Introduction
Clinical communication currently represents a fundamental aspect of medical care, not only within the setting of primary care but also in any clinical specialty. Communication is precisely the channel through which care is provided, and many well-designed studies have shown effective clinical communication to favor the processes of diagnosis and therapy.1 To achieve and maintain effective clinical communication, physicians should be proficient in a number of skills, have specific knowledge, and project clearly-defined, appropriate attitudes.2 Communicational skills are specific, observable and testable.3,4
Clinical communication is currently an important part of the medical curriculum in both undergraduate and graduate training.5,6 In Spain the National Program for the Family Medicine Specialty7 includes clinical interviewing as an educational task that should form part of the training for these physicians. However, this recommendation is still too generic and inadequately elaborated; as a result its implementation has been uneven. In the undergraduate curriculum, training in communications skills --when present-- is merely testimonial. Thus, because of its clinical importance and because training in this important area is still in its earliest stages in Spain, it is necessary to determine how well basic communication skills are used by medical students, residents and practicing physicians, and what attitudes practitioners display in the course of interviews with patients. This information is needed before specific training programs can be designed; however, at present reliable information that can be taken to characterize the situation throughout the country is not available. The aim of the present study was therefore to discover how communication behavior (attitudes and use of skills and related tasks) evolves in family medicine residents during their third and final year of training.
Material and methods
Design and study population
A quasi-experimental before-after design was used. The study population comprised third-year residents at eight teaching units across Spain, located in Córdoba, Vizcaya, Cantabria, Jaén, Seville, Malaga, Asturias, and Orense (N=379). A sample size of 186 participants was estimated on the basis of a number of considerations. The percentage of correct answers on the questionnaire we used to evaluate knowledge, attitudes and communication skills (global data, attitude, communication tasks, communication skills--habilidades, in Spanish--in residents; abbreviated as GATHA-RES) was predicted to be 30% at the start of the third year of the residency program (pretest) and 50% at the end of the third year of training (post-test). The magnitude of difference we expected to detect was therefore 20%. We assumed an alpha error of 5%, a beta error of 20%, a bilateral hypothesis, a ratio of 1:1, and a 10% drop-out rate. A total of 193 participants were chosen by random sampling, stratified across teaching units, of all third-year residents who satisfied the inclusion criteria. Twenty-three residents were excluded mainly because they did not agree to participate, or because they were on leave for a prolonged period during the study.
Clinical scenarios
The residents faced six clinical cases (A, B, and C), presented as three clinical encounters at the beginning of the third year, and three more in the final month of the third year of training. The scenarios were designed by an ad hoc working group made up of family physicians and experts in the evaluation of clinical competence. The cases were paired such that although the clinical contents differed, they were similar in complexity. Thus case A represented a biomedical problem in a person 65 years old with no additional psychosocial or personal relation difficulties. The pretest situation presented a slight worsening of the patient´s asthma, and in the post-test situation the patient had diarrhea. Case B represented an organic manifestation of somatization (headache/backache) of a psychosocial problem (stress due to possible change in location of job/family-related stress related with starting a new job). The patient was 30 years old and expressed his expectations (computed tomography scan/referral to a specialist) in order to trigger a negotiation process. Case C represented a 45-year-old woman with an organic problem (inflammatory knee joint pain/abdominal pain) who expressed specific fears (invalidity/cancer) and intense emotions (mother´s death/mastectomy because of cancer). This patient also had specific demands (referral/laboratory tests) that triggered a negotiation process. All cases were represented by standardized patients who were trained according to guidelines that were established and agreed upon by members of the group responsible for this part of the study.
During the recording of the interviews each actors´ performance was observed as a check for appropriateness. In addition, during the study period the investigator responsible for this part of the method evaluated a group of interviews involving each actor to ensure that performances were appropriately standardized. All physician-patient encounters were recorded on videotape. The residents knew that the encounters were being simulated with standardized patients, and were asked to act as if they were actual consultations. There was a time limit of 10 minutes per encounter.
