Background. Cirrhotic patients present a complex interaction between deficient synthetic liver function, hemodynamic abnormalities and superimposed conditions that alter coagulation system. This alters both coagulation and fibrinolytic processes,increasing bleeding and thrombosis risks. Particularly, critically ill cirrhotic patients represent a diagnostic challenge since they have multiple comorbidities making the thrombotic and bleeding risks unpredictable. The prevalence of bleeding and thrombosis in this subset of patients remains poorly described. The main aim of this article is to describe the prevalence of thrombotic and hemorrhagic complications in cirrhotic patients admitted between 2007 and 2012 at Médica Sur Clinic and Foundation ICU.
Material and methods. We performed a five years retrospective study including every cirrhotic patient admitted to ICU between January 2007 and December 2012.
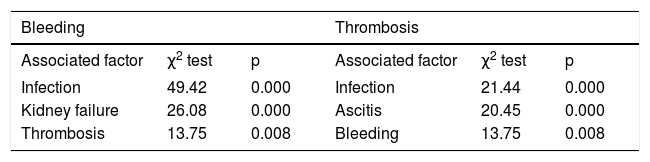
Results. The incidence of hemorrhage was 48.5%, the overall incidence of thrombotic complications was 13.66%. Variceal bleeding was the most prevalent hemorrhagic event and portal vein thrombosis the most common thrombotic event. Factors associated with presenting a bleeding episode included kidney injury, infection an thrombosis. Factors associated with increased thrombotic risk included ascitis,infection and bleeding.
Conclusion. Critically ill cirrhotic patients have an high risk for both thrombotic and bleeding episodes. The association between the presence of bleeding and thrombotic events was statistically significant.
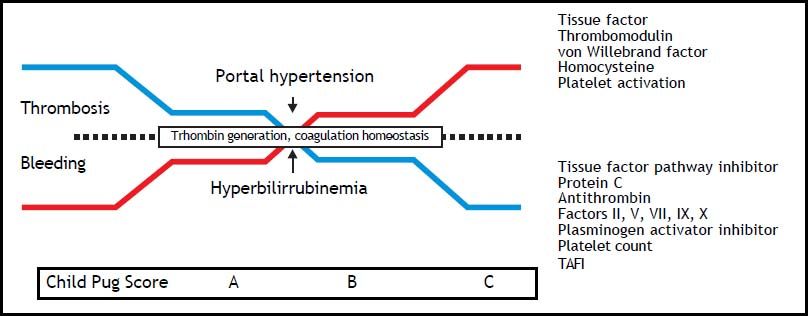
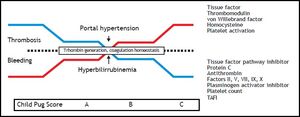
Cirrhotic patients have an elevated risk to develop both thrombosis and hemorrhage. In a single patient, bleeding and thrombosis may be present at the same time. Especially, critically ill cirrhotic patients represent a diagnostic and therapeutic challenge. Although variceal bleeding remains the most prevalent coagulopathy-associated exacerbation, thrombotic complications are not uncommon in the cirrhotic patient1–5 (Figure 1).
Ccagulation abnormalities according to cirrhosis progression, reflected by Child-Pugh Score. As cirrhosis progress, levels of tissue factor pathway inhibitor, protein C, antithrombin, factors II,V, VII, IX, X, plasminogen activator inhibitor, platelet count and TAFI decreases, while tissue factor, thrombomodulin, von Willebrabd Factor, homocysteine an platelet activation increases, leading to stable thrombin generation and a fragile balance between thrombosis and bleeding. Aggregated factors, such as portal hypertension or hyperbilirrubinemia, may trigger bleeding or thrombotic events. TAFI: thrombin-activatable fibrinolysis inhibitor.
