Radical hysterectomy is the standard treatment for patients with early-stage cervical cancer. However, for women who wish to preserve fertility, radical trachelectomy is a safe and viable option.
ObjectiveTo present the first case of laparoscopic radical trachelectomy performed in the National Cancer Institute, and published in Mexico.
Clinical casePatient, 34 years old, gravid 1, caesarean 1, stage IB1 cervical cancer, squamous, wishing to preserve fertility. She underwent a laparoscopic radical trachelectomy and bilateral dissection of the pelvic lymph nodes. Operation time was 330min, and the estimated blood loss was 100ml. There were no intraoperative or postoperative complications. The final pathology reported a tumour of 15mm with infiltration of 7mm, surgical margins without injury, and pelvic nodes without tumour. After a 12 month follow-up, the patient is having regular periods, but has not yet tried to get pregnant. No evidence of recurrence.
ConclusionsLaparoscopic radical trachelectomy and bilateral pelvic lymphadenectomy is a safe alternative in young patients who wish to preserve fertility with early stage cervical cancer.
La histerectomía radical es el tratamiento estándar para los pacientes con cáncer de cérvix en etapa temprana; sin embargo, para las mujeres que desean preservar la fertilidad, la traquelectomía radical es una opción segura y viable.
ObjetivoPresentar el primer caso de una traquelectomía radical por laparoscopia, realizada en el Instituto Nacional de Cancerología y publicado en México.
Caso clínicoPaciente de 34 años, una gestación y una cesárea, con cáncer de cérvix etapa IB1, epidermoide, que deseaba preservar la fertilidad. Se sometió a una traquelectomía radical laparoscópica y a disección bilateral de los ganglios linfáticos pélvicos. El tiempo operatorio fue de 330min, y la pérdida de sangre estimada fue 100ml; no se presentaron complicaciones intra o postoperatorias. La patología final reportó un tumour de 15×7mm de infiltración lo que corresponde a menos del 50% del estroma cervical, los bordes quirúrgicos sin lesión, ganglios pélvicos sin tumour. A 12 meses de seguimiento, la paciente está presentando menstruaciones regulares, pero aún no se ha tratado de embarazar. No hay evidencia de recurrencia.
ConclusionesLa traquelectomía radical laparoscópica con linfadenectomía pélvica bilateral es una alternativa segura en pacientes jóvenes que desean preservar la fertilidad con cáncer de cérvix etapa temprana.
Cervical cancer is the second most widespread cancer in women in developing countries and the seventh in developed countries.1 it has been estimated that approximately 500,000 new cases of invasive cancer will be diagnosed throughout the world every year. Due to the effective use of appropriate detection of cervical cancer, many women will be diagnosed at a relatively young age and at an early stage.2
The standard treatment for patients with early-stage cervical cancer (IA2 and IB1) is radical hysterectomy. However, for those women who wish to preserve future fertility, radical trachelectomy is now considered a safe and feasible option.3 The procedure may be performed using a vaginal and/or abdominal approach, with comparable oncologic outcomes.4 The first laparoscopic radical trachelectomy was performed by Lee et al.5 and since then other researchers have published their experience with this procedure.6–16
Laparoscopic trachelectomy may be performed using a robotic platform whenever available, with few reported cases in literature to date.17,18
