Colorectal cancer has a growing incidence in our society. However, the performance of laparoscopic interventions in this field is still not included in the National Training Program. Given the lack of references, our objective was to analyze the resident’s participation in laparoscopic colorectal surgery and its possible effect on morbidity and mortality and oncological prognosis.
MethodsA retrospective longitudinal single-center study that included all laparoscopic colorectal surgical procedures performed by residents (R group) and by attending surgeons (A group) between 01/01/2009 and 12/31/2017, maintaining follow-up until 12/31/2018. Postoperative morbidity and mortality, overall survival (OS) and disease- free survival (DFS), as well as their relationship with the resident involvement as first surgeon were analyzed.
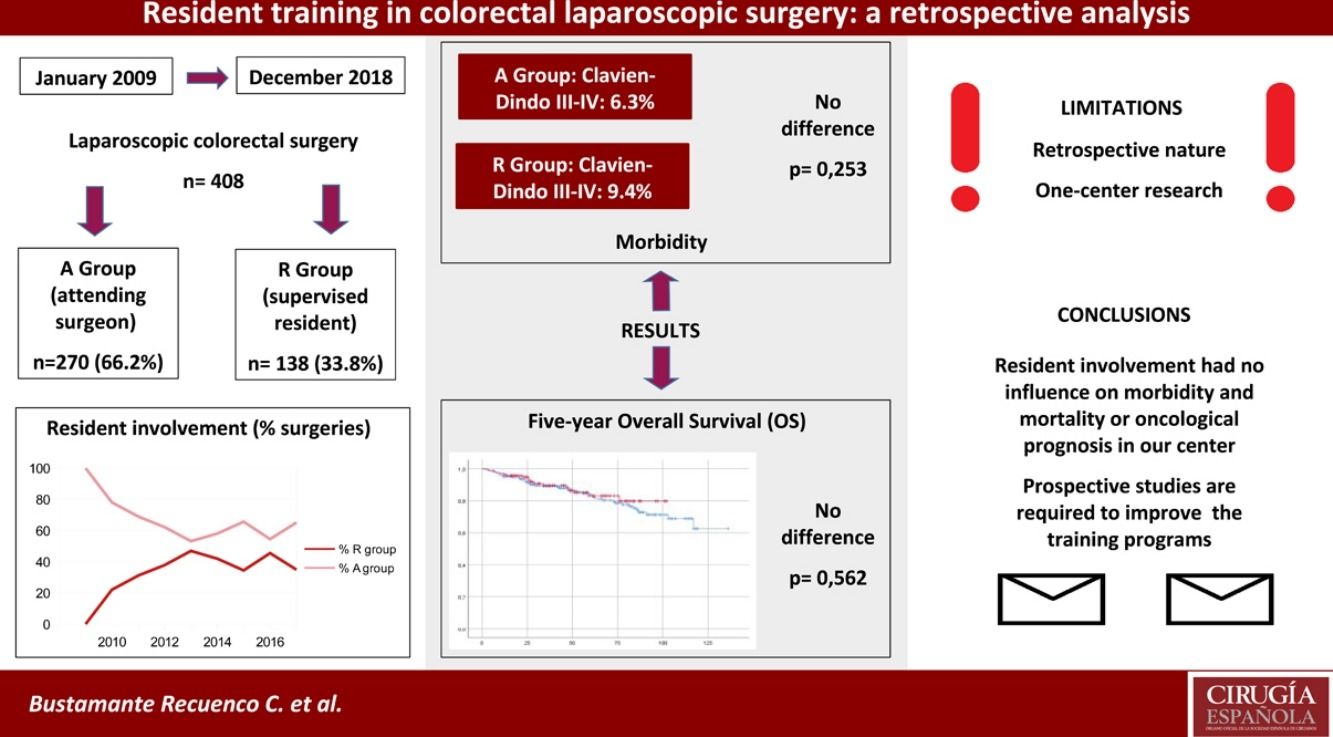
Results408 patients were analyzed, of which 138 (33.8%) were operated by a supervised resident and 270 (66.2%) by the attending surgeon. No differences were detected in the rate of postoperative complications between both groups (OR: 1.536; 95% CI: 0.947–2.409; p = 0.081). Furthermore, resident participation had no influence on tumor recurrence rate (R Group: 14.2% vs. A Group: 16.9%; p = 0.588) or on overall (p = 0.562) or disease-free survival (p = 0.305).