Variceal bleeding represents the 80-90% of the bleeding episodes; risk factors for developing variceal bleeding include advanced Child-Pugh class, large varices and the presence of red wale markings. High levels of D-dimer and t-PA have been described as significant laboratory markers for variceal bleeding risk.4,6 Spontaneous intracerebral hemorrhage prevalence in hospitalized cirrhotic patients is 0.8% for all etiologies, 80.3% virus-related and 1.8% alcohol-related groups. It is not related to Child-Pugh score or prolonged PT.6
The incidence of biopsy-associated bleeding in patients with histological diagnosis of cirrhosis is 0.7%; neither PT, prolonged activated partial thromboplastin time (aPTT) nor thrombocytopenia are reliable predictors for biopsy related bleeding.6 In patients with advanced hepatitis C, percutaneous liver biopsy related bleeding risk is: 0.4%, for patients with 1.1 or less international normalized ratio (INR) 1.1%, for patients with a 1.2 INR, and 2.4% for patients with an INR of 1.3 or higher.7 Central venous cannulation in cirrhotic patients carries a low risk for bleeding even if the INR is 1.5 or more.6,7 Paracentesis has a 0.2% incidence of severe hemorrhage, with a 0.016% of death rate. Bleeding risk is not related with a PT up to twice the midpoint of normal values or with a platelet count of < 50,000.6
Patients with cirrhosis have a 1.65-1.74 relative risk of deep venous thrombosis (DVT) compared with controls. The prevalence of DVT in hospitalized cirrhotic patients is 0.8 % and 0.5% of hospitalized cirrhotic patients present their first venous thrombosis during hospitalization. Reduced aPTT, and low serum albumin levels have been found to be an independent predictor for developing DVT, while prolonged INR does not appear to protect against the development of hospital-acquired DVT. Decompensated cirrhotic patients admitted to an inpatient hepatology service have a 7% incidence of DVT in a 6-month period.4,5,8
Portal vein thrombosis (PVT) is the most common thrombotic event in cirrhotic patients, with a reported incidence from 7.4 to 11%. Reported risk factors include prothrombotic states arising from protein C, protein S and antithrombin III deficiencies, myeloproliferative disorders, sclerotherapy of esophageal varices, abdominal surgery, hepatocellular carcinoma, antiphospholipid syndrome, mutations of prothrombin, factor V Leiden and methylenetetrahydrofolate reductasa, a key enzyme in the folate cycle and homocysteine metabolism.8,9 From all thrombotic events in cirrhotics, 65.5% corresponds to DVT, 19.5% to PE, and 15% to patients with both DVT and PE. Only 7% of the patients who present thrombosis were receiving medical thromboprophylaxis at the time the thrombotic event occurred. Until now, the exact prevalence of thrombosis and hemorrhage in this particular population remains poorly described. The aim of this study is to describe the prevalence of thrombotic and bleeding complications in cirrhotic patients admitted to the ICU.10,11
Material and MethodsThe medical records were retrospectively reviewed for every cirrhotic patient admitted to ICU from January 2007 to December 2012, excluding patients with non-cirrhotic hepatic disease, and pregnant women. Patients whose medical records did not accomplished all variables studies were discharged from the study.
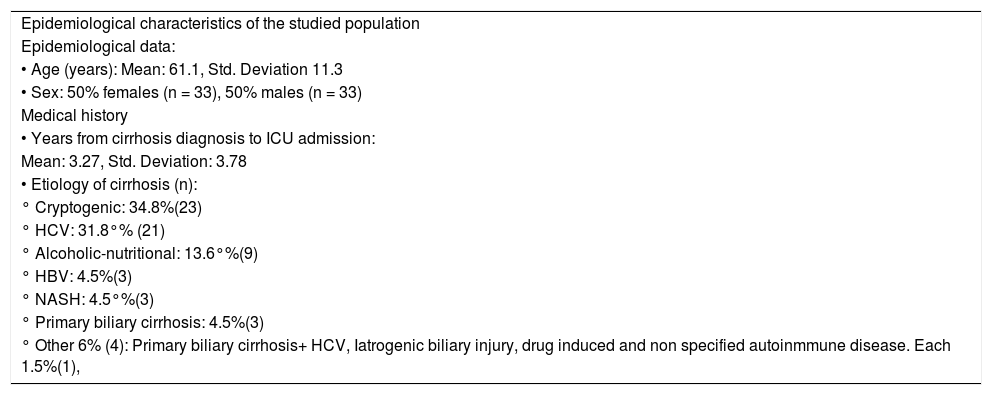
Assessed variables included epidemiological data, medical history data, variables associated to the clinical situation at the moment of ICU admission, clinical course and clinical outcome variables. Epidemiological and baseline characteristics at ICU admission are summarized in tables 1 and 2 respectively.