Study variables and information sources
Throughout the study period the residents carried out their regular training and clinical activities in accordance with the national plan (national curriculum) for specialization in family medicine with applicable local modifications. The main activity was providing out-patient care at a local health center on a full-time basis under the tutorship of a specialist in family medicine.
A self-administered questionnaire was used to obtain information on the characteristics of each teaching unit, tutors and the residents in their charge. The time used for each interview was also recorded.
Instrument used to evaluate the interviews
To evaluate the recorded interviews we used the GATHA-RES questionnaire (see Annex). This tool, designed and developed in Spain to evaluate the communication skills of medical residents, is divided into three sections or dimensions: a) attitudes, b) tasks, and c) skills. It has been validated and shown to be reliable. This instrument is an elaboration of the earlier 47-item GATHA-BASE questionnaire, which had undergone previous consensus validity evaluation by communication experts (communication and health group). The validation process used to refine the questionnaire for the desired target population (medical residents) comprised evaluation of internal consistency and between-observer reliability,8 followed by evaluation of content validity and within-observer reliability.9 This process resulted in a 27-item questionnaire with a Cronbach alpha value of 0.8, a between-observer reliability for each item, measured as the kappa index, of 0.41-0.95, and an intraclass correlation coefficient (ICC) of 0.97. Content validity was verified by factor analysis, which revealed a 9-factor structure that explained 62% of the variance. Within-observer reliability was verified with 47 recorded interviews from the actual study, camouflaged among other video recordings that were sent to the evaluators in four monthly batches during the 4-month evaluation period. Within-observer agreement was high, with a kappa index >0.63 and <1 and and ICC=0.94 in the first month, and a kappa index >0.80 and <1 and an ICC=0.95 in the fourth month.
All interviews were evaluated by an observer who was blind to the pretest or post-test nature of the interview. This evaluator was previously trained in the use of the GATHA-RES questionnaire. Between- and within-observer reliability was also checked as described above.
In the present study the highest score attainable varied for each of the three cases. In case A the highest possible score was 23 points, as items 9, 25, 26 and 27 were not applicable. In case B the highest possible score was 26 points, as item 27 was not applicable and items 6 and 12 were always fulfilled. In case C the highest score attainable was 27 points; all items were applicable.
Statistical analysis
Data coding and processing were done with the Access database program (Microsoft Office) by two persons working independently under the supervision of the investigator responsible for statistical analyses. This investigator ran periodic internal checks by systematically sampling 1 out of every 10 questionnaires and verifying the accuracy of data entry. The statistical analysis consisted of a descriptive study of the variables; 95% confidence intervals (95% CI) were calculated for the main estimators. Bivariate analyses consisted of McNemar´s test or Fisher´s exact test to compare the percentages of responses obtained for each item in the pretest and post-test; Student´t t test to compare paired data for mean total scores in the pretest and post-test; Pearson´s correlation coefficient to check the correlation between pretest and post-test scores; and one-way analysis of variance to investigate the relation between duration of the interviews and GATHA-RES score. Multivariate analysis consisted of multiple linear regression with the enter method to identify the independent variables related with mean GATHA-RES score for the three interviews recorded at the end of the residency period (post-test). Differences were considered significant at P<0.05; all contrasts were bilateral. All analyses were done with the SPSS (Statistical Package for Social Sciences).
Results
Table 1 shows the main characteristics of the population of third-year residents in family medicine, their tutors, and the teaching units.
Of the 193 residents who started the study, 154 completed it (20% drop-out rate). Losses were due to causes such as a change in center, illness, or technical problems with the video recording; however, the most frequent cause was failure of the physician to attend the recorded interview.
A total of 1024 clinical encounters were analyzed (544 at the start and 480 at the end of the third year of residency). Seventeen recordings were unusable because of technical problems.
