzed with SPSS version 19.0. Medians were used for comparative analysis and Kaplan–Meier curves, for survival analysis. The confidence interval was 95% and statistical significance was P<.05.
We used Cox logistic regression for univariate and multivariate analysis of prognostic factors.
ResultsAll patients included in this study were assessed after RPS surgery with curative intent since 2000; since this date, en bloc surgery was included in our surgical treatment protocols. Follow-up of all patients included a minimum of 18 months after surgery (24–204 month range). Group A included 27 patients after enucleation, and group B included 29 patients after en bloc surgery.
Group ADescriptive AnalysisIn group A, the mean age of patients was 46 years (31–61 range). Thirteen patients were treated at our center, in the context of a multidisciplinary team, and the remaining 14 were treated primarily at other institutions.
The tumors were symptomatic in 66% of cases. Preoperative biopsy was performed in 40% of patients. Neoadjuvant treatment was indicated in 18.5% of patients with non-liposarcoma tumor. The surgery was optimal (R0) in 15%, marginal (R1) in 63%, and microscopic residual (R2) in 22% of patients. The average diameter of the tumor resected was 20cm, with <10cm in 18% of cases, between 10 and 20cm in 52% of cases, and >20cm in 29.6% of cases. The histopathological type was liposarcoma in 70.4% of cases, malignant fibrous histiocytoma in 11% of cases, and other types of tumors (leiomyosarcoma, malignant schwannoma, fibrosarcoma, extraskeletal Ewing sarcoma) in 18% of cases.
Tumor-free margins were obtained in 7.4% of patients. To assess the histological grade, in most patients the tumor was grade iii (59.3%), with 22.2% grade II and 18.5% grade I.
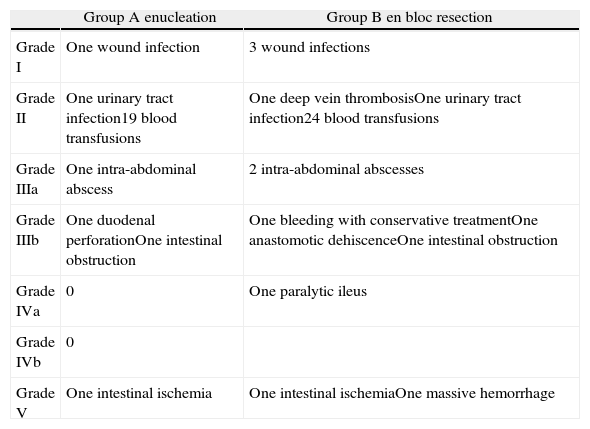
While assessing surgical morbidity according to the Clavien-Dindo classification, we observed 7.4% with grade IIIb and 3.7% (one case) with grade IV (Table 1).8 Mean hospital stay was 9.3±4 days.
Morbidity According to the Clavien-Dindo Classification.
| Group A enucleation | Group B en bloc resection | |
| Grade I | One wound infection | 3 wound infections |
| Grade II | One urinary tract infection19 blood transfusions | One deep vein thrombosisOne urinary tract infection24 blood transfusions |
| Grade IIIa | One intra-abdominal abscess | 2 intra-abdominal abscesses |
| Grade IIIb | One duodenal perforationOne intestinal obstruction | One bleeding with conservative treatmentOne anastomotic dehiscenceOne intestinal obstruction |
| Grade IVa | 0 | One paralytic ileus |
| Grade IVb | 0 | |
| Grade V | One intestinal ischemia | One intestinal ischemiaOne massive hemorrhage |
Reoperation rate was 7.4% (2 cases). Adjuvant therapy was administered in 48% of patients (40.7% chemotherapy, and 18.5% radiotherapy).