We present the case of a patient upon whom laparoscopic radical trachelectomy was performed and we review the outcome of similar procedures published in the literature.
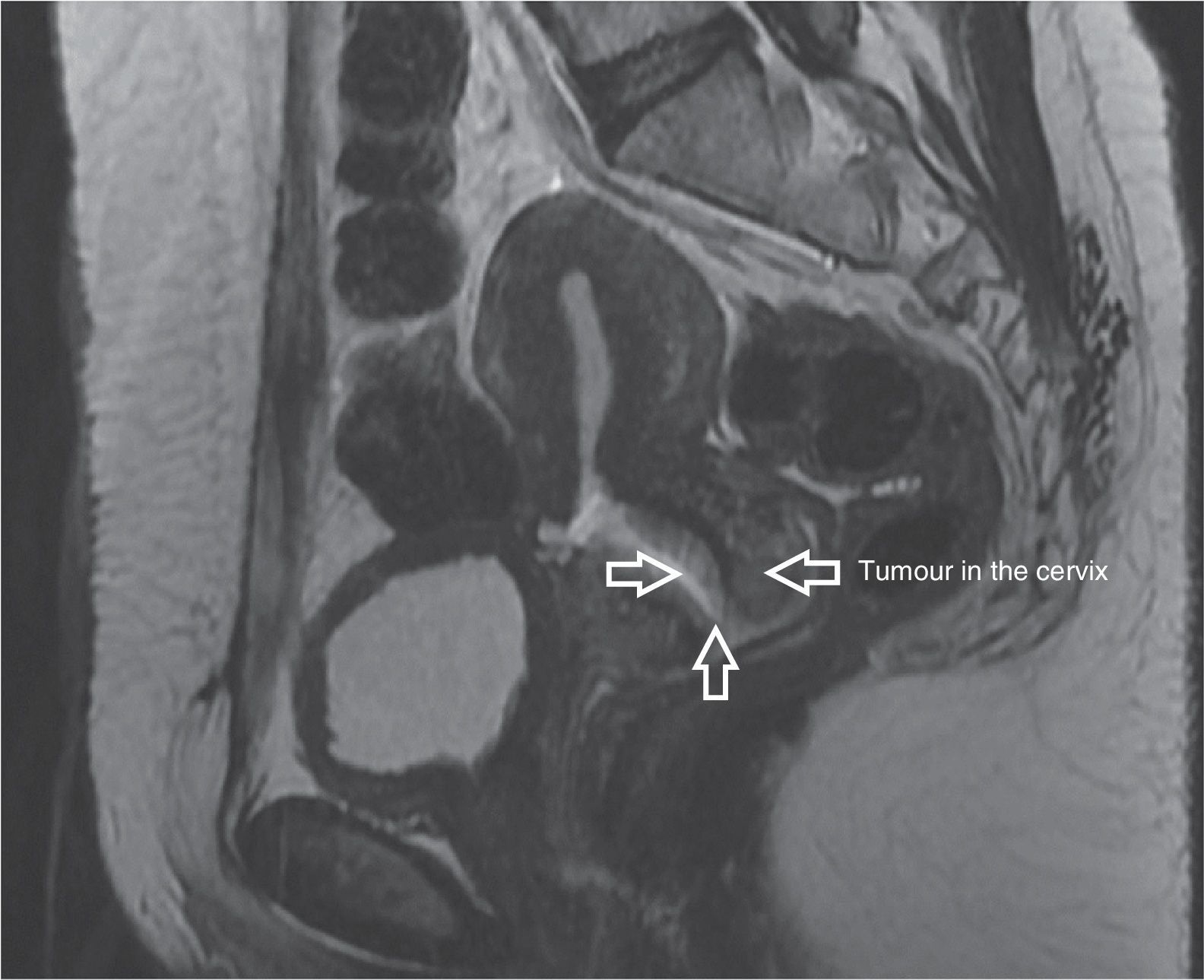
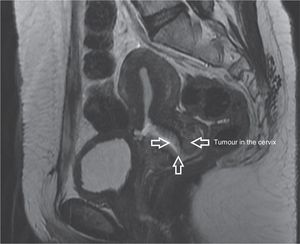
Clinical caseA female patient aged 34, who had had a baby by caesarean section, had been diagnosed with cervical cancer and was assessed for the first time in the National Cancer Institute in March 2013. A physical examination showed a body mass index of 27.8kg/m2, a cervix of 3cm diameter with a 2cm×2cm ulcerated and indurated central tumour towards the anterior cervical lip and with no changes to the parametria and vaginal fornix. A biopsy of the cervix reported invasive moderately differentiated epidermoid carcinoma. Stage IB1 (2cm×2cm) cervical cancer was diagnosed. NMR imaging of the pelvis was performed which showed a 6cm×6mm poorly delineated tumour with irregular edges, with heterogeneous enhancement of tumour and no sign of enlarged pelvic lymph nodes, or suspected malignancy (Fig. 1). The patient wished to preserve fertility and was referred for laparoscopic radical trachelectomy and bilateral dissection of the pelvic lymph nodes, which was carried out in April 2013 under general anaesthesia, in the Trendelenburg position. The surgical procedure commenced with the insertion of a VCare® UterineManipulator/Elevator (ConMedEndosurgery, Utica, NY, USA) into the uterus. Following this, a 10mm supraumbilical incision was made, the trocar was inserted under direct view with Endopath Bladeless Trocarendopath Optiview Optical Obturator (Ethicon) up to the abdominal cavity, and this was inflated with CO2 to a maximum pressure of 15mmHg. 4 auxiliary (Ethicon) trocars were used, 2 5mm trocars, one to the right and the other to the left in the lower quadrants, respectively and 2 5mm trocars positioned to the right and left of the flanks at the level of the umbilicus, respectively. The abdominal cavity was examined and afterwards an incision of the broad ligament was made, in a triangle formed by the round ligament, the psoas major muscle and the infundibulopelivc ligament, making the incision parallel to the latter. This was achieved by placing the uterus in counterweight to the incision and the placing upwards pressure on the round ligament, dissecting paravesical and pararectal retroperitoneal spaces, then the rectovaginal space and dissecting the vesicovaginal tissues. The round ligaments and both ovaries with their infundibulopelivc ligament were preserved. Examination was made of the pelvic lymph nodes, with no sign of suspected malignancy, and we therefore proceeded in identifying the uterine arteries, which were coagulated and cut at the hypogastric artery emergency level. Parametrial tissues were resected up to the pelvic wall using bipolar laparoscopic LigaSure™ energy (5mm blunttip, Covidien). The ureters were released from the neighbouring peritoneal and parametrial tissues. The bladder was dissected exposing the bladder pillars, which were coagulated and resected at the posterior wall of the bladder. The collateral vaginal vessels in their upper third area were resected with bipolar energy and the vaginal vessels in the lower third area were preserved. The vagina was resected 1cm below the cervix with a monopolar (Karl Storz) clamp, and pressure was later placed vaginally downwards on the uterus, cervix and parametria with the loose vaginal area. The cervix was section at 1cm below the isthmus with a monopolar electrosurgical pencil through the vagina. The specimen, including cervix, bilateral parametria and the upper virginal margin was removed through the vagina.