ConclusionResident involvement in laparoscopic colorectal surgery had no influence on morbidity and mortality or oncological prognosis in our center. Conducting prospective studies in this regard will provide greater knowledge, enabling a progressive improvement of the training program.
El cáncer de colon y recto presenta una incidencia creciente en nuestra sociedad. Sin embargo, la realización de intervenciones por laparoscopia en este subcampo sigue sin incluirse de forma protocolizada en el Programa Nacional de Formación. Ante la falta de referencias, nuestro objetivo fue analizar la participación del residente en cirugía colorrectal laparoscópica y su posible efecto sobre la morbimortalidad y el pronóstico oncológico.
MétodosEstudio retrospectivo longitudinal unicéntrico que incluyó todas las intervenciones de cirugía colorrectal realizadas por residentes (grupo R) y adjuntos (grupo A) por laparoscopia entre el 01/01/2009 y el 31/12/2017, manteniendo el seguimiento hasta el 31/12/2018. Se analizó la morbimortalidad postoperatoria, la supervivencia global (SVG) y libre de enfermedad (SLE), y su relación con la participación del residente como primer cirujano.
ResultadosSe analizaron 408 pacientes, de los cuáles 138 (33,8%) fueron intervenidos por parte de residentes bajo supervisión y 270 (66,2%) por parte de adjuntos. No se detectaron diferencias en la tasa de complicaciones postoperatorias entre ambos grupos (OR: 1,536; IC 95%: 0,947–2,409; p = 0,081). Asimismo, la participación del residente no tuvo influencia sobre la recidiva tumoral (grupo R: 14,2% vs. grupo A: 16,9%; p = 0,588) ni sobre la SVG (p = 0,562) ni SLE (p = 0,305).
ConclusionesLa realización de cirugía laparoscópica colorrectal por parte del residente no tuvo influencia sobre la morbimortalidad ni el pronóstico oncológico en nuestro centro. La realización de estudios prospectivos y de mayor evidencia proporcionará un mayor conocimiento posibilitando una mejora progresiva de la metodología docente.
The laparoscopic approach has developed and spread exponentially in recent decades in Spain. The progressive acquisition of experience and technical skills, as well as the publication of studies confirming its advantages over the open approach1,2, have contributed to its consolidation as the approach of choice in colorectal surgery.
It follows, therefore, that resident training should include learning and mastering these surgical techniques. Although the Spanish Association of Surgery (AEC for its initials in Spanish) and the Section of Endoscopic Surgery have developed specific courses in this regard, the feeling of insufficient training persists in Spain. In addition, there is a lack of updating of the National Programme of the Speciality, as only 15 cholecystectomies during residency training in laparoscopy are included as training in laparoscopy3. These factors, together with the lack of control of teaching quality at each centre, complicate the collection of objective data and the implementation of teaching. This situation makes the communication of local training programmes all the more important, as they serve as a guide and example of improvement for other centres.
In these studies, the main concern has always been safety in terms of morbidity and mortality and oncological prognosis of patients operated on by residents. In this regard, there are numerous reviews that report an absence of differences between these patients and those who undergo surgery by attending surgeons4,5. However, at national level, although teaching methodologies and results of relatively large series have been reported, most of them are non-comparative studies with a low level of evidence6,7. Thus, our aim was to evaluate and compare the morbidity and mortality and oncological prognosis of patients operated on, either by residents under supervision or by specialised colourectal surgeons at our centre.
MethodDuring the period from 01 January 2009 to 31 December 2017, we retrospectively analysed all patients undergoing colorectal surgery performed by residents under supervision or by specialised attending surgeons in this field. The end of follow-up was set for December 2018. The data were obtained through our own retrospective database.
