Videothoracoscopic (VTC) resection of peripheral pulmonary nodules (PN) occasionally requires performing a mini-thoracotomy to locate them using palpation. The aim of this study is to evaluate the usefulness of inserting a CT-guided harpoon as a method for locating PN prior to surgery.
Material and methodsA study was conducted on a total of 52 patients who were scheduled for locating 55 PN prior to surgery by inserting a CT-guided harpoon, from November 2004 to January 2011.
ResultsOf the 52 patients, of whom 35 had a history of cancer, 31 were male and 21 were female, with ages between 28 and 84 years (mean: 62.2 years) with a PN <20mm (mean: 9.57mm). A total of 55 harpoons were inserted (3 patients had 2 simultaneous harpoons). Using the VTC it was observed that 52 harpoons were correctly anchored to the PN. There were no complications. In the group of 35 patients with an oncology history, the nodules were malignant in 26 cases (74.3%), and there were 17 (70.6%) with malignant PN in those with no oncology history. The hospital stay varied between 4 and 72h, with 19 patients (36.5%) included in a one-day surgery program.
ConclusionsThe preoperative identification of peripheral pulmonary nodules enables them to be removed directly with VTC. The insertion of a CT-guided harpoon in the PN is a safe and effective procedure that can be performed in a one-day surgery program.
La resección videotoracoscópica (VTC) de los nódulos pulmonares (NP) periféricos requiere en ocasiones la práctica de una minitoracotomía para su localización mediante palpación. El objetivo de este estudio es evaluar la eficacia como método de localización preoperatoria de los NP de la colocación de un arpón guiado por TAC.
Material y métodosDesde noviembre de 2004 hasta enero de 2011, 52 pacientes fueron programados para localización preoperatoria de 55 NP mediante la colocación de un arpón guiado por TAC.
ResultadosUn total de 52 pacientes (31 hombres y 21 mujeres) con edades entre 28 y 84 años (media: 62,2 años) con NP <20mm (media: 9,57mm). De ellos, 35 tenían historia oncológica. Se colocaron 55 arpones (a 3 pacientes, 2 arpones simultáneos). En la VTC, 52 arpones fueron hallados correctamente anclados al NP. No se observaron complicaciones. En el grupo de 35 pacientes con antecedentes oncológicos, los nódulos resultaron ser malignos en 26 (74,3%). En los 17 no oncológicos fueron malignos el 70,6%. La estancia hospitalaria osciló entre 4 y 72h, con 19 pacientes incluidos en un programa de cirugía ambulatoria (36,5%).
ConclusionesLa identificación preoperatoria de los NP permite su resección VTC directa. La colocación de un arpón guiado por TAC en los NP constituye un procedimiento seguro y efectivo que puede llevarse a cabo en un programa de cirugía ambulatoria.
When a patient presents with a radiological finding of a solitary pulmonary nodule (SPN), in most cases histological differentiation between malignancy and non-malignancy is necessary. The conventional procedures that are currently available for the histological diagnosis of SPN are: transthoracic fine-needle aspiration (FNA) or transbronchial biopsy. The effectiveness of both procedures can occasionally be limited by either an unfavorable position or the small size of the SPN. Furthermore, cytology is often not able to give a definitive diagnosis of non-malignancy.1
In the last 15 years, video-assisted thoracoscopic surgery (VATS) has become an essential tool for diagnosing and treating SPN.2,3 VATS is minimally invasive and provides complete resection of the nodule for histological analysis. Moreover, VATS resection may be an acceptable surgical option in patients with a primary pulmonary tumor and limited lung function.4 Nevertheless, the benefits of VATS could be affected by the inability to correctly locate the pulmonary nodules (PN) at the time of the procedure, which, according to some authors, occurs in 7.5%–11% of cases.5,6
This study was designed to evaluate the effectiveness of CT-guided hook wire localization of peripheral pulmonary lesions requiring VATS resection.
Materials and MethodsWe retrospectively analyzed 52 patients who had undergone VATS resections of SPN marked with CT-guided hook wires between November 2004 and January 2011 at the Hospital Universitari del Sagrat Cor (HUSC) and the Hospital Clinic (HC) in Barcelona. The project was approved by the Ethics Committees at both hospitals. All patients signed an informed consent to participate in the study.