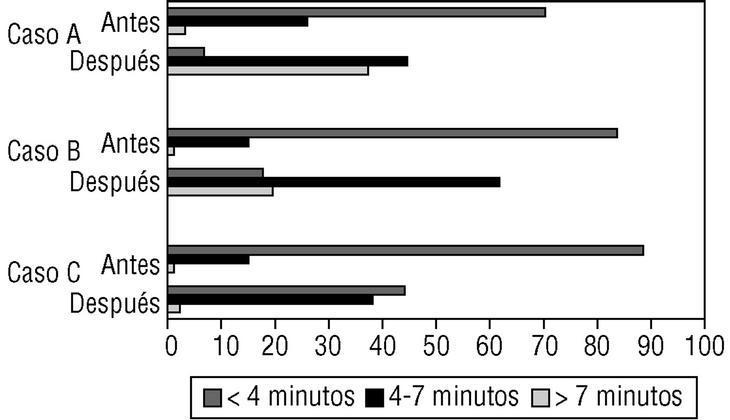
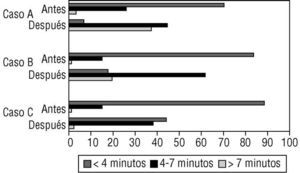
Figure 1 shows the duration of the interviews. The time spent on each of the three interviews was significantly shorter at the end of the study period.
Figure 1:Mean time spent by residents on each consultation at the beginning and at the end of the study period.
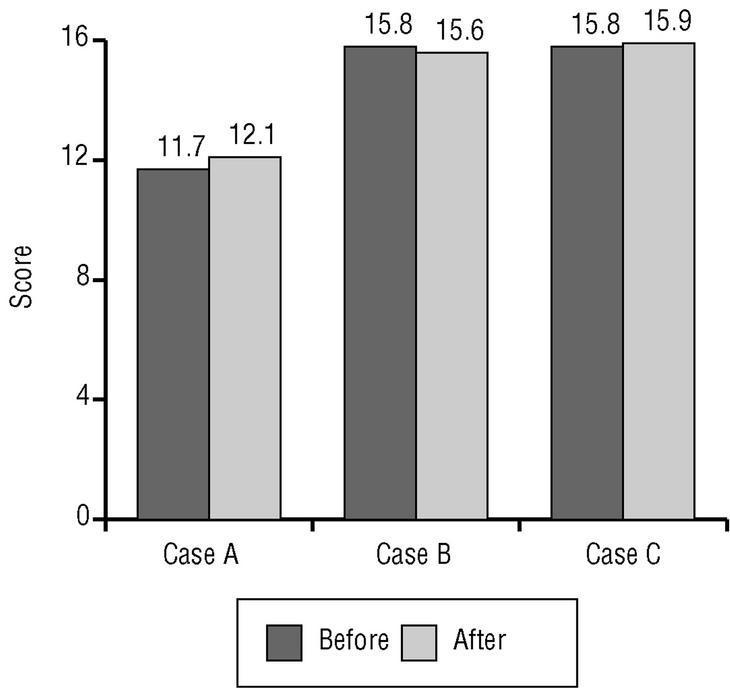
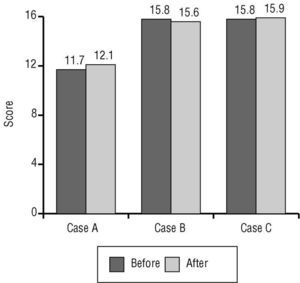
Figure 2 shows the overall scores for all residents on each case at the beginning and at the end of the study. The differences were small and nonsignificant. Mean scores ranged from 11.66 points (case A, pretest; range, 6-17 points; SD, 1.98; 95% CI, 11.38-12.06) to 15.90 points (case C, post-test; range, 8-22 points; SD, 2.84; 95% CI, 15.46-16.45). The time spent on each interview was directly proportional to mean score for each case (P<0.05).
Figure 2:Mean scores obtained by residents on the GATHA-RES questionnaire for consultations at the beginning and at the end of the study period.