Our centre is a tertiary public hospital with 500–600 beds. The service incorporates two residents each year who perform annual rotations of two to three months in the Coloproctology Unit. This unit has five surgeons and four to five operating theatres per week (approximately 100–110 colorectal cancer operations/year). At the end of the first year of residency, the Basic Training Course in laparoscopic surgery of the AEC is completed, and between the third and fourth year, the Phase II course of the Spanish Society of Obesity Surgery (SECO) is completed. In addition, surgical practices on experimental animals are performed twice a year.
The decision as to whether the resident physician performs the intervention is made by the attending surgeon in charge. This decision is made on an individual basis according to the experience of the resident, his/her availability and the complexity of the case. The initial approach is laparoscopic except in cases with tumour invasion of adjacent organs or multiple previous open surgeries. In right colectomies, a biplane manual extracorporeal anastomosis is performed, while in left resections it is performed intracorporeally via the transanal route.
The entire research was conducted in accordance with the principles of the STROBE initiative and the Declaration of Helsinki8. Approval was obtained from the Clinical Research Ethics Committee of our centre.
Patients over 18 years of age with benign or malignant disease who underwent initial scheduled laparoscopic surgery were included. Patients with incomplete follow-up, emergency surgery, open surgery and resections involving the middle or lower rectum were excluded. Patients were divided into two groups according to whether they were operated on by residents (group R) or by attending surgeons (group A). Surgery was considered as resident-performed if the resident successfully completed all technical procedures of the surgery. The following variables were analysed and compared: age, gender, ASA (American Society of Anaesthesiologists) anaesthetic risk, type of operation, operative time and postoperative morbidity and mortality. The Clavien–Dindo classification9 was applied to determine severity and management of complications. Overall survival (OS) and disease-free survival (DFS) were recorded separately for oncological and non-oncological patients.
Statistical analysisQuantitative variables were expressed according to the value of the mean and standard deviation if they followed a normal distribution; or according to the value of the median and interquartile range if they did not follow such a distribution. The X2 test was used as a hypothesis test for qualitative variables and the Student’s t-test or Mann–Whitney U-test for quantitative variables according to compliance with the assumption of normality. Bonferroni correction was used for multiple comparisons. In the survival analysis, the Kaplan–Meier estimator and the log-rank and Cox regression test were used as comparative tests.
The software used was the statistical programme SPSS version 25.0® (IBM, SPSS Statistics for Windows, Version 25.0. Amonk, NY: IBM Corp.).
ResultsData were collected for 408 patients, of whom 138 (33.8%) were operated on by residents under supervision and 270 (66.2%) by attending surgeons. The demographic characteristics are shown in Table 1. No differences were found in age or sex distribution. A higher ASA III anaesthetic risk was observed in group R compared to group A (23.9 vs. 14.1%; p = .013).
Patient demographic characteristics.
| Group R | Group A | P value | |
|---|---|---|---|
| n = 408 (%) | 138 (33.8) | 270 (66.2) | |
| Age (years) (IQR) | 70 (15) | 69 (13) | .215 |
| Sex | |||
| Male. n (%) | 82 (59.4) | 169 (62.6) | .533 |
| Female, n (%) | 56 (40.6) | 101 (37.4) | |
| Anaesthetic risk (ASA), n (%) | |||
| I | 9 (6.5) | 11 (4.1) | .279 |
| II | 92 (66.7) | 217 (80.4) | .002 |
| III | 33 (23.9) | 38 (14.1) | .013 |
| IV | 4 (2.9) | 4 (1.5) | .329 |
| Pathology | |||
| Benign, n (%) | 29 (21) | 51 (18.9) | .609 |
| Malignant, n (%) | 109 (79) | 219 (81.1) |
IQR: interquartile range.