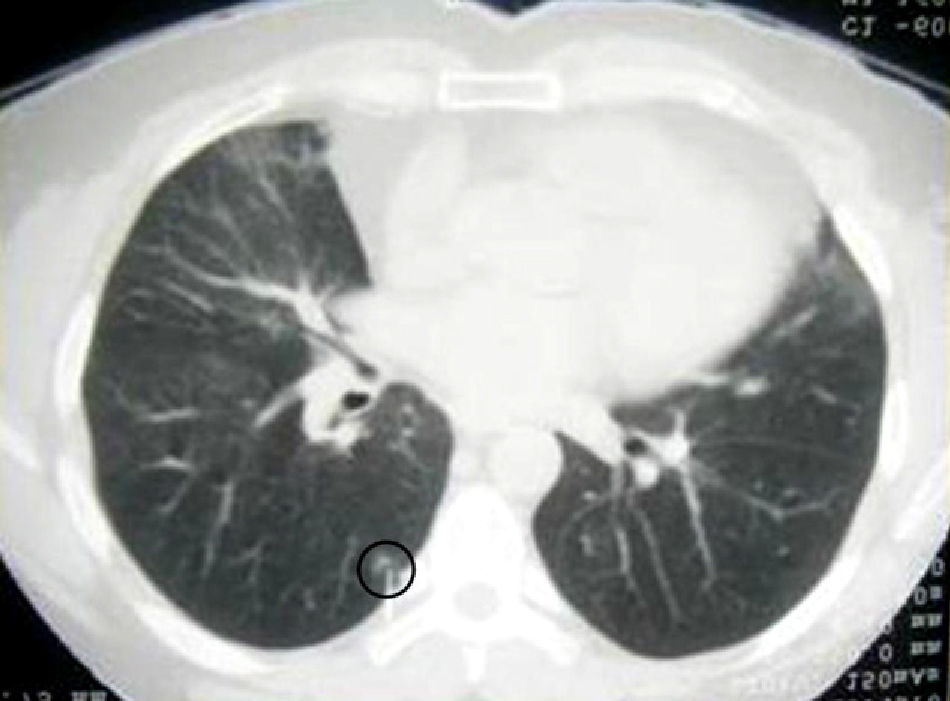
In the study, 2 CT models were used: the Philips Brilliance helical MDCT® (HUSC) and Siemens Somatom Emotion Duo® (HC). In all cases, axial cuts were performed with collimation 4mm×4.5mm, as is standard in conventional needle aspirations. These cuts are able to locate PN and also direct the placement of the hook wire either in the nodule or as close as possible. The interpretation of the results of the CT and the placement of the hook wires were performed by the same team of radiologists in each hospital.
On the day of surgery (just before the intervention) the patients were taken to the Diagnostic Radiology Unit and placed on the CT table, in the posterolateral thoracotomy position if possible. The placement of the CT-guided hook wire was carried out with local anesthesia with lidocaine and in sterile conditions.
The localization system used (except in the first 7 patients) was the Somatex Duo System® (Berlin, Germany), which was applied in 35 patients, and the Somatex Lung Marker System® (Berlin, Germany) in 10. The Duo System® was originally designed as a pre-operative marker for impalpable breast lesions, but it is also very appropriate for PN. We have been using this device in our patients with excellent results. The main advantages of this system are its flexibility, sharp tips (ideal for hard nodules) and arches, which avoid dislocation of the devices (we previously used a system without a hook shape). The Lung Marker System® is specifically designed for CT-guided marking of PN before VATS.7,8 It is a spiral-shaped wire whose shape provides reliable anchoring in the pulmonary parenchyma. We have used it successfully in 10 of our patients. In our experience, both marker systems have been shown to be safe and reliable.
These systems include 2 metallic needles: the first (introducer) needs to reach the lung lesion through the wall; when chest CT shows that the introducer is properly located (correct direction and proximity to the lesion), a second needle (with the hook wire) is introduced through the former and puts the arches in place (by precisely feeding them through the second needle) either close to or inside the lung nodule to be resected (Fig. 1). At that time, the needle is withdrawn and the proximal end of the hook wire is positioned on the skin covered by a dressing. The wire is left loose enough to be able to move with the lung collapse during surgery. At the end of the localization procedure, the patients are transferred to the operating room.