Table 2 lists the pretest and post-test results for each item in the three dimensions of the GATHA-RES questionnaire. In case A there were significant increases in the scores for items related with confidence (item 3), attentiveness (item 4), and formal and organizational aspects of the consultation (items 5, 7, 19, and 20). Post-test scores were lower for items that dealt with social and family environment (item 15) and the impact of symptoms on daily life (item 11). In case B we found low initial scores and subsequent decreases particularly for items related with the impact of the problem on the patient´s life (item 11), mood (item 13), stressful life events (item 14) and, to a lesser extent, the social and family environment (item 15), pointing (item 22), and negotiation skills (items 25 and 26). There were improvements in the scores for items related with etiquette (item 20) and organization (items 7 and, to a lesser degree, 19). In case C the pretest and post-test scores were similar. The post-test improvements in items that dealt with etiquette and organization of the visit (items 7, 19 and 20) compensated for the lower post-test scores in more important and determining items such as exploration of mood (item 13), social and family environment (item 15), impact of the problem on the patient´s daily life (item 11) and negotiation strategies (items 25 and 26).
The correlation coefficients for scores at the beginning and at the end of the study were statistically significant (P<0.05), although the correlation was weak for all cases (case A, 0.230; case B, 0.242; case C, 0.278; cases A+B+C, 0.3599). Multiple linear regression analysis (Table 3) showed that the variables which best predicted residents´ communication skills were age (inverse correlation with GATHA-RES score), duration of the interviews (direct correlation with score), tutor´s training in clinical interviewing, and teaching unit.
Discussion
This study represents one of the first attempts in Spain to identify aspects of clinical communication that physicians in general, and residents in particular, develop in clinical encounters. Prior knowledge of these aspects is essential to plan and modify, when appropriate, educational programs on the basis of empirical data rather then mere assumption. The number of residents and different centers that participated in this study is among the highest to date, thus we believe our results to be highly consistent. However, our findings are, in general terms, negative, like those reported by Torío Durantez and García Tirado for a different sample of residents and staff physicians.10 Theirs is the only other study which, to our knowledge, used videotaped encounters to evaluate the consultation style of Spanish physicians. These authors reported consultation style to be physician-centered and illness-centered rather than open and patient-centered.
The residents´ skills related with formal and organizational aspects of the interview improved in all three of the cases in the present study. In particular, after their third year in the regular primary care residency program, the duration of the interviews was significantly shorter. This reduction was accompanied by very modest improvements in case A (the patient with a biomedical problem); thus for this type of patient, interviewing skills can be considered to show some degree of improvement as duration of the interview decreases. However, in the other two cases an overall backslide was seen: the residents failed to evaluate key psychosocial elements and did not use communication skills considered important to establish an effective relationship with the patient and for the interview to be clinically effective.1
Although their influence on the results was considered slight, some limitations derived mainly from the method we used need to be taken into account in the interpretation of our findings. With regard to the measurement instrument, the checklist format of the GATHA-RES questionnaire records only whether specific behaviors occurred in the course of the interaction, but not the degree to which they were manifested. This latter feature is better reflected with a Lickert scale or with interactional analysis.11 The exploration of symptoms and information provided to the patient were discriminative in the validation of the instrument,8 but were not found to be discriminative in the present study; this made it impossible to analyze these areas. Another important consideration is that the GATHA-RES questionnaire does not record the type of questions the physician asks the patient, ie, open-ended, closed, leading, or some other type of narrative facilitation.12-16 The questionnaire does not indicate who dominated the conversation in terms of time, and does not record information about smiling or other elements of social conversation, which are known to be related with the quality of clinical communication.12,15 Also absent is information on when manifestations of empathy and understanding, which represent opportunities for emotional expression and empathy,17 occur in the course of the interview. Moreover, because clinical communication is analyzed separately from the diagnosis, when the diagnosis was ominous we cannot rule out that residents might have concentrated on other aspects of the clinical process. In this connection, a study of tests of clinical competence18 showed that more experienced clinicians scored lower. However, we believe this would not be the case in residents whose experience is more limited.
Despite these considerations, the GATHA-RES questionnaire provides valuable information. The patient roles in cases B and C provided many potential opportunities for the physician to explore the patient´s agenda and thus develop the skills and carry out the tasks needed to build a relationship and perform an appropriate psychosocial examination. To judge from the results, the residents did not take advantage of these opportunities. Nonetheless, the questionnaire has been shown to have discriminative validity,9,19 a fact which supports the validity of the results we report.