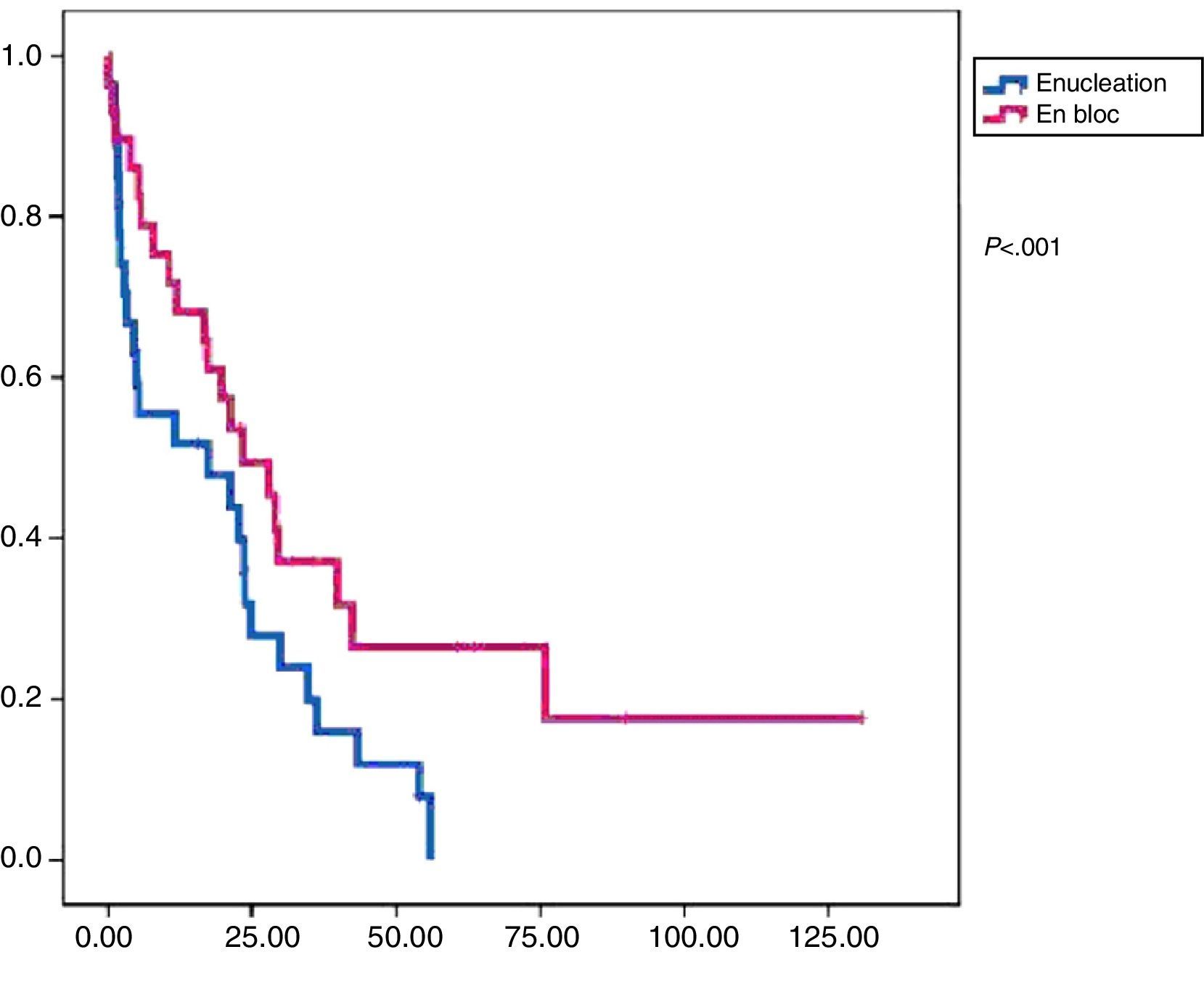
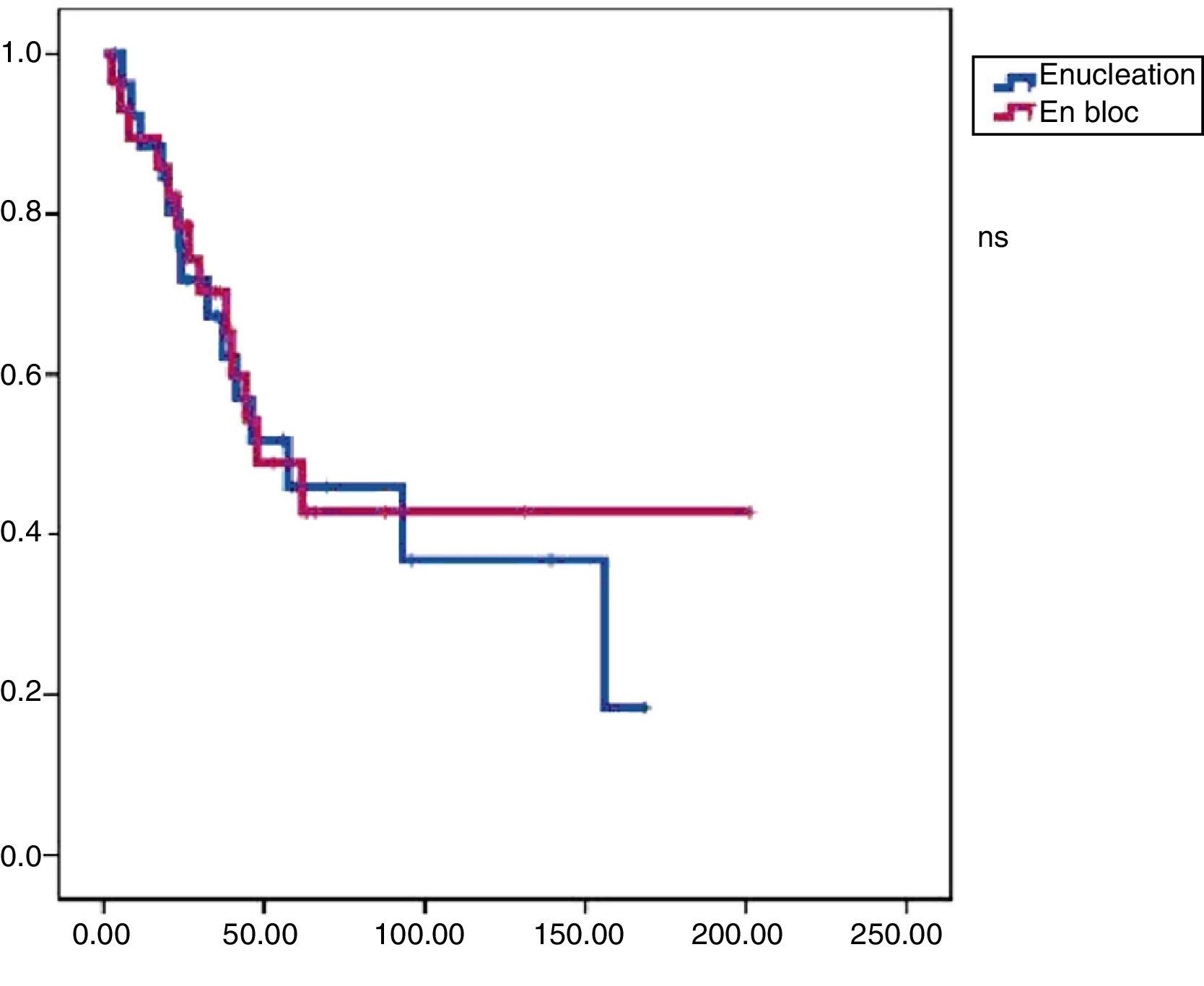
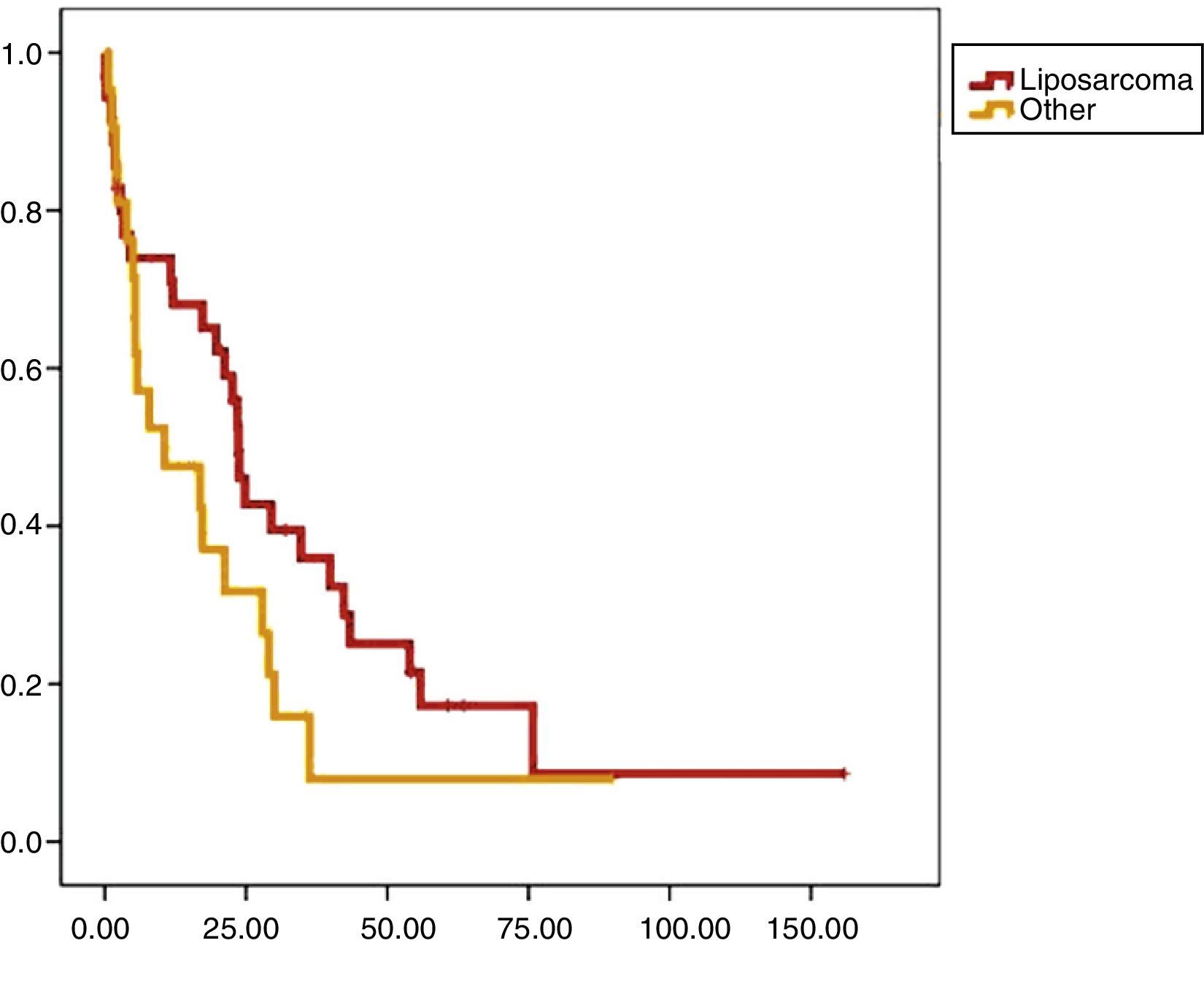
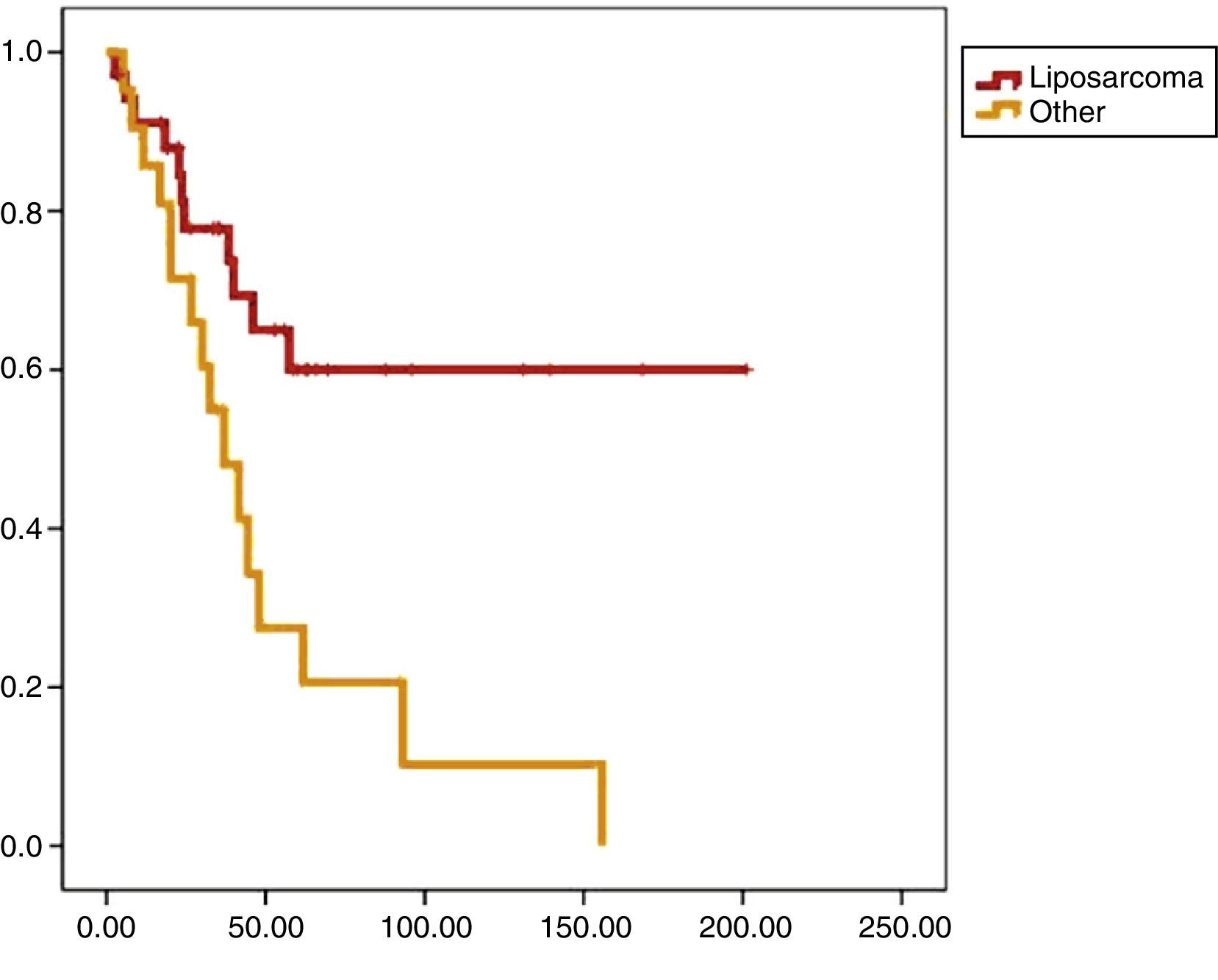
In this group, 24 patients presented recurrence within a median of 17.3 months DFS. At the end of the follow-up period, 19 patients were alive and mean OS was 47.9 months (Figs. 1 and 2).
Notably, the multidisciplinary team reassessed all patients not treated in our center, and in 70% of them, we performed a second surgery (en bloc resection) with curative intent.
Group BDescriptive AnalysisIn group B, the mean age of patients was 60 years (46–74 year range). A total of 25 patients (86.2%) were initially treated at our hospital, and only 4 patients at