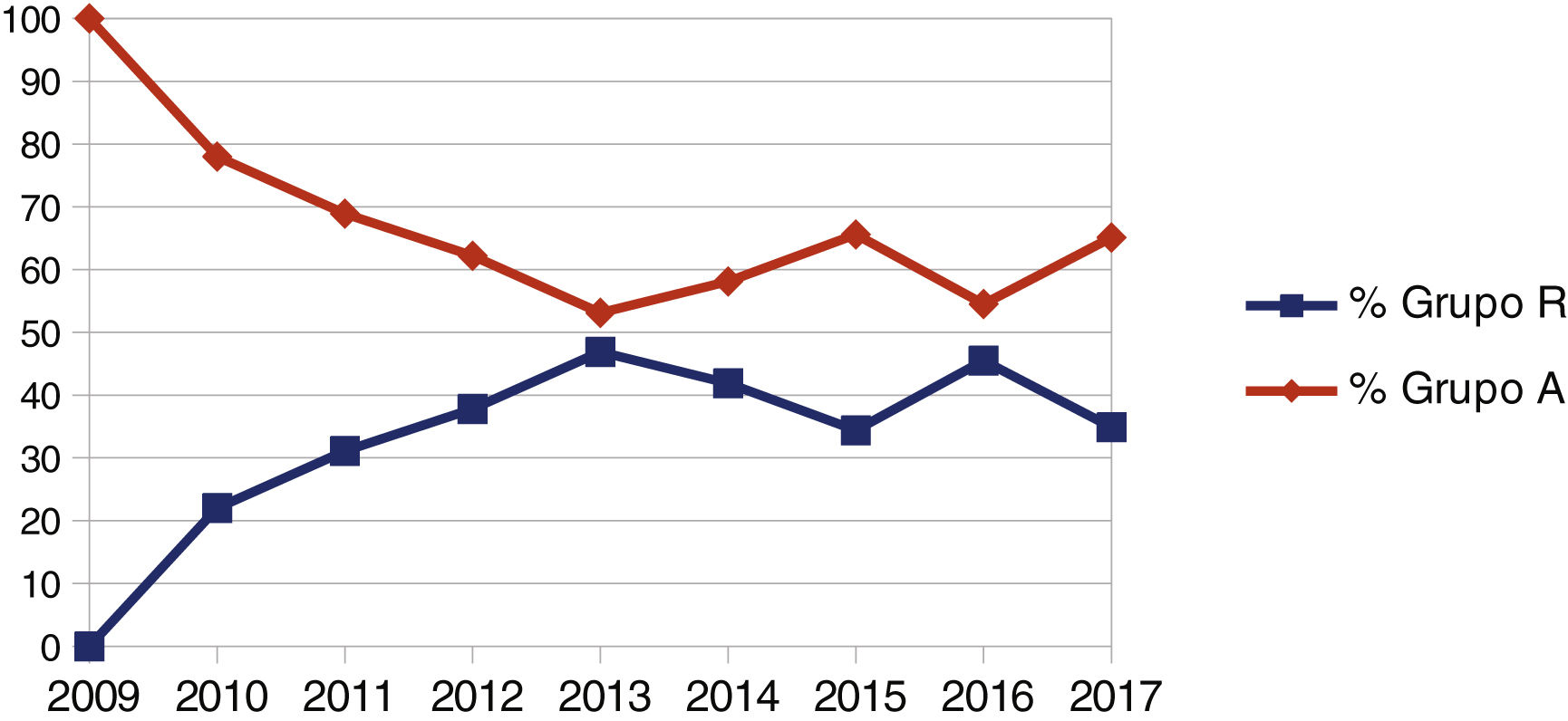
The evolution of the resident’s participation as main surgeon is summarised in Fig. 1. This shows a progressive percentage increase in the number of surgeries performed, from 0% in 2009 to an average of 39.17% between 2014 and 2017, with this difference being statistically significant (p = .001). It should also be noted that 79% of the patients operated on by residents had malignant pathology.