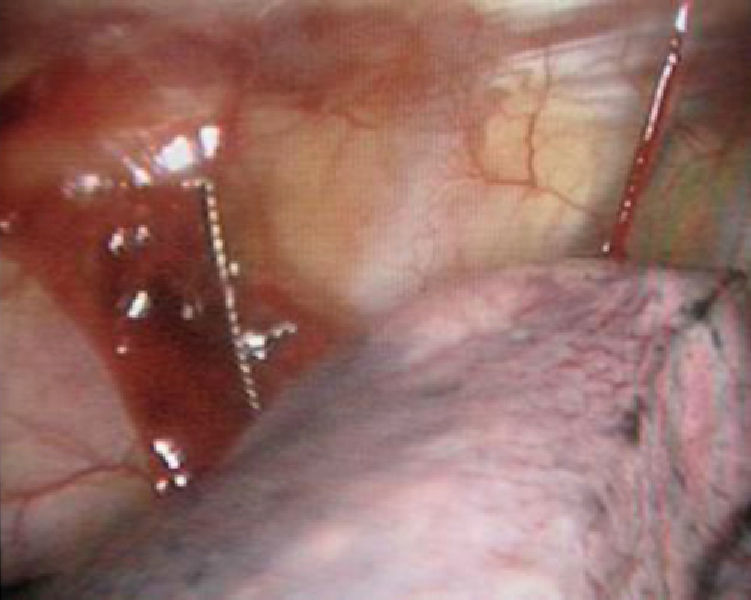
For our study, VATS surgery was done under general anesthesia using selective ventilation through a double-lumen endobronchial tube. The thoracoscope was inserted through a 10-mm entry port at the 7th intercostal space on the midaxillary line in most cases. Other intercostal incisions (12mm and 5mm) were made in order to visualize and manipulate the nodule. The collapsed lung parenchyma and the hook wire entering through the chest wall and anchored to the nodule were visible with the camera (Fig. 2). Partial resections were performed by VATS and all the samples were extracted through the 12mm port with a protective endobag. The surgical samples included PN with the anchored hook wire and significant parenchyma resection margins (Fig. 3). All the samples were analyzed intraoperatively by the pathologist using frozen sections. When the diagnosis was a benign nodule, metastatic disease and/or primary lung cancer in a patient with limited lung function and if the resection margins were reported to be correct, the resection was considered complete and the procedure was finished after systematic lymph node sampling. Finally, a chest drain tube was inserted. When the finding was primary bronchogenic carcinoma, the incision was converted to limited thoracotomy and the resection was completed (lobectomy).
The conversion to thoracotomy in these patients was considered a therapeutic necessity and not a failed VATS resection.
Results52 patients were included in the study (31 men and 21 women). Mean age was 62.2 (range 28–84). The nodules had a maximum diameter of 20mm (mean 9.57mm). Thirty-seven nodules were <10mm. In 6 patients, the nodule was detected during the staging of a recently diagnosed neoplasm, in 29 patients during the follow-up of a previously known neoplasm and in 17 patients there was no previous oncologic history. We placed 55 hook wires (in 3 patients, 2 hook wires were inserted simultaneously). The positioning of the hook wires was performed satisfactorily by the radiologists in the Diagnostic Radiology Unit in all cases. Fifty-two hook wires were found to be correctly anchored during the video-assisted exploration and 3 (5.4%) had become displaced. Pre-operative CT, performed immediately after the placement of the hook wire, showed minimal pneumothorax in 6 patients (11%). None of the patients presented significant symptoms and none required the insertion of a chest drain. VATS resection was performed in 50 out of the 52 patients without needing to extend the port of entry incisions. No other complications associated with the placement of the hook wire were observed (no bleeding or significant pneumothorax). Among the 35 patients with previous oncological history, the nodules were malignant in 26 cases (74.3%) (14 lung, 4 colon, 3 melanoma, 2 breast and one parotid, endometrial and urothelial); 9 nodules were benign (2 hamartomas, one adenomatous hyperplasia, one chronic pneumonia, one sarcoidosis, 3 inflammatory infiltrates and one intraparenchymal lymph node).
Among the 17 patients without oncologic history, there were 12 bronchogenic carcinomas (3 double) and 5 benign nodules (3 hamartomas, one tuberculous nodule and a fibrous nodule).
Hospital stay ranged between 4 and 72h, with 19 patients included in an outpatient surgery program (36.5%); 15 patients were discharged after 24h (28.8%), one after 72h due to persistent air leak (1.9%) and 17 after 5 days as they required additional lung resection.