Baseline characteristics of the studied population.
| Epidemiological characteristics of the studied population |
| Epidemiological data: |
| • Age (years): Mean: 61.1, Std. Deviation 11.3 |
| • Sex: 50% females (n = 33), 50% males (n = 33) |
| Medical history |
| • Years from cirrhosis diagnosis to ICU admission: |
| Mean: 3.27, Std. Deviation: 3.78 |
| • Etiology of cirrhosis (n): |
| ° Cryptogenic: 34.8%(23) |
| ° HCV: 31.8°% (21) |
| ° Alcoholic-nutritional: 13.6°%(9) |
| ° HBV: 4.5%(3) |
| ° NASH: 4.5°%(3) |
| ° Primary biliary cirrhosis: 4.5%(3) |
| ° Other 6% (4): Primary biliary cirrhosis+ HCV, Iatrogenic biliary injury, drug induced and non specified autoinmmune disease. Each 1.5%(1), |
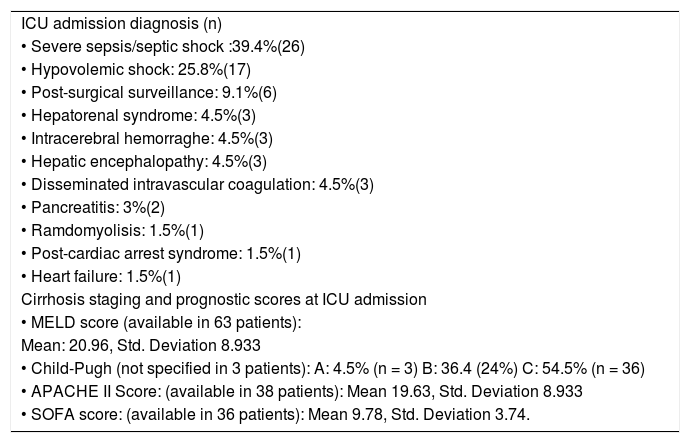
Clinical condition at ICU admission of the studied population.
| ICU admission diagnosis (n) |
| • Severe sepsis/septic shock :39.4%(26) |
| • Hypovolemic shock: 25.8%(17) |
| • Post-surgical surveillance: 9.1%(6) |
| • Hepatorenal syndrome: 4.5%(3) |
| • Intracerebral hemorraghe: 4.5%(3) |
| • Hepatic encephalopathy: 4.5%(3) |
| • Disseminated intravascular coagulation: 4.5%(3) |
| • Pancreatitis: 3%(2) |
| • Ramdomyolisis: 1.5%(1) |
| • Post-cardiac arrest syndrome: 1.5%(1) |
| • Heart failure: 1.5%(1) |
| Cirrhosis staging and prognostic scores at ICU admission |
| • MELD score (available in 63 patients): |
| Mean: 20.96, Std. Deviation 8.933 |
| • Child-Pugh (not specified in 3 patients): A: 4.5% (n = 3) B: 36.4 (24%) C: 54.5% (n = 36) |
| • APACHE II Score: (available in 38 patients): Mean 19.63, Std. Deviation 8.933 |
| • SOFA score: (available in 36 patients): Mean 9.78, Std. Deviation 3.74. |
Statistical analysis was performed using SPSS v. 17 software. For continuous variables, average and standard deviations were calculated. Chi Square or Fisher’s exact test were used to find any association between categorical variables. For all statistical variables, a p value < 0.05 was considered statistically significant using a bidirectional hypothesis.
ResultsBetween January 2007 and December 2012, 67 patients with cirrhosis diagnosis were admitted in ICU. One patient was excluded because he had a liver transplant history 2 years before ICU admission.
Primary admission departments were: emergency department in 40 patients (60.6%), non-critical hospital room in 12 patients (18.2%), ICU in 10 patients (15.2%) and intermediate care unit in 4 patients (6.1%).
At admission, the average age was 61.1 years. Thirty-three (50%) were females and 33 (50%) males. The 3 most common cirrhosis etiologies were cryptogenic cirrhosis (34.8%), HCV (31.8%) and alcoholic-nutritional (13.6%). In 51 (77.2%) cases, the period between cirrhosis diagnosis and ICU admission was recorded, and its average was 3.2 years.