Another limitation lies, as noted earlier, in the design of the ca ses based on standardized patients. The results may have been influenced by the facts that the patients were not authentic and the interview conditions were not those of an actual clinical encounter. However, the characteristics of the experimental conditions favored appropriate interviewing: perhaps the most important of these characteristics were the availability of more time for the interview than under real conditions, and the absence of pressure to make a decision that would actually affect the person. Both these conditions have been used by us19 and by other researchers, and have been found to be useful.12,13,15,20-23 The clinical challenges, although differing in complexity, reflected real cases encountered in primary care; nonetheless it could be argued that a patient complaining of headaches generally produces more anxiety in the trainee physician that does a patient with backaches. In the case B pretest (headache), the residents might have been concerned with performing a more exhaustive physical examination and hence might have spent more time on the examination than they used for the case B post-test (backache). However, this would not account for the their failure, in the post-test, to investigate associated psychosocial factors that deserved exploration in patients with back pain as much as they would have in patients with headaches.
It is important to recall that there was little variation in the overall scores across the three cases. Considering that we transformed qualitative assessments into quantitative information, the differences were nonetheless very small; although we believe this observation is of little importance per se, it is significant that the scores for certain items were worse at the end of the study, and that after a third year of training at the center where residents habitually practiced, we failed to find significant improvements.
It would have been interesting to measure the patients´ subjective impressions of, and satisfaction with, their physician´s interview style. One recent study found that the patient´s perception of the encounter correlated better with health outcome that did an observer´s assessment of the interview.24 With regard to the evaluation of the impact of a given educational measure, although its influence is often clearly reflected in the patient´s degree of satisfaction,12,15,25,26 it is more difficult to determine, with the instruments now available, whether the physician´s behaviors and skills change, or whether a specific measure has any actual repercussions on the patient.27 However, well-designed studies are now appearing that demonstrate positive changes in practicing physicians23,26,28,29 and residents.12,15,30,31 And studies with medical students have reported a positive influence of certain techniques on basic communication skills.20,22,32-34
It is worrying that residents did not explore psychosocial aspects of the health problems that could have been assumed to have a psychosocial component, and which are frequent within the setting of the residents´ current and future practice. Also of concern is their failure to use communication skills known to be effective,1 and their failure to initiate negotiations to at least try to evaluate the causes of a patient´s «inappropriate» or «surprising» demand. To judge from existing evidence, these failings are likely to affect the physician´s ability to detect and resolve clinical problems, and are also likely to detract from the quality of the physician-patient relationship. A poor physician-patient relationship has a negative influence on clinical tasks,3,4,35 increases malpractice suits36 and favors the inappropriate use of resources by both the patient37 and the physician.24 Because of the nature of the family medicine (ie, continuity and personalized care, familiarity, gateway to the medical system, and types of health problems encountered), this consideration is central to the basic technology involved in this clinical specialty: clinical communication. If the resident´s performance worsens as the time spent with each patient becomes shorter, and if these changes occur during the final year of training at health centers, the situation is worthy of careful analysis involving many other factors in addition to those examined here.
One of the most interesting findings in this study is the high priority residents seem to give to time management. They assume an inherent time shortage and concentrate on improving this situation by the time they finish their training. One of the greatest worries of Spanish primary care physicians is the feeling that time is short and that the patient burden is large,38 and this appears to be one of the messages that tutors transmit. We feel that this situation is the logical, albeit perverse, consequence of the excessive numbers of users assigned to primary care centers, and of an overburdened primary health care system. Because quality performance is related with spending more time with the patient, it is revealing that the preoccupation with time should create bad habits in clinical practice.
The residents´ attitude toward these topics is a further factor that might have influenced the results. The way the health care system is organized, and the procedure used to fill physicians´ posts, go a considerable way toward explaining the development of an «underground curriculum». The primary care system in Spain demands certain skills and knowledge sets to the detriment of certain others: posts are still filled mainly by multiple-choice examinations (or similarly structured procedures) that reward factual knowledge, and in which communication skills and consultation style count for very little. The system neither rewards nor penalizes practitioners who do not know how to attend to their patients´ personal needs, a skill that is more highly valued in predominantly private systems of health care and in public systems which include payment based on the number of patients actually seen, and which offer patients the free choice of physician. The nature of the current Spanish system conditions residents´ priorities and attitudes, especially in their final year of training, when they are most concerned with their future employment options.