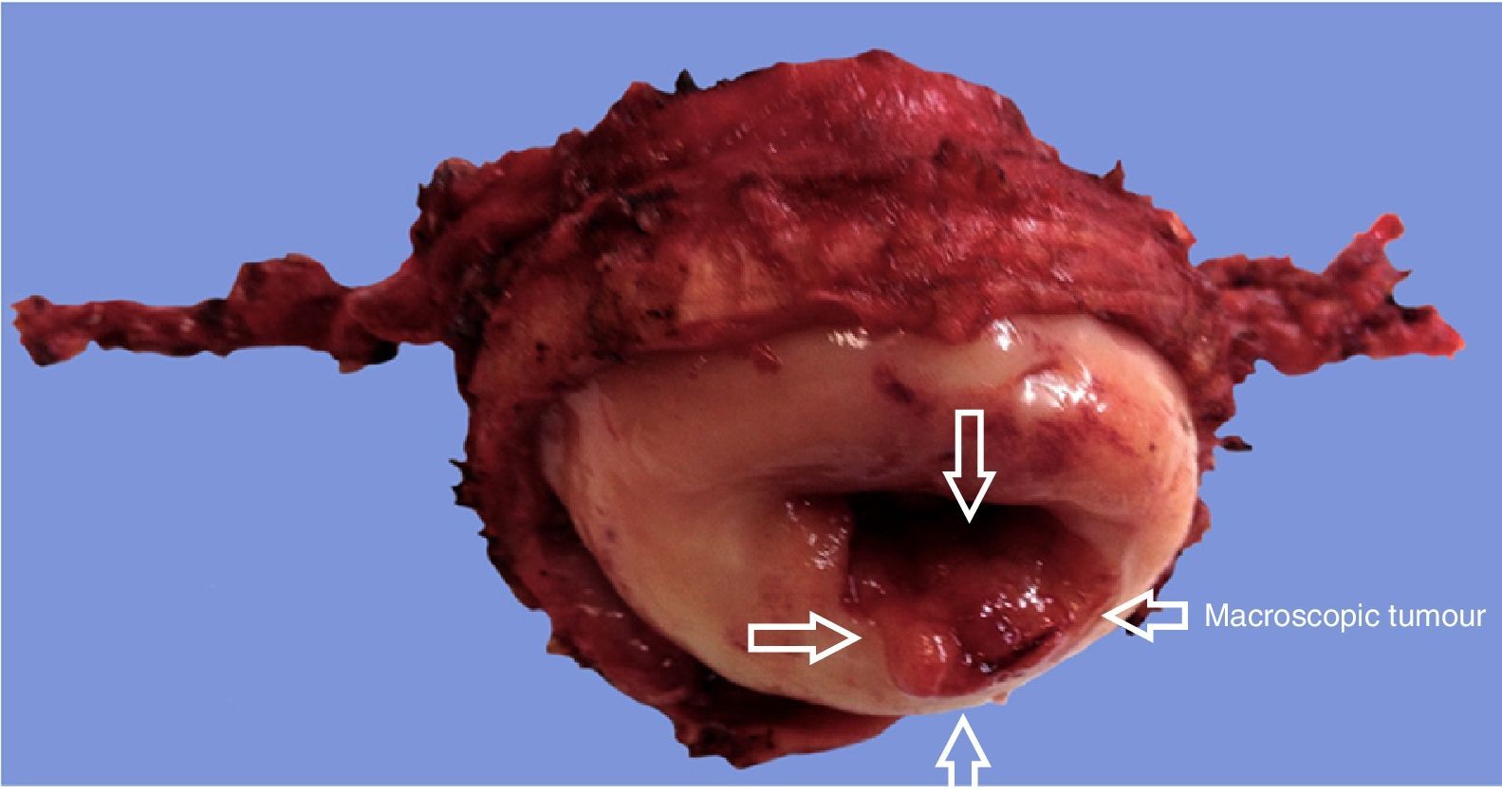
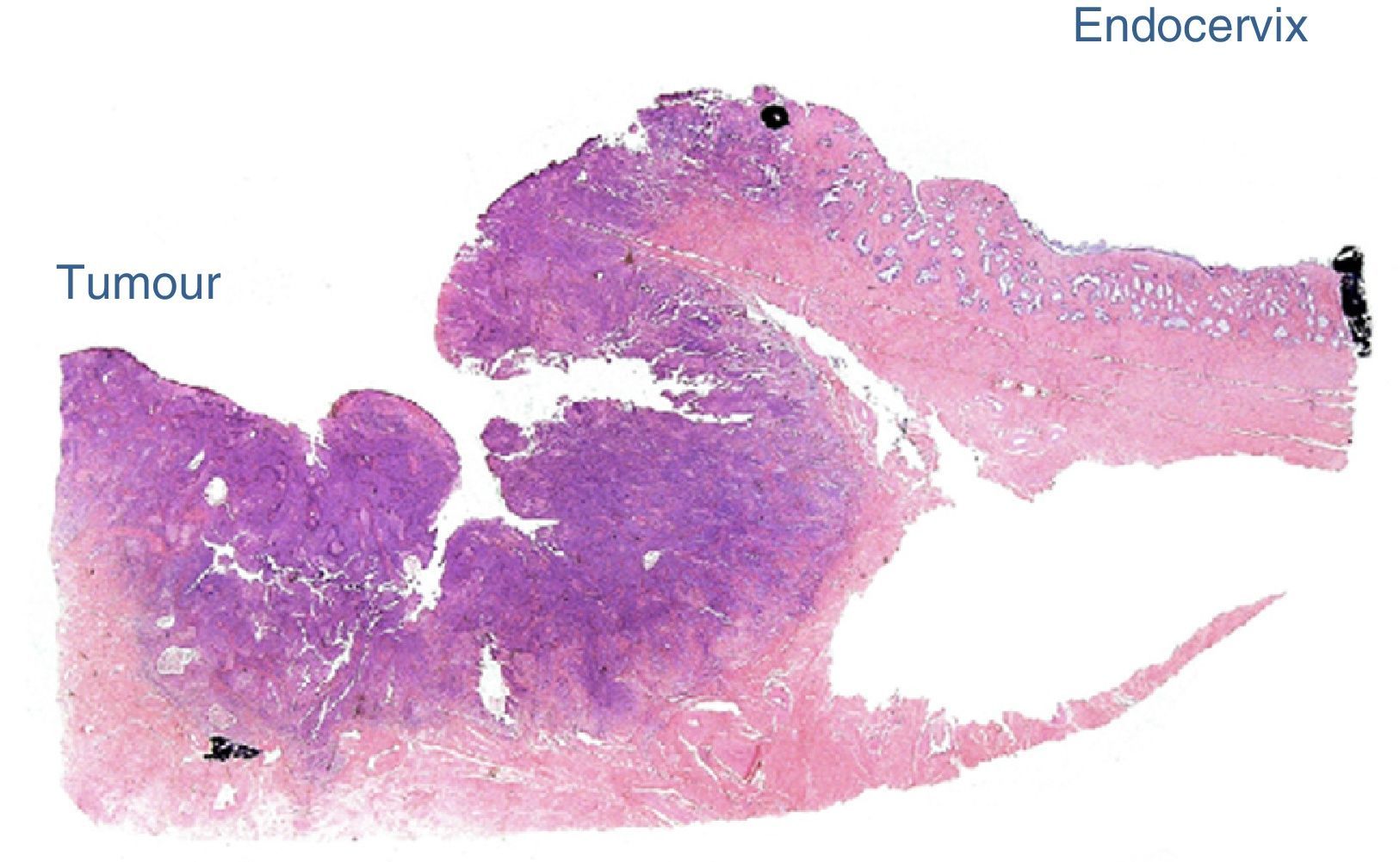
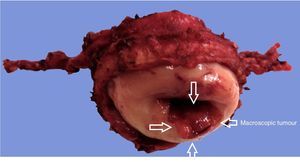
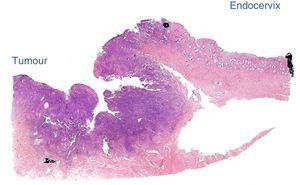
The intraoperative frozen section analysis reported free margins (Fig. 2). Bilateral pelvic lymphadenectomy was later performed of common iliac, external and hypogastric vessels and of the obturator fossa, with conventional limits, and tissue was removed vaginally. The edge of the uterine body was sutured to the proximal vaginal edge with simple suture using 8 individual 2-0 poliglactine (Vicryl) sutures. This was performed with a vaginal approach. No cervical cerclage was carried out (this will be performed when the patient is pregnant). A Foley catheter (8 