other institutions. The patients had symptoms in 76% of cases. Preoperative biopsy was performed in 41% of cases. Neo-adjuvant treatment was administered in 14 patients. Surgery was considered radical in all patients operated on with tumor resection associated with excision of adjacent organs or structures and not limited to the resection of the tumor and its pseudocapsule. Organs or structures associated with tumor resection were the kidney (70%), the right or left colon (44%) and other for 18% of the cases (spleen in 4 patients, psoas muscle in 6 patients, inferior vena cava in one patient who did not require reconstruction from previous thrombosis, uterus in 2 patients, pancreas in 3 patients, colon in 15 patients, and small intestine in one patient). Only one organ with tumor infiltration was resected in 10 patients, 2 organs in 13 patients, 3 and 4 organs in 2 cases respectively, and finally the excision of 5 organs in one patient. The surgeon considered the surgery as optimal in 65.5% of cases, marginal in 27.5% by resecting areas including only tumor pseudocapsule, because it was in contact with unresectable structures, and microscopic residual tumor in 7% of cases.
The mean tumor diameter was 28cm, with >20cm in 59% of cases, 10–20cm in 34% of cases, and only 7% were smaller than 10cm. Tumor subtype was liposarcoma in 55.2% of cases, malignant fibrous histiocytoma in 13.8% of cases, leiomyosarcoma in 10.3% of cases and “other” in 20% of cases. The anatomopathology report identified tumor-free margins in 51.7% of cases. The predominant histological grade was III/III in 48.3% of cases and grade II/III in 38% of cases. Observed perioperative morbidity, based on the Clavien-Dindo classification, was 14% for grade iiia, 17% for grade IIIb, and 6% for grade V (2-patient mortality) (Table 1).8 The mean hospital stay was 17.2±12 days.
Reoperation rate was 17.2%. Adjuvant treatment was administered in 55% of cases (51.7% chemotherapy and 38% radiotherapy). In this group, 14 patients presented recurrence with a median DFS of 23.4 months. At the end of the study period, 9 patients had died and the median OS was 57.3 months (Figs. 1 and 2).