An additional explanation for residents´ attitudes toward the clinical interview lies in the fact that the system for assigning residency posts forces a plethora of medical school graduates with little interest in family medicine to specialize in this branch of practice. Both younger residents and medical students appear to be more conscientious with regard to communication issues in comparison to residents who are about to finish their clinical training; the former also appear to be more sensitive to these issues, judging from the results of an earlier study39 and from the findings of the present analysis, which found performance to correlate inversely with age. Training in communication skills should form part of graduate training from the first year.4 As Smith and colleagues noted,15 residents should first be trained in the key elements of their specialty, including clinical communication. The best approach, however, would be a program of structured training beginning in the first years of medical school, as in other countries.4,6,40
The previous training (in medical school and in earlier residency programs) that residents bring with them when they arrive at the health center is hospital-centered and disease-centered, paternalistic and physician-centered. Paradoxically, after this prior experience they are still better able to provide patient-centered care than after one year of contact with what in theory should be an additional phase of patient-oriented training and practice. The reason for this appears to lie in the fact that at the start of their rotation through the health center, residents are not yet aware of all the characteristics of the context in which family medicine is practiced. Once they become familiar with these features and come to feel comfortable in the family medicine clinic, they adopt behaviors learned at hospitals as well as those acquired at health centers. In fact, most family doctors display a disease-centered consultation style.10 A sense of what matters is developed by--among other things--imitation of role-models.41 In this connection we previously found that of all variables, the tutor had the greatest influence on residents´s training in interviewing skills.42 However, further analysis of the difficulties tutors have in transmitting educational messages to trainees is beyond the scope of this discussion.
One positive finding this study revealed is that, judging from the agreement in scores, residents do not appear to maintain their consultation styles throughout the third year of training. In other words, those who score highest and lowest (ie, those who initially have a more or less strongly patient-centered style) at the beginning of the third year did not necessarily obtain similarly high or low scores at the end of this period. This finding suggests that at this stage in their training, family medicine residents do not yet have a rigid consultation style; in theory, external factors could induce positive changes. This is also supported by the fact that age correlated inversely with improved performance, hence the potential for changes in behavior may be potentially greater in earlier stages of training. The influence of the tutor was emphasized by the higher scores of residents whose tutors were sensitive to and well trained in interviewing skills. These two observations should orient future training strategies.
In conclusion, residents learn to shorten the duration of consultations at the expense of a decline in basic communication skills for the provision of appropriate patient care. These declines were most notable in the exploration of personal and contextual characteristics of the illness, and in negotiation skills. The variables that best predicted a good communication skills in family medicine residents were age (inverse correlation), duration of interviews, and tutor´s training in clinical interviewing. These results may be extrapolatable to residents in other clinical specialties, and suggest that substantial changes are needed in the training of residents in family medicine in Spain.
Acknowledgements
We than GSK España for their help with this project, and Dr. José M. Martínez Carretero and the Institut d´Estudis de la Salut (IES) for providing facilities and help with the standardized patients. We also thank Dr. Emilio Sánchez Cantalejo of the Escuela Andaluza de Salud Pública for his comments on the statistical methods, and Drs. Rafael Llamas, Inmaculada Jaramillo and Raquel Portillo of the Unidad Docente de Medicina de Familia in Córdoba for their help with data management. Our appreciation goes to all third year residents in family medicine (1996-1999 program) at the authors´ family medicine teaching units for their participation in this study.
Correspondence: Roger Ruiz Moral, Coordinador, Unidad Docente de Medicina de Familia, C/ Dr. Blanco Soler 4, 14004 Córdoba, Spain. Email: rruizm@papps.org .This work was supported by the Fondo de Investigación Sanitaria (Project 1244/98) and the Servicio Andaluz de Salud (Project 113/98). Manuscript accepted for publication 8th October 2001.