We have read with interest the article by Rinella ME et al. [1], in which metabolic dysfunction-associated steatotic liver disease (MASLD) has been proposed as a novel diagnostic term that differs from non-alcoholic fatty liver disease (NAFLD). The original name change from NAFLD to metabolic dysfunction-associated fatty liver disease (MAFLD) has successfully reduced the stigma associated with the condition and emphasized its close connection with metabolic disorders [2–4]. However, the definition of MAFLD is complex, and some subitems, such as HOMA-IR and high-sensitivity C-reactive protein (hs-CRP), are not routinely measured in clinical practice across regions, which leads to underdiagnosis and delayed treatment [5,6]. The proposed name change to MASLD, which optimizes the MAFLD definition, is simplified and acceptable. MASLD is defined by inclusion rather than exclusion criteria and is diagnosed in patients with hepatic steatosis and metabolic risk factors. However, its practicality and effectiveness have not been tested and validated in real-world settings. We aimed to identify MASLD patients and compare the characteristics of MASLD and non-MASLD steatosis patients.
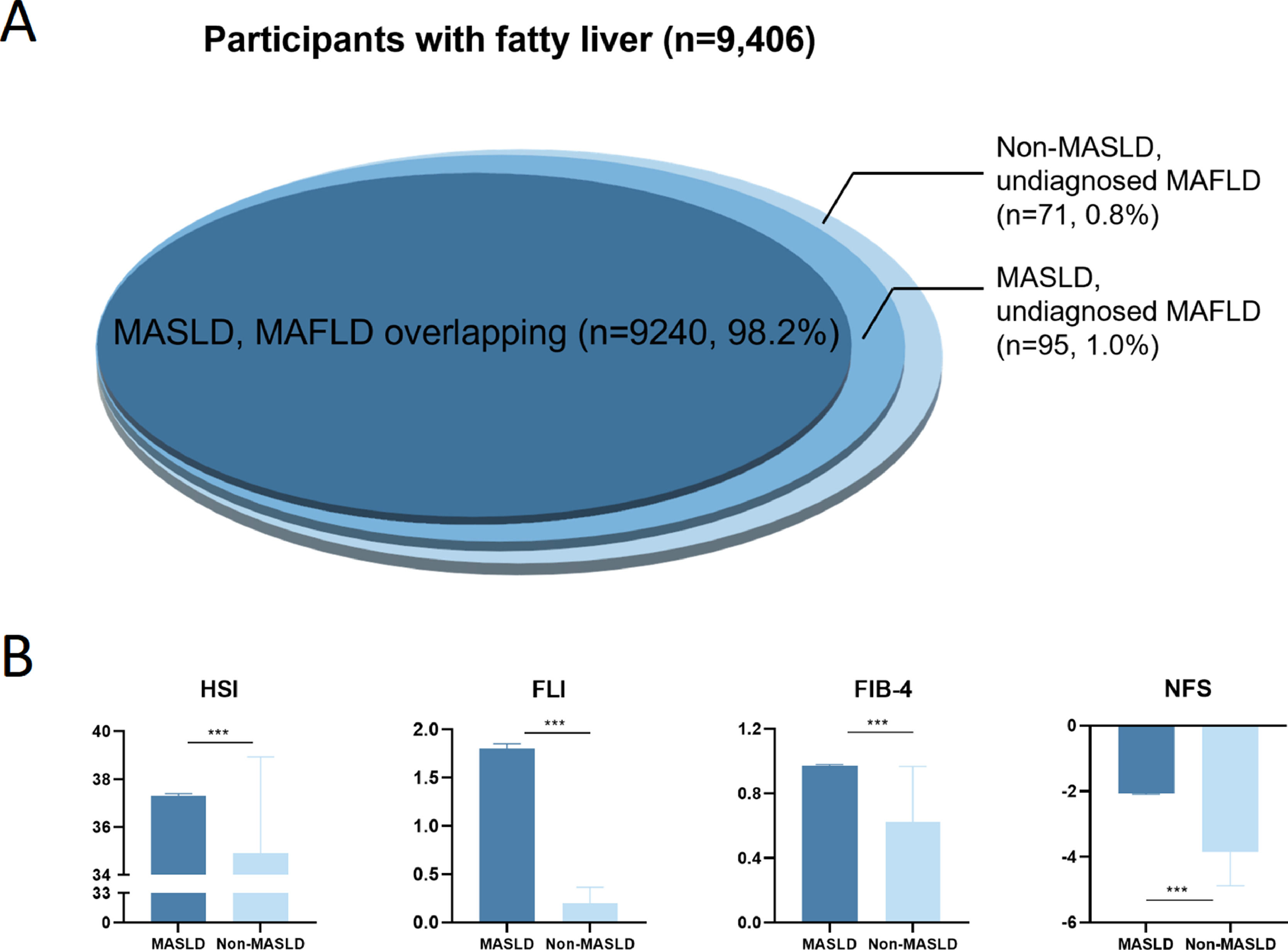
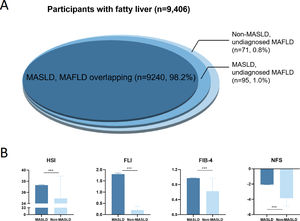
Our study involved 9406 patients diagnosed with fatty liver by ultrasound for analysis. Of them, 9240 (98.2%) patients were diagnosed with MAFLD and MASLD overlapping, and 95 (1.0%) patients were classified as MASLD but undiagnosed MAFLD due to the lack of hs-CRP and insulin. And 71 (0.8%) patients were identified as non-MASLD but undiagnosed MAFLD patients (Fig. 1A). In addition, MASLD patients were older, predominantly male, and exhibited a higher prevalence of metabolic disorders and elevated liver enzymes compared with non-MASLD patients. Additionally, the MASLD group displayed significant liver steatosis and fibrosis (Table S1), including elevated HSI [37.31 (34.77, 40.22) vs. 35.00 (32.35, 37.82), p<0.001], FLI [1.80 (0.81, 4.17) vs. 0.14 (0.09, 0.24), p<0.001], FIB-4 [0.97 (0.69, 1.34) vs. 0.51 (0.37, 0.78), p<0.001] and NFS [−2.06 (−2.96, −1.11) vs. −3.85 (−4.58, −3.26), p<0.001] (Fig. 1B). These findings highlight the importance of accurately identifying and treating MASLD patients to prevent further liver damage and improve outcomes.
In conclusion, the MASLD definition represents an improvement in identifying patients with substantial hepatic fibrosis and steatosis within the fatty liver population. The name change is necessary to reflect the underlying pathophysiology and enhance diagnostic accuracy accurately.
Authors' contributionsWen Xie: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing review & editing. You Deng, Wenya Chen: Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing original draft, Writing review & editing.
Availability of data and materialSurvey data will be shared upon reasonable request to the corresponding author.
Declaration of interestsNone.