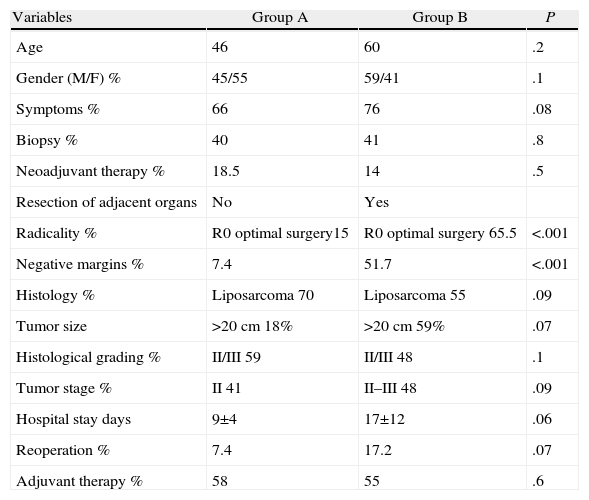
Comparison AnalysisGroups A and B were comparable with respect to all the parameters studied except radical surgery (with a higher percentage in group B) and the presence of free margins (higher percentage in group B) (Table 2). In terms of disease-free survival, group B showed better results with significant differences (P<.01) compared to group A. We also found improved overall survival in group B; however, in this case, without statistical significance (P<.08).
Comparison Between Groups.
| Variables | Group A | Group B | P |
| Age | 46 | 60 | .2 |
| Gender (M/F) % | 45/55 | 59/41 | .1 |
| Symptoms % | 66 | 76 | .08 |
| Biopsy % | 40 | 41 | .8 |
| Neoadjuvant therapy % | 18.5 | 14 | .5 |
| Resection of adjacent organs | No | Yes | |
| Radicality % | R0 optimal surgery15 | R0 optimal surgery 65.5 | <.001 |
| Negative margins % | 7.4 | 51.7 | <.001 |
| Histology % | Liposarcoma 70 | Liposarcoma 55 | .09 |
| Tumor size | >20cm 18% | >20cm 59% | .07 |