French) was inserted vaginally in the endometrial canal and left in place for 7–10 days, to reduce stenosis of the residual cervix, and was then removed. The operation time was 330min. Estimated blood loss was 100ml. There were no interoperative or postoperative complications. The patient was discharged from hospital the second day after surgery. The intravesical Foley catheter was removed on day two, and urination was spontaneous thereafter.
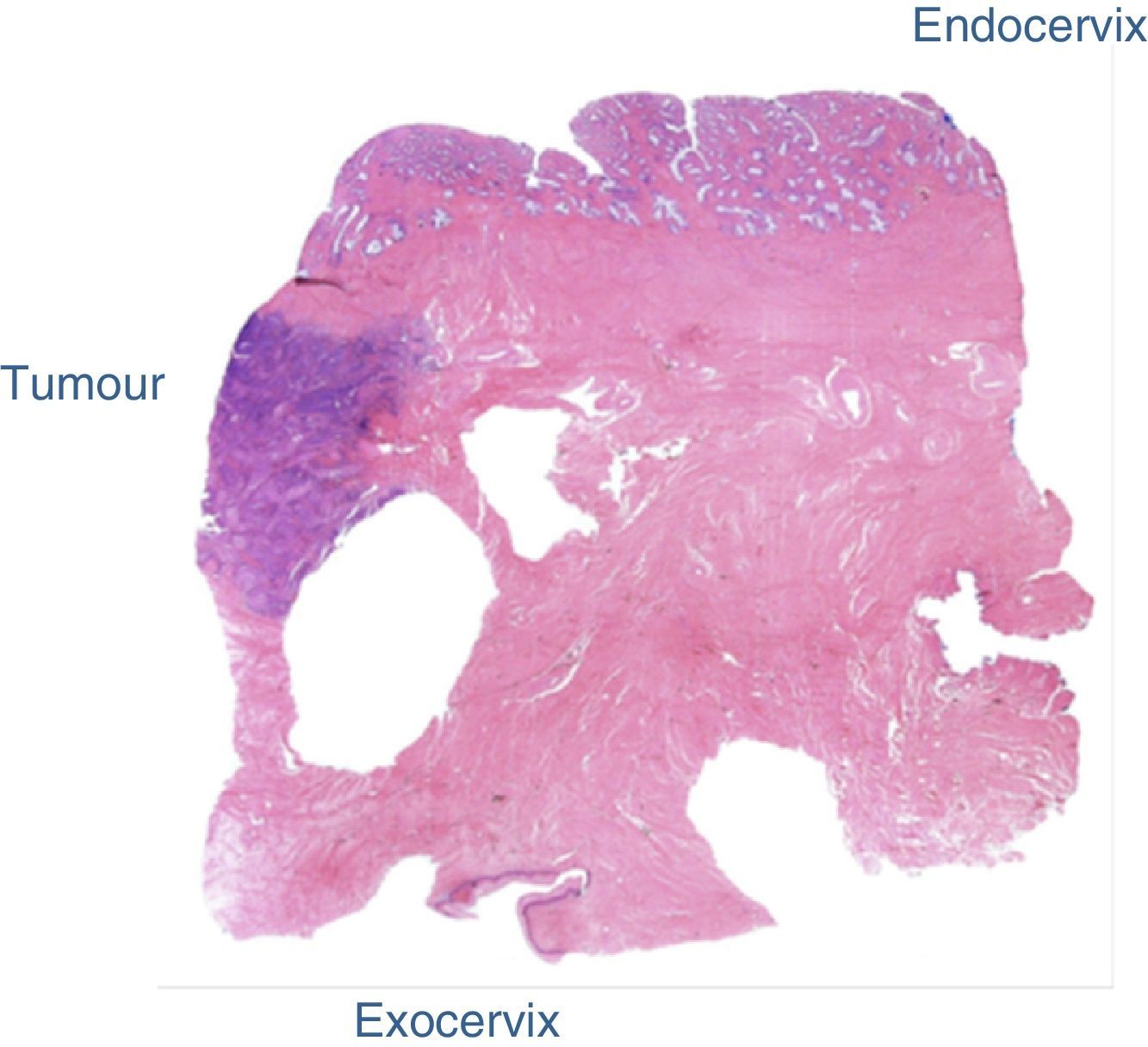
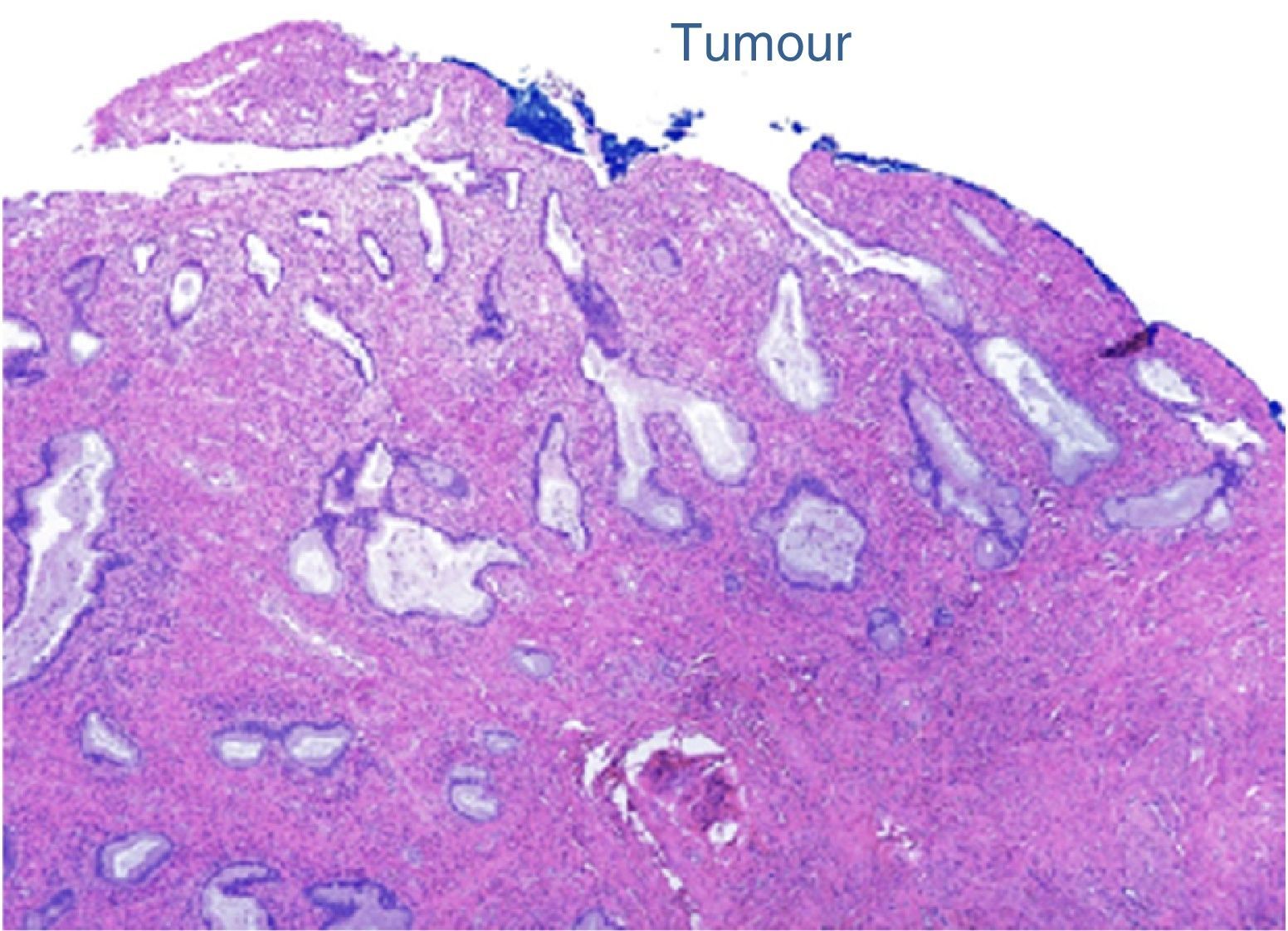
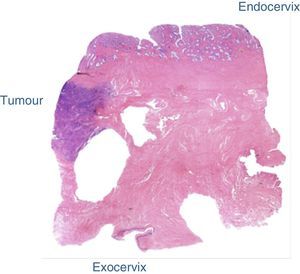
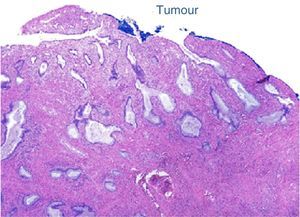
The final laboratory analysis reported: posterior cervical lip with invasive moderately differentiated carcinoma of the cervix of 15mm on the long axis, 7mm invasion to the stroma in a 19mm thick wall (<50%) with no sign of lymphovascular invasion, surgical site edges free from neoplasia (envocervical edge to 12mm of neoplastic cells), both parametrias free from neoplasia, 3 out of 3 internal iliac lymph nodes, 6 out of 6 external iliac lymph nodes and 3 out of 3 obturator lymph nodes free from neoplasia (Figs. 2–5).
After 20 months of follow-up the patient presented with regular menstruations, colposcopic and vaginal smears were made, both without any signs of disease. The patient wishes to become pregnant and her gynaecological and obstetric assessment and follow-up are being carried out in the National Institute of Perinatology.