Residents completed more right colectomies than left colectomies (44.1% vs. 24.4% of the total; p = .001). Regarding surgical variables, no differences were detected in the duration of surgery, conversion rate or number of stomas between the two groups. No significant differences were detected in the number of total complications (OR: 1.536; 95% CI: .947–2.409; p = .081) or in those classified as Clavien–Dindo III–IV (OR: 1.548; 95% CI: .729–3.287; p = .253). There was a higher rate of intra-abdominal abscess in group R compared to group A (5.8 vs. 1.5%; OR: 4.092; 95% CI: 1.210–13.839; p = .026). Hospital stay was similar between both groups (six days group R vs. seven days group A; p = .068) (Table 2).
Interventional characteristics and postoperative morbimortality.
| Group R | Group A | P value | |
|---|---|---|---|
| n = 408 (%) | 138 (33.8) | 270 (66.2) | |
| Type of intervention | |||
| Right colectomy, n (%) | 86 (44.1) | 109 (55.9) | <.001 |
| Left colectomy, n (%) | 52 (24.4) | 161 (75.6) | |
| Time in surgery (min) (IQR) | 227.5 (90) | 210 (76) | .074 |
| Right colectomy | 222.5 (95) | 210 (70) | .296 |
| Left colectomy | 237.5 (63) | 210 (90) | .057 |
| Conversion. n (%) | 17 (12.3) | 23 (8.5) | .116 |
| Right colectomy, n (%) | 7 (5.1) | 5 (4.3) | .306 |
| Left colectomy, n (%) | 10 (7.2) | 18 (6.7) | .070 |
| Stoma, n (%) | 4 (2.9) | 5 (1.9) | .494 |
| Complications, n (%) | 37 (26.8) | 52 (19.3) | .081 |
| Right colectomy, n (%) | 26 (30.2) | 24 (22) | .192 |
| Left colectomy, n (%) | 11 (21.2) | 28 (17.4) | .542 |
| Severity, n (%) | |||
| Clavien–Dindo I | 10 (7.4) | 10 (3.7) | .117 |
| Clavien–Dindo II | 14 (10.1) | 23 (8.5) | .588 |
| Clavien–Dindo III–IV | 13 (9.4) | 17 (6.3) | .253 |
| Clavien–Dindo V | 0 (.0) | 2 (.7) | .551 |
| Type of complications, n (%) | |||
| Anastomotic leakage | 3 (2.2) | 10 (3.7) | .556 |
| Intra-abdominal abscess | 8 (5.8) | 4 (1.5) | .026 |
| Postoperative ileum | 13 (8.7) | 12 (4.8) | .122 |
| Haemorrhage | 3 (2.2) | 6 (2.2) | 1.000 |
| Surgical wound infection (SWI) | 1 (.7) | 5 (1.9) | .668 |
| Evisceration | 2 (1.4) | 1 (.4) | .265 |
| Gut obstruction | 0 (.0) | 2 (.7) | .551 |
| Pancreatic fistula | 1 (.7) | 1 (.4) | 1.000 |
| Intestinal ischaemia | 1 (.7) | 0 (.0) | .338 |
| Doctors | 12 (8.7) | 16 (5.9) | .295 |
| Reintervention, n (%) | 4 (2.9) | 12 (4.4) | .447 |
| Need for ICU, n (%) | 3 (2.2) | 16 (5.9) | .089 |
| Hospital stay (days) (IQR) | 6 (3) | 7 (2) | .068 |
ICU: intensive care unit; IQR: interquartile range.
No differences were observed in the number of nodes identified in the pathological analysis or in the tumour recurrence rate between the two groups (Table 3). The type of intervention (right or left colectomy) had no influence on the above two variables. There were 12% more pT3-4 tumours in group A than in group R, and this difference was significant (p = .016). Also, the attending surgeons tended to operate on patients with more advanced stages than the residents (TNM stage III-IV: 43.2% group A vs. 37.1% group R), although this trend was not significant.