| Histological grading % | II/III 59 | II/III 48 | .1 |
| Tumor stage % | II 41 | II–III 48 | .09 |
| Hospital stay days | 9±4 | 17±12 | .06 |
| Reoperation % | 7.4 | 17.2 | .07 |
| Adjuvant therapy % | 58 | 55 | .6 |
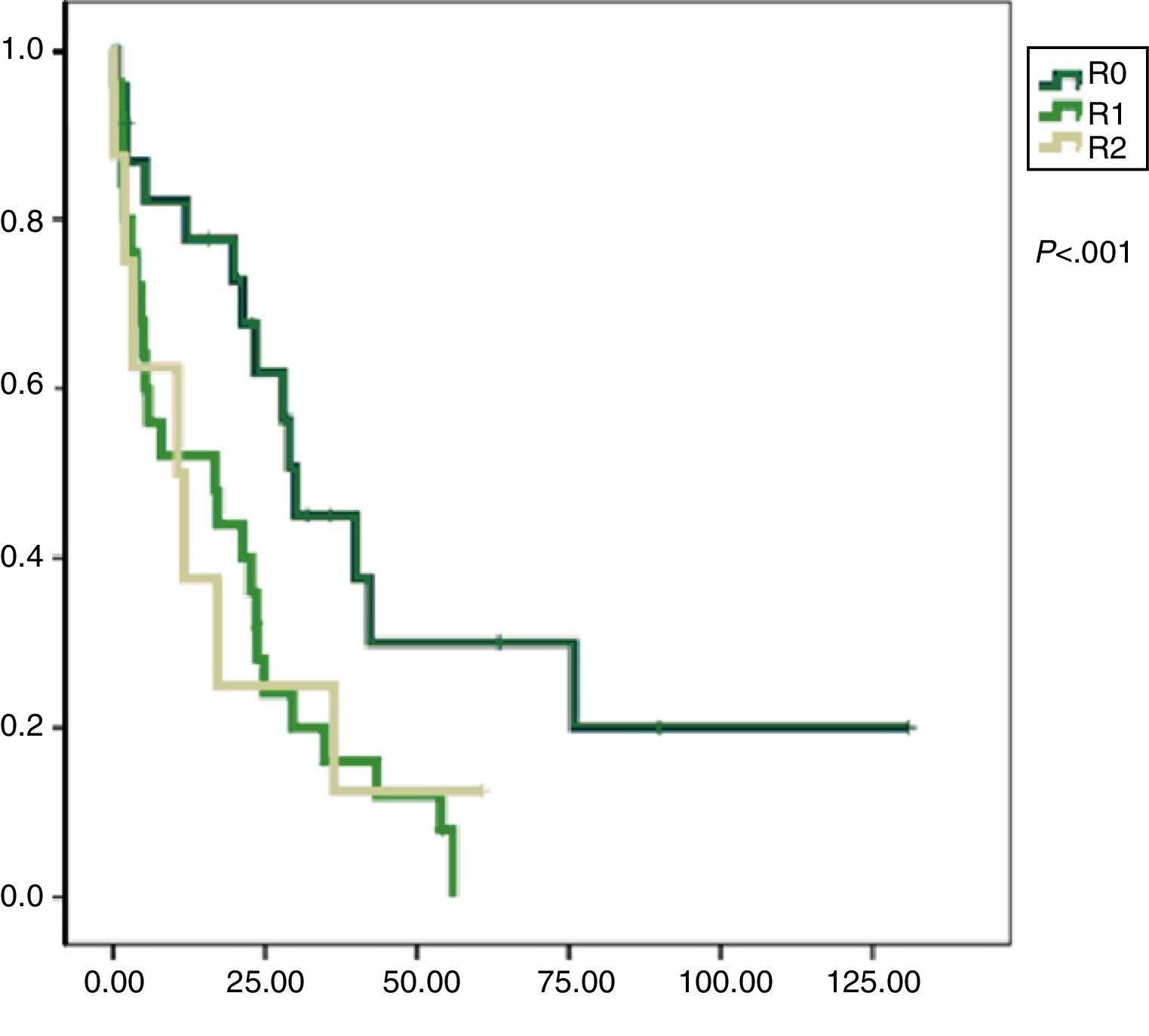
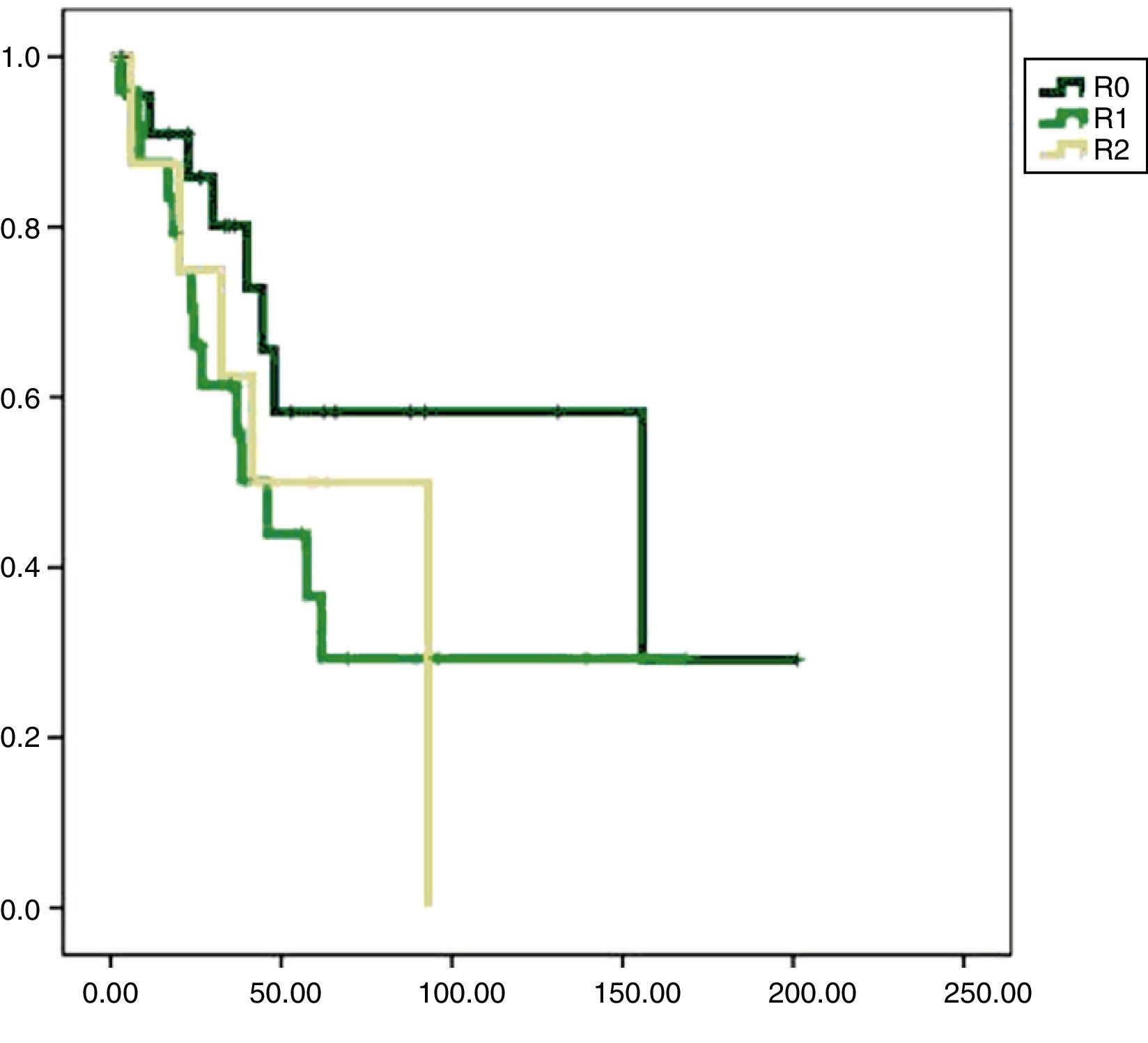
Univariate analysis found that DFS was longer in R0 resections, with a clear statistically significant difference (P<.05). However, this difference could not be observed with regard to the OS (Figs. 3 and 4). When the various histological types were compared (liposarcoma to other types), regardless of the treatment the patients underwent, DFS and OS were greater in patients with liposarcoma (Figs. 5 and 6). Multivariate analysis showed that only the radicality of the excision and histologic subtype had associated significance. R0 tumor excision and liposarcoma subtype were associated with a greater RFS (relapse-free survival), and only the subtype of liposarcoma was associated with a higher OS.