DiscussionThe main selection criteria for undertaking a radical trachelectomy is the wish to preserve fertility. The preservation of the uterus in women who are not planning to become pregnant or with prior alternations to fertility is under dispute.19,20
Tumour size is the most important risk factor in recurrence, and in different studies it has been demonstrated that the risk of recurrence20,21 greatly increases with tumours over 2cm. In our case tumour size was under 2cm and we therefore considered this as a criterion for the inclusion of the procedure.
The histopathology examination is important for determining the type, stage, tumour size, depth of invasion and extension of the lymphovascular space.
Magnetic resonance imaging is the ideal method of preoperative assessment, for determination of the exact tumour size, the extension of infiltration of the cervical stroma and the amount of healthy stroma which has been preserved (determination of tumour growth in three dimensions); information may be even greater with the use of a endovaginal setting coil22–24 or the creation of an artificial saline hydrocolpos.25 We performed nuclear magnetic resonance on our patient and all patients were candidates for radical management to preserve fertility.
Several authors showed that invasion of less than half of the cervical stroma is the limit for undertaking a safe trachelectomy, because a free margin of 1cm is required,26–28 and margins of 5–8mm is sufficient, but this is still as yet disputable.29 All trachelectomy approaches must retain a good proportion of healthy stoma since the probability of a successful pregnancy is greater.
The suggested eligibility criteria for radical trachelectomy are: the wish to preserve fertility, confirmation of cervical cancer, invasive epidermoid cancer, adenocarcinoma, or squamous adenocarcionoma, tumour size under 2cm, FIGO IA1 state with invasion of lymphovascular space, IA2 and IB1, tumour limited to cervix and confirmed by preoperative nuclear magnetic resonance, aged ≤40, no sign of metastasis in the pelvic lymphatic nodes, that no anterior infertility has been documented. In institutions they consider the on exclusion of patients aged >40 or body mass index as the only factor not associated with infertility.30
It has been estimated that with careful selection of patients for conservative fertility surgery, for 12–17% of patients, the procedure will be cancelled due to the lymph node metastasis or the positive endocervical margin.19
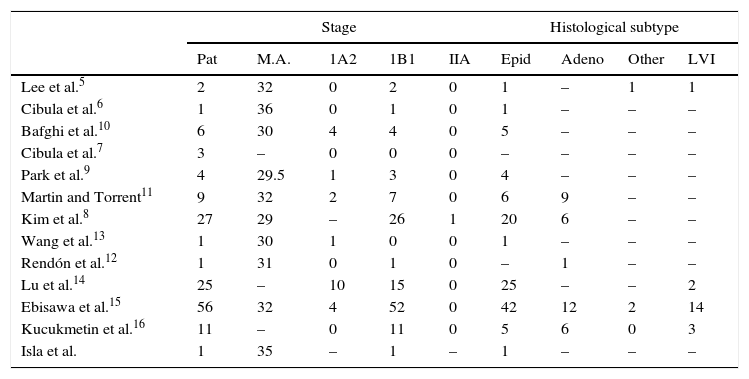
A review of 12 reported articles up to 2014 was made, which included this report, with 146 cases in total, on whom laparoscopic radical trachelectomy had been performed. This is summarised in Tables 1–3.
Clinical and pathological data of reports on laparoscopic radical trachelectomy.
| Stage | Histological subtype | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Pat | M.A. | 1A2 | 1B1 | IIA | Epid | Adeno | Other | LVI | |
| Lee et al.5 | 2 | 32 | 0 | 2 | 0 | 1 | – | 1 | 1 |
| Cibula et al.6 | 1 | 36 | 0 | 1 | 0 | 1 | – | – | – |
| Bafghi et al.10 | 6 | 30 | 4 | 4 | 0 | 5 | – | – | – |
| Cibula et al.7 | 3 | – | 0 | 0 | 0 | – | – | – | – |
| Park et al.9 | 4 | 29.5 | 1 | 3 | 0 | 4 | – | – | – |
| Martin and Torrent11 | 9 | 32 | 2 | 7 | 0 | 6 | 9 | – | – |
| Kim et al.8 | 27 | 29 | – | 26 | 1 | 20 | 6 | – | – |
| Wang et al.13 | 1 | 30 | 1 | 0 | 0 | 1 | – | – | – |
| Rendón et al.12 | 1 | 31 | 0 | 1 | 0 | – | 1 | – | – |
| Lu et al.14 | 25 | – | 10 | 15 | 0 | 25 | – | – | 2 |
| Ebisawa et al.15 | 56 | 32 | 4 | 52 | 0 | 42 | 12 | 2 | 14 |
| Kucukmetin et al.16 | 11 | – | 0 | 11 | 0 | 5 | 6 | 0 | 3 |
| Isla et al. | 1 | 35 | – | 1 | – | 1 | – | – | – |
Adeno: adenocarcinoma; M.A: mean age; Epid: epidermoid; Pat: patients; LVI: lymphovascular invasion.