DiscussionAdvances in thoracic surgery over the last 10 years have significantly widened the spectrum of thoracoscopy. Today, VATS is routinely used to diagnose and treat most pulmonary processes.2,3 SPN resection is the most common indication for VATS due to the fact that most pulmonary nodular lesions can be easily detected with inspection and tactile evaluation using endo instruments. Nevertheless, some SPN are difficult to identify with thoracoscopy. The small size of the nodule and/or the distance to the pleural surface could be limiting factors when performing adequate thoracoscopic resection.9 Pre-operative marking of an SPN is necessary in many occasions in order to carry out complete, safe exeresis with VATS.10,11
There are several varying techniques described in the literature for locating SPN: pre-operative injections of markers in the location where an SPN is situated (methylene blue,12 lipiodol13 or colored collagen14), radioguided surgery,15 intraoperative detection of the SPN with ultrasound16,17 and CT-guided placement of a metallic hook wire.7,8,18–20
The correct localization of SPN with the injection of methylene blue has a reported failure rate of approximately 13%, mainly due to excess liquid injected or a previous error in the localization of the nodule.12
The intraoperative detection of SPN with ultrasound requires a flexible ultrasound endoscope. This can be limited by the presence of air in the parenchyma, especially when complete lung collapse is not feasible.16 Despite the lack of complications and the high sensitivity and specificity seen with the use of ultrasound17 there have only been a few cases published in the literature. The technique has also presented important limitations in the localization of inflammatory nodules.19
Palpation (digital or endo instrumental) through entry port incisions has been the most commonly used method for locating SPN in VATS. Nonetheless, it has been seen that this practice is effective only when the nodule is superficial or is >2cm.1
Since November 2004, we have been using CT-guided placement of hook wires to pre-operatively locate those peripheral PN that we have considered difficult to palpate. Our SPN study protocol also includes transbronchial pulmonary biopsy and/or CT-guided fine-needle transthoracic biopsy. We perform biopsy with VATS only when less invasive conventional procedures have not been able to provide a diagnosis or when they were not indicated.
Marking nodules with hook wires has significantly simplified our surgical approach for small and indeterminate SPN. The physical proximity of the Diagnostic Radiology Unit to the operating room and the possibility to carry out the procedure just before surgery has made this technique a safe, fast procedure in our experience. In our series, pneumothorax occurred after the placement of the hook wire in 6/52 patients (11.5%). These pneumothoraxes were minimal and were not clinically significant; therefore, thoracic drain tubes were not necessary and the patients were able to be transferred to surgery without problems. The risk of the hook wire accidentally being displaced was reduced by properly positioning the patients on the surgical table and by maintaining an adequate length of wire cable outside the thorax, thus allowing the wire to “follow” the collapsed parenchyma during selective ventilation. Despite these precautions, we had a displaced hook wire rate of 5.4% (3/55 wires), 2 of which were due to a different hook wire type (used at the beginning of the study) when the SPN markers were neither Somatex Duo System® (Berlin, Germany) nor Somatex Lung Marker System® (Berlin, Germany). Both systems have provided excellent results (no other cases of accidental displacement occurred after the initial 3 cases).
In any event, our rate of accidental displacement (5.4%) is acceptable and consistent with the percentage of 8% published in the literature21 and much lower than the 47% failure rate due to accidental displacement, erroneous localization of the nodule or significant subpleural hematoma published by Bernard in a multicentric study.3 In all these cases, thoracoscopic resection was still possible in spite of the accidental displacement because the hematoma left on the pleural surface allowed us to locate the nodule without any difficulty. Due to this reason, we do not think that the injection of methylene blue is required as a complement to hook wire marking.
There have been isolated reports of pulmonary air embolism during hook wire localization.22 In our experience, we have found no evidence of this complication.
The size of the nodule, and the distance from the pleural surface have been considered the most important parameters for adequate identification in VATS.9 The main difficulties published in the bibliography make reference to a size smaller than 10mm and/or a distance from the pleural surface of between 5 and 15mm.2,9,21 With the placement of the hook wire, we surpassed these limitations and it was not necessary to convert to standard thoracotomy at any time because of difficulties locating the PN.
Despite the fact that the placement of CT-guided hook wires is an additional cost to the resection of SPN, this is compensated by the savings in hospital costs. The hook wire makes safe, immediate surgical resection possible while avoiding thoracotomy, which shortens surgical time and hospital stay. When patients are prepared in the Diagnostic Radiology Unit (while the previous intervention is going on simultaneously), there is a saving in both cost and operating room time.
In summary, it is a fact that spiral CT makes it possible to detect PN that would not be visible with traditional CT. This leads to a significant increase in the number of PN detected. Whenever the diagnosis of a pulmonary nodule cannot be made with less invasive techniques such as transbronchial biopsy and/or CT-guided fine-needle aspiration, VATS should be considered both as a diagnostic as well as a therapeutic procedure. The pre-operative evaluation of PN with chest CT is important to define the indication of surgical resection and to select those patients who could benefit from pre-operative localization. The localization of PN with hook wires could be a very effective tool with minimal complications and a high success rate. The procedure should be carried out just before surgery, requiring the close cooperation of radiologists, pathologists and surgeons. In expert hands, it is a safe and effective procedure.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Molins L, et al. Localización de nódulos pulmonares con arpón guiado por tomografía axial computarizada previa a la resección videotoracoscópica. Experiencia en 52 casos. Cir Esp. 2013;91:184–8.