Crohn’s disease (CD) is histologically characterized as having transmural and patchy involvement of the entire intestinal tract.1 Ileal and ileocolic involvement (L1 and L3 of the Montreal classification, respectively) are the most frequent locations of the disease.2 Currently, and despite the advent of biological treatments, more than half of patients with CD undergo surgery within 10 years of diagnosis. Usually, and although surgery resolves the condition, it is not curative and new procedures are frequently needed due to stenosis in previous anastomoses or new outbreaks of the disease. Within 10 years of an initial intervention, 35% of patients will need some type of reoperation.3
Endoscopic dilation has demonstrated efficacy in the treatment of stricture, both in primary (novo) stenosis and in short-term anastomotic stenosis.4,5 However, the long-term results are controversial.6,7
Our main objective was to evaluate the clinical results of the treatment of anastomotic stenosis of CD with a stenotic pattern using either surgery or endoscopic dilation, and we have conducted a retrospective analytical study from 1990 to 2019 at a tertiary hospital.
Clinical anastomotic stricture was defined as stenosis that required another procedure, either endoscopic or surgical.
The inclusion criteria were: diagnosis of CD with at least a stenotic pattern, age over 18 years, previous ileocecal resection due to stenosis, and having undergone endoscopic or surgical treatment of the anastomosis due to clinical recurrence.
Patients under 18 years of age, those without a follow-up, resections other than ileocecal resection, and strictureplasties were excluded. Likewise, procedures for causes other than stenosis were omitted.
A total of 35 procedures were analyzed, including 21 (60%) endoscopic dilations and 14 (40%) surgical procedures, in 19 patients. The indication of the procedures was determined by a multidisciplinary committee that included gastroenterologists and surgeons.
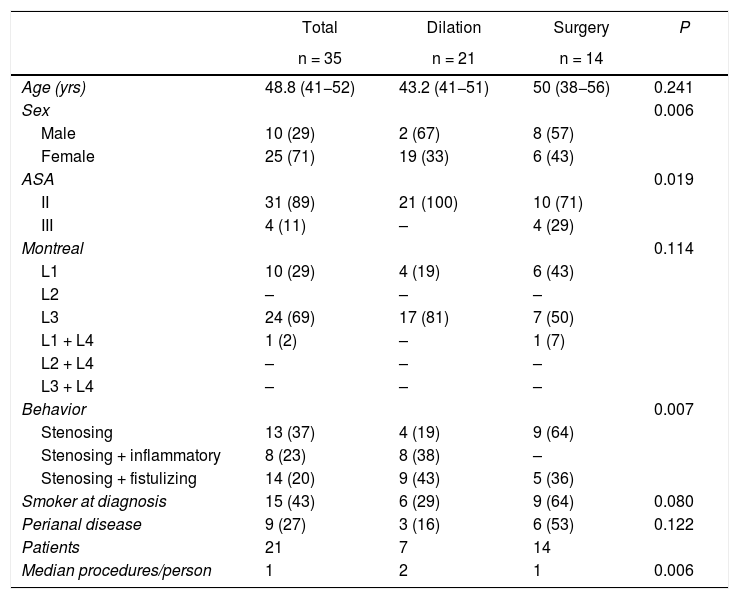
The median follow-up of the sample was 10.8 years (5–25). The median age was 48.8 (40–52) years, with no differences between groups (P = 0.241). 89% of the patients were ASA II. Four patients were considered ASA III, all of them in the surgical group.
The Montreal classification refers to the phenotype of the disease at diagnosis. Most of the patients were grouped between L1 and L3 (L1 [4 dilation vs 6 surgery]; L3 [7 dilation vs 7 surgery]).
The distribution of the theoretical phenotypes was quite homogeneous. This result is in line with the current concept that the chronic and progressive nature of intestinal damage in CD is manifested as several different complications, such as stricture, fistulae and abscesses.8 The remaining sociodemographic and clinical characteristics are summarized in Table 1.