Postoperative stage and number of resected nodes.
| Group R | Group A | P value | |
|---|---|---|---|
| n = 348 (%) | 126 (36.2) | 222 (63.8) | |
| pT stage, n (%) | |||
| pT1 | 10 (7.9) | 12 (5.2) | .318 |
| pT2 | 12 (9.4) | 17 (7.4) | .496 |
| pT3–pT4 | 82 (64.6) | 176 (76.5) | .016 |
| TNM stage, n (%) | |||
| 0 | 4 (3.7) | 11 (5.1) | .569 |
| I | 18 (16.7) | 21 (9.8) | .073 |
| II | 46 (42.6) | 90 (41.9) | .900 |
| III | 38 (35.2) | 80 (37.2) | .722 |
| IV | 2 (1.9) | 13 (6) | .091 |
| Resected nodes (n.°) (IQR | 18 (12) | 19 (12) | .536 |
| Right colectomy | 18 (12) | 21 (12) | .086 |
| Left colectomy | 18.5 (14) | 18 (11) | .898 |
| Tumour recurrence, n (%) | 18 (14.2) | 39 (16.9) | .588 |
| Local | 4 (3.1) | 11 (4.8) | .526 |
| Metastatic | 14 (11) | 28 (12.1) | .802 |
| Right colectomy | 10 (12) | 19 (18.1) | .287 |
| Left colectomy | 8 (18.2) | 20 (15.9) | .612 |
IQR: interquartile range; pT: primary tumour size and invasion; TNM: American Joint Committee classification on Cancer stages I–IV; seventh edition.
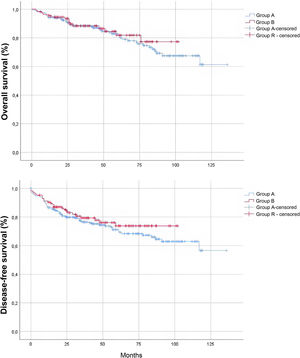
The median follow-up time, estimated by inverse Kaplan–Meier, was 56 months (95% CI 51.116–60.884). Fig. 2 shows the survival analysis of the study sample. The fact that the intervention was completed by a resident had no influence on the SVG (HR: .847; 95% CI: .482–1.486; p = .562) and SLE (HR: .788; 95% CI: .499–1.244; p = .305) of the oncology patients. Likewise, no significant differences were detected in non-oncology patients.
DiscussionTechnical skills in laparoscopic surgery begin to be developed during specialisation in general surgery. To obtain training in laparoscopic surgery, the plan only requires 30 procedures, 15 of which are cholecystectomies3. In other major laparoscopic surgical procedures, the learning curve is more blurred.
Laparoscopy is widely accepted as the approach of choice for most colorectal surgery procedures because of the advantages of a minimally invasive approach and the absence of oncological differences10–13. However, numerous studies have advocated better results in this field when performed by expert surgeons14–16. This idea, together with the gap in the training curriculum, conflicts with the development of technical skills on the part of the resident. In the last decade, several studies have shown that laparoscopic surgery performed by residents, supervised by experienced coloproctology attendings, is safe even irrespective of residency year4,5,17. These results influence patient prognosis and training programmes.
In our study, one in three patients (total n = 138) was operated on by a resident under supervision, with increasing participation throughout the study (Fig. 1). Although this may appear to be a low individual volume, this increasing participation and the concentration of interventions in fourth- and fifth-year residents (114/138 = 86.8%) means that approximately six colectomies per year/resident were performed between 2015 and 2017; and 12–18 interventions at the end of training. This figure is significantly lower than the 40–100 procedures that Targarona et al. state are necessary to acquire adequate technical competence18. This teaching limitation in our case is generated by the surgical volume of the unit. The similar situation of most hospitals nationwide and the high participation of residents as a percentage in our series mean that we consider our results to be correct.
This training deficit is not specific to Spain. Postgraduate training has been developed in the USA through nationally regulated fellowship19 type programmes. In the old continent, although such programmes exist and some are of high quality, their protocolisation and state recognition is not homogeneous. Some countries have chosen a different path in this regard, the United Kingdom being an example to follow, as the development of the national LAPCO programme for training in laparoscopic colorectal surgery led to an increase in the laparoscopic approach and a general decrease in morbidity and mortality20. A similar initiative to improve training would be very useful in the Spanish setting.