DiscussionRPS has a good medium-term survival, with 60% at 5 years after optimal surgical treatment.10 Most of the RPS are liposarcomas that, despite having a low frequency of metastasis, have a high incidence of local recurrence.11 Survival is directly related to relapse, because sooner or later, optimal resections are impossible.
Surgery is the best treatment option for RPS, especially for liposarcomas, as there is no evidence of any chemotherapeutic agent improving survival of these patients.12 Even when surgical treatment is not optimal, radiotherapy alone is insufficient for “tumor sterilization”, as indicated by previous studies.13 In our case series, neoadjuvant treatment did not produce any variation in DFS or OS, as these are factors unrelated to that treatment.
The purpose of en bloc surgery is obtaining complete macro and microscopic excision, even if this requires the inclusion of healthy retroperitoneal or abdominal organs in contact with the tumor.14,15 The retroperitoneum is not a well-defined space; therefore, a significant number of abdominal or retroperitoneal organs are often in contact with the tumor, and are not necessarily infiltrated by it. However, the importance of achieving R0 radical surgery may require resecting these organs (en bloc surgery). The published series have an optimal resection rate from 54 to 88%.15,16
In our series, the optimal surgery rate was higher in patients treated at our center than in the group of patients treated at other institutions without multidisciplinary strategies or without surgeons experienced in multiorgan excision (73 compared to 27%). These results are comparable with those obtained in the reference centers.15,16 Moreover, considering our results, it appears that the rate of severe complications was higher in the surgery group with more aggressive resections, excluding mortality, which is not comparable as it includes patients referred from other centers. Therefore, we believe that RPS en bloc resection is feasible as first line treatment with acceptable results. It is well known that the difficulties of an R0 resection increase after successive reoperations, this being particularly true of retroperitoneal lesions.11 Most patients die from complications from these recurring surgeries.
In our study, the higher rate of disease-free survival in the group of patients undergoing en bloc surgery for the first time, indicates that radical treatment is crucial from the beginning. For patients in the enucleation group, where 14 of the 27 patients were operated in centers without multidisciplinary teams, if we detected tumor relapse or persistence, we were able to perform en bloc surgery in 70% of them. It is evident that this fact contributes to the overall survival, and may explain why we find no significant differences between the 2 groups. Unfortunately, the second and subsequent surgeries, even with radical intent, often have worse outcomes.
Our study shows that an optimal initial surgery can achieve higher disease-free survival rates, and consequently, better overall survival rates. In multivariate analysis, the presence of clear margins in the tumor resection specimen and liposarcoma histology showed a higher ratio of disease-free survival as demonstrated by other authors.17–19
We can conclude that the ideal surgical procedure in patients with retroperitoneal sarcoma is an aggressive en bloc surgery, including multivisceral excision. Currently, this therapeutic approach seems the best option for patients with retroperitoneal sarcoma, especially if “en bloc” excision is planned as a first line therapy.
Conflict of InterestThe authors declare having no conflict of interest.
Please cite this article as: Gonzalez Lopez JA, Artigas Raventós V, Rodríguez Blanco M, Lopez-Pousa A, Bagué S, Abellán M, et al. Diferencias entre cirugía en bloque y enucleación en el tratamiento del sarcoma retroperitoneal. Cir Esp. 2014;92:525–531.