Characteristics of the sample.
| Total | Dilation | Surgery | P | |
|---|---|---|---|---|
| n = 35 | n = 21 | n = 14 | ||
| Age (yrs) | 48.8 (41−52) | 43.2 (41−51) | 50 (38−56) | 0.241 |
| Sex | 0.006 | |||
| Male | 10 (29) | 2 (67) | 8 (57) | |
| Female | 25 (71) | 19 (33) | 6 (43) | |
| ASA | 0.019 | |||
| II | 31 (89) | 21 (100) | 10 (71) | |
| III | 4 (11) | – | 4 (29) | |
| Montreal | 0.114 | |||
| L1 | 10 (29) | 4 (19) | 6 (43) | |
| L2 | – | – | – | |
| L3 | 24 (69) | 17 (81) | 7 (50) | |
| L1 + L4 | 1 (2) | – | 1 (7) | |
| L2 + L4 | – | – | – | |
| L3 + L4 | – | – | – | |
| Behavior | 0.007 | |||
| Stenosing | 13 (37) | 4 (19) | 9 (64) | |
| Stenosing + inflammatory | 8 (23) | 8 (38) | – | |
| Stenosing + fistulizing | 14 (20) | 9 (43) | 5 (36) | |
| Smoker at diagnosis | 15 (43) | 6 (29) | 9 (64) | 0.080 |
| Perianal disease | 9 (27) | 3 (16) | 6 (53) | 0.122 |
| Patients | 21 | 7 | 14 | |
| Median procedures/person | 1 | 2 | 1 | 0.006 |
Out of the total of 19 patients analyzed, surgery was selected as the initial procedure for 14 patients, and the surgical option resolved the condition in 12 patients. The other 2 patients required one dilation per patient to resolve the condition. Out of the 5 patients whose initial treatment was dilation, none required salvage surgery.
The median number of procedures in the surgical group was 1 (1–1). This datum contrasts with endoscopic dilations, where the median number of procedures per person was 2 (1–7). This difference is statistically significant (P = 0.006). However, although the patients required more procedures in the endoscopic group, in our sample none required salvage surgery during follow-up.
The mean length of the stenosis was 4.6 ± 0.7 cm.
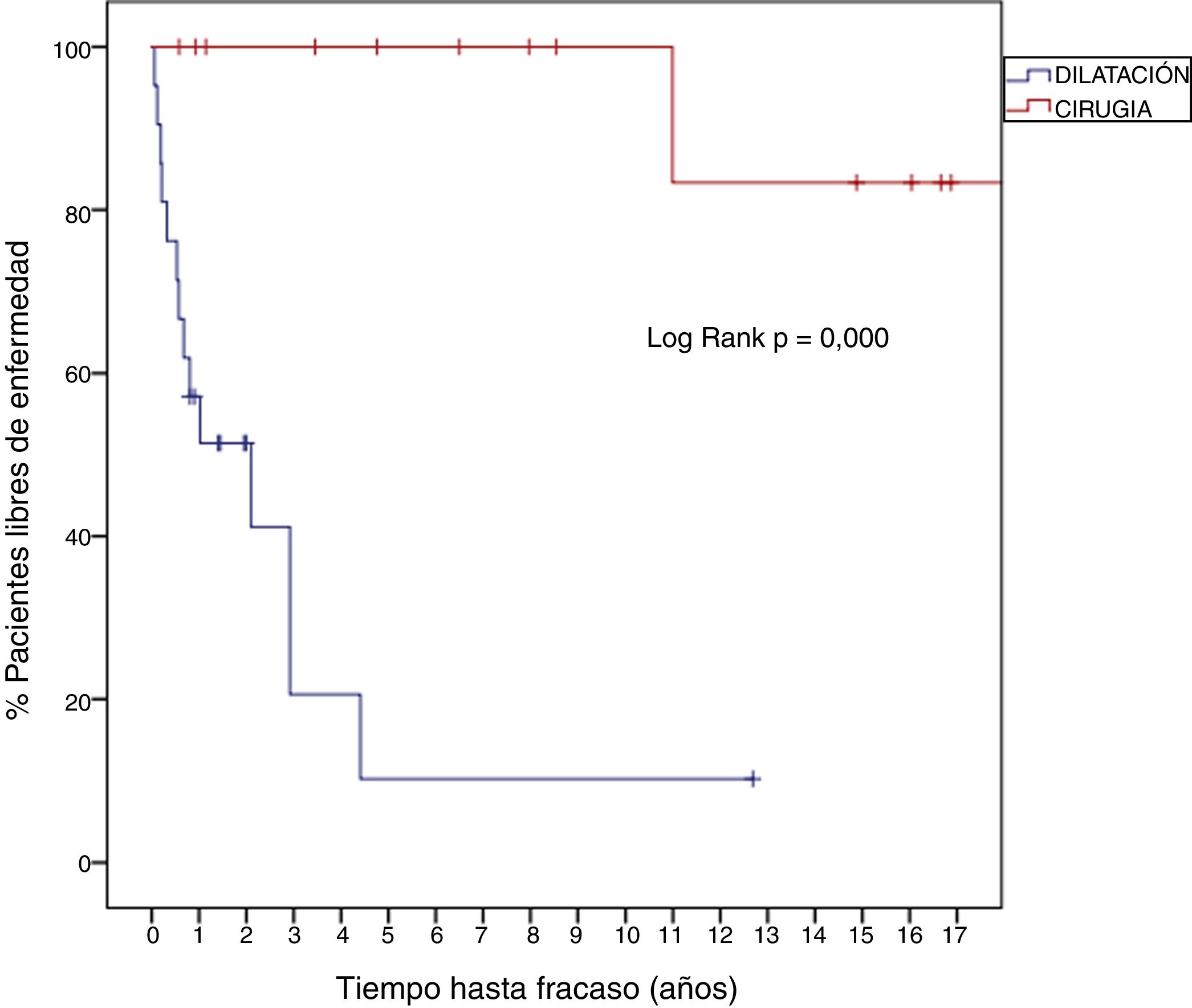