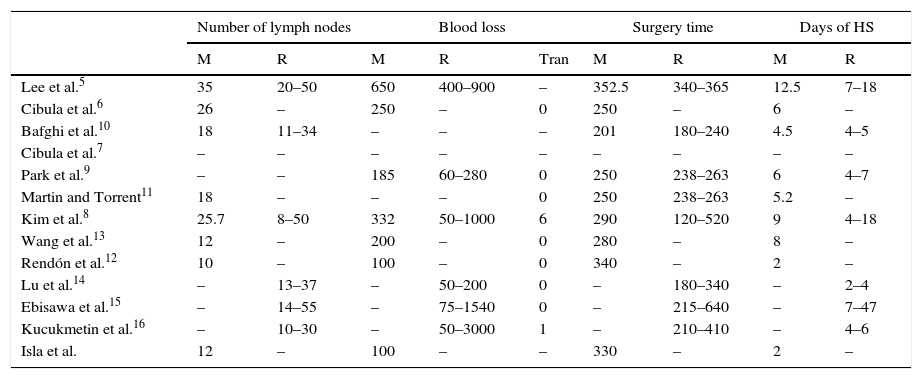
Description of surgical information of the radical laparoscopic trachelectomy series.
| Number of lymph nodes | Blood loss | Surgery time | Days of HS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M | R | M | R | Tran | M | R | M | R | |
| Lee et al.5 | 35 | 20–50 | 650 | 400–900 | – | 352.5 | 340–365 | 12.5 | 7–18 |
| Cibula et al.6 | 26 | – | 250 | – | 0 | 250 | – | 6 | – |
| Bafghi et al.10 | 18 | 11–34 | – | – | – | 201 | 180–240 | 4.5 | 4–5 |
| Cibula et al.7 | – | – | – | – | – | – | – | – | – |
| Park et al.9 | – | – | 185 | 60–280 | 0 | 250 | 238–263 | 6 | 4–7 |
| Martin and Torrent11 | 18 | – | – | – | 0 | 250 | 238–263 | 5.2 | – |
| Kim et al.8 | 25.7 | 8–50 | 332 | 50–1000 | 6 | 290 | 120–520 | 9 | 4–18 |
| Wang et al.13 | 12 | – | 200 | – | 0 | 280 | – | 8 | – |
| Rendón et al.12 | 10 | – | 100 | – | 0 | 340 | – | 2 | – |
| Lu et al.14 | – | 13–37 | – | 50–200 | 0 | – | 180–340 | – | 2–4 |
| Ebisawa et al.15 | – | 14–55 | – | 75–1540 | 0 | – | 215–640 | – | 7–47 |
| Kucukmetin et al.16 | – | 10–30 | – | 50–3000 | 1 | – | 210–410 | – | 4–6 |
| Isla et al. | 12 | – | 100 | – | – | 330 | – | 2 | – |
HS: hospital stay; M: mean; R: range; Tran: transfusion.
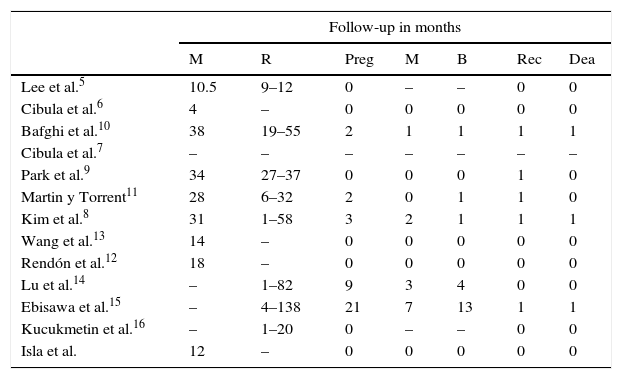
Postoperative and follow-up data of the laparoscopic radical trachelectomy series.
| Follow-up in months | |||||||
|---|---|---|---|---|---|---|---|
| M | R | Preg | M | B | Rec | Dea | |
| Lee et al.5 | 10.5 | 9–12 | 0 | – | – | 0 | 0 |
| Cibula et al.6 | 4 | – | 0 | 0 | 0 | 0 | 0 |
| Bafghi et al.10 | 38 | 19–55 | 2 | 1 | 1 | 1 | 1 |
| Cibula et al.7 | – | – | – | – | – | – | – |
| Park et al.9 | 34 | 27–37 | 0 | 0 | 0 | 1 | 0 |
| Martin y Torrent11 | 28 | 6–32 | 2 | 0 | 1 | 1 | 0 |
| Kim et al.8 | 31 | 1–58 | 3 | 2 | 1 | 1 | 1 |
| Wang et al.13 | 14 | – | 0 | 0 | 0 | 0 | 0 |
| Rendón et al.12 | 18 | – | 0 | 0 | 0 | 0 | 0 |
| Lu et al.14 | – | 1–82 | 9 | 3 | 4 | 0 | 0 |
| Ebisawa et al.15 | – | 4–138 | 21 | 7 | 13 | 1 | 1 |
| Kucukmetin et al.16 | – | 1–20 | 0 | – | – | 0 | 0 |
| Isla et al. | 12 | – | 0 | 0 | 0 | 0 | 0 |
M.: miscarriage; Dea: deaths; Preg: pregancies; M: mean; B: birth; R: range; Rec: recurrence.
Lee et al.5 reported 2 cases, with operation times of 340min, where there were no complications during surgery, with blood loos of between 900 and 400ml, hospital stay of 18 and 7 days respectively. The number of pelvic lymph nodes was 20 and 50 respectively, both without tumour, the 2 patients were menstruating regularly and there was no evidence of recurrence at 12 and 9 months.5
Cibula et al.6 reported a case of laparoscopic radical trachelectomy with an operating time of 250min, with blood loss of 250ml, where there were no complications during the procedure nor during the postoperative period. The Foley catheter was removed after 7 days, the hospital stay was for 6 days. The pathology report was: 25mm vaginal cuff and negative margin, negative parametrias, uterine cervix with no residual invasive cancer, with stage III intraepithelial neoplasia in the endocervical canal with free margins and 26 negative lymph nodes. Follow up was for 4 months. The same group posterior published 3 additional cases.7 Average operating time was 210min (range was: 200–250min), average blood loss was 400ml (range was: 350–700), the mean number of pelvic lymph nodes was 24 (range was 22–29) and hospital stay was 3 days in all cases. No recurrence was reported during follow-up.