The main hospital-admission diagnosis were: upper gastrointestinal bleeding (19 cases, 28.8%), neurological deterioration (18 patients, 27.3%) and unknown origin sepsis (12 cases, 18.2%). 5 patients (7.6%) were primarily admitted due to multiple contusions, 3 patients (4.5%) for scheduled hepatectomy. Etilic intoxication and hepatorenal syndrome represented 3.0%, each. Thoracic pain, post-cardiac arrest syndrome, pulmonary embolism, scheduled liver transplantation and thrombocytopenia represented 1.5% of hospital admission diagnosis each.
At hospital admission, 18 (27.4%) had diabetes mellitus type 2 (DM2), 18 (27.4%) systemic arterial hypertension (SAH) diagnosis and 9 (13.6%) both DM2 and SAH. Some other patients (24) had other comorbidities: hypotiroidism and history of rheumatic fever affected 6.1% each and 7.5% had a hepatocarcinoma.
Before ICU admission, 54.5% had at least one documented bleeding episode, while 3.0% had presented at least one documented thrombosis episode; 37.8% had suffered from at least one documented hepatic encephalopathy episode, 25.7% had experienced at least one documented spontaneous bacterial peritonitis episode, 36.6% had documented portal hypertension of any degree, and 19.6% of patients had at least one documented episode of acute kidney injury or any kind of renal insufficiency.
The most common ICU admission diagnosis were severe sepsis/septic shock (39.4%), hypovolemic shock (25.8%) and post-procedural follow-up (9.1%). Post-procedural diagnoses were 1 splenectomy, 1 hepatectomy, 1 hepatocarcinoma radioablation, 1 hepatocarcinoma embolization, 1 hip arthroplasty and 1 liver transplantation.
At the ICU admission, 54.4% presented acute kidney injury, 51.5% any degree of hepatic encephalopathy, 34.8 ascites and 42.8% an active infection. 39.4% had active bleeding and 7.6 % thrombotic complications.
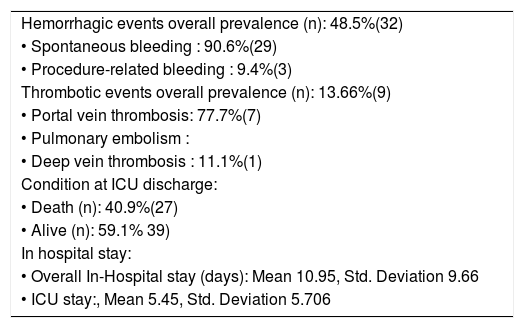
Thrombotic and bleeding episodes prevalenceThe prevalence of any hemodynamically significant bleeding at any time from hospital admission to discharge was 48.5% (32 patients). Among patients who bled, 65.6% (21 patients) had experienced at least one bleeding episode prior to hospital admission, and in 75% (24 patients) the diagnosis of active bleeding had been established at admission.
Out of patients who bled, 90.6% (29 patients) showed spontaneous bleeding while those with procedure related bleeding (3 patients) represented 9.4%. There were no patients with both spontaneous and procedure related bleeding.
Among patients who presented spontaneous bleeding episodes, 25 (90.6%) presented variceal bleeding, 8 (27.5% ) non-variceal gastrointestinal hemorrhage, 3 (10.3%) spontaneous intracerebral hemorrhage and 1 (3.4%) spontaneous rupture of hepatocarcinoma.
Out of patients who bled, only one was under anticoagulation and no patients were under antiagregation therapy nor pharmacological thromboprophylaxis. There was no significant relationship between being under anticoagulation, antiagregation or pharmacological thromboprophylaxis with the presence of any bleeding episode.
There were no significant disparities between the different etiologies of cirrhosis or Child-Pugh Score at ICU admission and the presence of any bleeding episode. Comparing the group of patients who bled and those who did not, there was no significant difference in mean MELD score nor in the number of years between cirrhosis diagnosis and hospital admission. There was a significant association between any kind of kidney failure or infection during hospital stay and the presence of hemorrhage.
The mean PTTa was significantly higher among patients who had bled in comparison to those who had not. There were no significant differences in mean hematocrit, platelet count, PT, bleeding time, fibrinogen, or D dimer in the group of patients who bled and those who did not, or between the patients who presented thrombosis and those who did not.
There was no significant difference in ICU or hospitalization days between patients who bled and those who did not, neither between those who presented thrombotic complications and those who did not. There was a significant association between the presence of bleeding and death.