The median disease-free time until a new procedure was needed was 8.25 years (2.9–16.2) in the surgical group compared to 0.9 years (0.4–2) in the endoscopic dilation group (Log Rank P = 0.000; HR 0.041; 95%CI 0.005–0.329) (Fig. 1).
One year after surgery, the 14 patients (100%) remained asymptomatic; meanwhile, the first year after dilation, 52% of the patients required another procedure. After 12 years, 83% of surgical patients had not required additional treatment; in the endoscopic group, all patients had undergone more therapeutic sessions.
Seven of the surgical patients (47%) presented complications, which were 85% Clavien-Dindo I and II. In one patient, a ureter was injured during surgery, requiring placement of a double J catheter with subsequent reoperation for removal. In the endoscopic procedures, no major complications (perforation or bleeding) were reported.
As the main limitation, the mean length of the stenosis demonstrated as a prognostic factor for success slightly exceeded the recommendations of previous series.7
Until now, few series have evaluated the outcome of endoscopic dilation for recurrent anastomotic stricture in CD. Our results suggest that surgery achieves a higher success rate with a single procedure than endoscopic dilation, but the tradeoff is a greater number of complications. For this reason, and in addition to the patient’s preferences, the decision on the treatment of ileocecal anastomotic stenosis in CD should be made within a multidisciplinary committee.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Juez Sáez LD, Ocaña J, Ramos D, Die J, García Pérez JC. Manejo de la estenosis anastomótica tras una resección ileocecal en la enfermedad de Crohn con patrón estenótico. Cirugía vs. dilatación endoscópica. Cir Esp. 2020. https://doi.org/10.1016/j.ciresp.2020.08.001