The learning curve can be measured by variables such as surgical time. Some studies have found no differences in morbidity, but a longer surgical time in surgeries performed by residents. Residents21. In our case, there are no differences in this variable, a fact that may be justified by a tendency in the selection of cases. Patients with larger tumours and more advanced stages were more frequently operated on by specialised attendings. This selection is justified in several studies to reduce morbidity and mortality and to facilitate learning. Aprendizaje4,5. Factors such as the experience of the attending or the resident's own skills may also have had an influence in this regard. As these factors are complex to quantify, they were not included in the analysis. However, these biases are present in almost all training studies and, in our opinion, do not detract from the validity of our results.
Resident surgeons operated almost twice as many right colectomies as left colectomies (86 vs. 52), possibly due to the performance of the anastomosis at the extracorporeal level in right resections. With regard to the conversion rate, although some groups publish rates in the resident group of up to 24% vs. 4% of the attending surgeions4, in our case we did not see this difference. Of note was a higher number of conversions in left resections, although this difference was not significant. We also documented no difference in the stoma rate between the two groups. It should be noted that rectal surgeries were excluded in this study. Although this could have an impact on the results as these are complex surgeries with anastomosis with a higher risk of dehiscence, some authors have also published no differences in surgical variables when rectal surgery is performed by residents21. Due to the volume of our unit, this surgery is performed by only a few members of the team.
In our sample, and in accordance with the results of Wojcik’s work, surgeries performed by residents did not result in greater postoperative morbidity and mortality or longer hospital stay17. According to the Clavien–Dindo classification, no differences were observed in terms of major complications (III–IV). Although the rate of intra-abdominal abscesses was higher in the residents' group, this event was treated with antibiotherapy in most cases. Equality in terms of complications was maintained despite a higher percentage of ASA III patients in the R group. The possible increased risk of complications due to the anaesthetic risk may have been offset by the lower tumour stage of the patients operated on by residents, which may have resulted in less technical difficulty and a better preoperative nutritional status.
Although there is broad evidence on the effect of teaching on morbidity and mortality, published evidence on oncological outcomes is limited4,5,22,23. In our series, the malignant nature of the disease was not a criterion for residents not to perform surgery, as 79% of patients in group R had this condition. In this subgroup, we found no difference in the number of nodes removed or in the recurrence rate (14.2% group R vs. 16.9% group A; p = .588). Furthermore, with a mean follow-up of almost five years, the interventions performed by residents did not have worse results in terms of SVG and SLE. The higher tumour staging of the patients operated on by residents may have influenced the prognostic equality of our work.
Our study has the limitations of retrospective data collection studies in relation to intraoperative findings, technical difficulties and reasons for conversion. It is also a single-centre study, which limits the external validity of the results. On the other hand, there is a bias in the selection of patients who were operated on by each group, depending on the complexity of each case. In this sense, we intend to develop our own selection protocol to ensure proper teaching without compromising patient safety. However, despite these limitations, this is an extensive series, drawn from an experienced unit and which includes a correct prognostic analysis of the oncological patients.
ConclusionsBased on our results, it can be concluded that resident participation in laparoscopic colorectal surgery is a safe practice in our centre, as it has no effect on patient morbidity and mortality or oncological prognosis. Further work with more evidence in this regard, as well as a detailed study of the effect of the experience of the resident and the attending on surgical outcomes, are necessary to improve the teaching methodology in our country.
FinancingThis research has received no funding from any collaborative entity.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Bustamante Recuenco C, Alonso-Lambertí Rizo L, Salazar Carrasco A, Valle Rubio A, Cendrero Martín M, Jiménez Carneros V, et al. Formación del residente en cirugía laparoscópica en coloproctología: análisis retrospectivo de morbimortalidad y pronóstico oncológico sobre 408 pacientes en nuestro centro. Cir Esp. 2022;100:555–561.