In 2006 Bafghi et al.10 reported 6 cases of laparoscopic radical trachelectomy. Average operating time was 201min (range was: 180–240), and median of lymph nodes was 18 (range was: 11–34). No complications arose, hospital stay averaged 4.5 days. One patient received adjuvant chemotherapy and radiotherapy and brachytherapy due to extensive invasion of the lymphatic and vascular cavity. 15 months after surgery this patient presented with recurrence and later died of disseminated disease. Two patients became pregnant. One patient had a miscarriage after 7 weeks and the other had a caesarean section after 35 weeks of pregnancy and gave birth to a healthy baby.
In 2009 Park et al.9 described 4 patients with early stage cervical cancer (one with stage IA2 and 3 with stage IB1) who underwent laparoscopic radical trachelectomy. Mean operating time and blood loss was 250min and 185ml, respectively. Anatomopatholgic diagnosis was squamous cell carcinoma in all cases and there was no lymph node metastasis. Mean follow-up was 34 months. Only one patient received concomitant chemo and radiotherapy due to recurrence.
Kimet al.8 in a total of 27 patients on whom trachelectomy was performed, obtained a mean operating time of 290min (range was: 120–520). The estimated blood loss was 332ml (range was: 50–1000) and perioperative transfusion was required in 6 patients (22.2%), and the mean transfusion volume was 2.2 units (range was: 2–3). There were no complications during the procedure or the postoperative procedures. The mean postoperative hospital stay was 9 days (range was: 4–18). Mean follow-up time was 31 months (range was: 1–58). Of the 27 patients who completed the laparoscopic radical trachelectomy, only one received adjutant therapy with paclitaxel and cisplantin. One patient presented with recurrence 8 months after surgery and died 4 months later from disease. A total of 6 patients tried to get pregnant and 3 were able to do so. Of these, 2 had miscarriages during the first three months, and the third patient had a caesarean section after 36 weeks of pregnancy.8
Martin and Torrent11 reported on 9 cases of laparoscopic radical trachelectomy with preservation of the hypogastric nerve. Average operating time was 270min and no complications were reported during surgery or the postoperative period; one patient required adjuvant chemo and radiotherapy. Two patients became pregnant, one of them until full term and the other was pregnant at the time of publication. During an average follow-up of 28 months one patient presented with recurrence, which was treated with chemo/radiotherapy.
Wang et al.13 published one case with preservation of the ascending branch of the uterine artery, where surgery lasted 280min and blood loss was 200cm3. There were no complications during surgery or postoperatively. The patient was disease free 14 months after surgery.
Rendón et al.12 reported one case of laparoscopic abdominal radical trachelectomy, with an operating time of 340min, and estimated blood loss of 100ml. There were no complications during the procedure or during the postoperative period. Hospital stay was 2 days and the pathology report showed: 10 negative lymph nodes, negative margins and parametrias, uterine neck with no invasive residual cancer and with adenocarcinoma in situ with free margins. Follow-up was 18 months without recurrence.
Lu et al.14 published the results obtained from 25 patients who underwent laparoscopic radical trachelectomy, with an average operating time of 232min, and average blood loss of 120ml, hospital stay on average of 3.3 days, with no presentation of complications during surgery and only 3 patients who presented with any postoperative complications, with an average follow-up of 66 months and no recurrences. 12 patients tried to become pregnant and 9 were able to do so. Three had miscarriages during the first three months, one a caesarean at 29 weeks due to ovular membrane rupture. 3 patients chose to have a caesarean at 37 weeks and the other 2 were pregnant at the time of publication.
Ebisawa et al.15 published the most extensive series involving 56 patients who underwent laparoscopic radical trachelectomy. Operating time was 349min, with average blood loss of 300ml; there were 2 vascular lesions which were repaired by laparoscopy, the average number of lymph nodes obtained was 32, average hospital stay was 17 days. Regarding the obstetric outcome: 25 women tried to get pregnant and there were 21 pregnancies in 13 women. Five had miscarriages during the first three months, 2 in the second three months, and 13 women had their babies by caesarean section. One patient was pregnant at the time of publication.
Kucukmetin et al.16 published a study of 27 women, which compared laparoscopic radical trachelectomy and open radical trachelectomy for the preservation of fertility in women with stage lB1 cervical cancer. Laparoscopic radical trachelectomy was performed on 11 (40.8%) women, whilst 16 (59.2%) were referred for radical open trachelectomy. Average blood loss and hospital stay were significantly reduced in the laparoscopic radical trachelectomy group (85 compared with 800ml, p<0.001, and 4 compared with 7 day, p=0.003). The average operating time was greater with the laparoscopic approach (320 compared with 192.5min, p<0.001). This study showed that laparoscopy had better results regarding blood loss and the duration of hospital stay.
ConclusionLaparoscopy has become an increasingly more frequently used tool in gynaecological oncology and in young patients who wish to preserve fertility. Laparoscopic radical trachelectomy with pelvic lymphadenectomy is an alternative technique in the treatment of uterine neck cancer in early stages, with the same oncologic outcome and appropriate obstetric outcome, but with the benefits of minimal invasion surgery: less bleeding, shorter hospital stay and better postoperative recovery compared with open surgery. Although follow-up times are still short, it is expected that the obstetric outcome and the oncologic outcome long term will not be overly different to its vaginal or abdominal counterpart.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Isla Ortiz D, Montalvo-Esquivel G, Chanona-Vilchis JG, Herrera Gómez Á, Ñamendys Silva SA, Pareja Franco LR. Traquelectomía radical laparoscópica para preservación de la fertilidad en cáncer de cérvix etapa temprana. Reporte de un caso. Cirugía y Cirujanos. 2016;84:329–335.