The thrombotic events prevalence at any time from admission to discharge was 13.6% (9 patients). Among those who presented thrombosis, 71.4% (5 patients) had suffered from at least one thrombotic episode previous to hospital admission and in 57.1% (4 patients) the diagnosis of thrombosis was established at admission.
Among patients who presented thrombotic events, 7 (10.6%) experienced portal vein thrombosis, 1 (14.3%) pulmonary embolism and 1 (14.3%) deep vein thrombosis. 4 patients (12.5% of patients who bled and 57.1% of patients with thrombosis) had both thrombotic and bleeding complications during their hospital stay.
There were no significant differences between the different etiologies of cirrhosis and the presence of any thrombotic episode. There were no significant differences in mean MELD score between the group of patients who had a thrombotic episode and those who did not.
In contrast to hemorrhagic events, thrombotic events did have a significant association with the presence of ascitis, infection or a Child Pugh C status at ICU admission. In comparison with the “non-thrombotic episodes group”, the group of patients who presented any thrombotic episode had a higher mean number of years between the cirrhosis diagnosis and ICU admission and a higher mean SOFA score at admission. The association between the presence of bleeding and thrombotic events was statistically significant. The clinical outcomes are summarized in table 3 and statistically significant associations are summarized in table 4.
Clinical outcomes in the studied population.
| Hemorrhagic events overall prevalence (n): 48.5%(32) |
| • Spontaneous bleeding : 90.6%(29) |
| • Procedure-related bleeding : 9.4%(3) |
| Thrombotic events overall prevalence (n): 13.66%(9) |
| • Portal vein thrombosis: 77.7%(7) |
| • Pulmonary embolism : |
| • Deep vein thrombosis : 11.1%(1) |
| Condition at ICU discharge: |
| • Death (n): 40.9%(27) |
| • Alive (n): 59.1% 39) |
| In hospital stay: |
| • Overall In-Hospital stay (days): Mean 10.95, Std. Deviation 9.66 |
| • ICU stay:, Mean 5.45, Std. Deviation 5.706 |
The present study focuses on a special subgroup of cirrhotic patients, which shows many of the well-known predisposing factors, for both thrombotic and hemorrhagic events. Thus, it is expectable that the overall prevalence of these complications will be higher than in ambulatory and non-ICU hospitalized patients.1–4
The incidence of DM2 and SAH was high, in concordance with the high prevalence of metabolic syndrome in the hispanic population.12–14
We reported an incidence of hemorrhagic complications nearly two times higher than the one reported in ambulatory population. This can be explained because the ICU admitted population studied already had a 33% prevalence of bleeding episodes history.15
The type of hemorrhage distribution within the total bleeding episodes widely varies from those reported in previous studies. Although variceal and non-variceal gastrointestinal bleeding remained the most prevalent kinds of hemorrhage, a 4.5% overall prevalence of intracerebral hemorrhage corresponding to 9.3% of the total bleeding episodes is found.16–18
The prevalence of procedure related bleeding episodes was higher than the one found in previous reports. Remarkably only one bleeding was related to traditionally reported procedures (central venous cannulation) while the two others corresponded to mayor procedures (total hip arthroplasty and hepatocarcinoma embolization, respectively). Although the high incidence of well-known risk factors for bleeding related to central venous cannulation, bleeding incidence remained the same to those in previous reports probably because they had all been made by experienced personnel.16–18
In contrast to bleeding episodes, thrombotic episodes prevalence was not higher than in ambulatory nor even hospitalized cirrhotic patients, even when taking into account more kinds of thrombotic events (deep vein thrombosis, pulmonary embolism, ischemic cerebrovascular disease and portal vein thrombosis). This may be explained in terms of lack of systematic ultrasonography screening of a highly prevalent event that does not have overt clinical manifestations.19–21
The fact that hemorrhagic but not thrombotic complications prevalence was higher in the present study population than in previous reports, the association between thrombotic episodes and higher Child-Pugh Score, and the association between thrombotic episodes and longer time lapses between cirrhosis diagnosis and ICU admission may be explained by at least two different, not mutually excluding, facts:19–21
- •
Thrombosis is a late-onset complication of hepatic failure, and therefore it is present only in patients with less hepatic function (i.e. those with Child-Pugh C status) or in those with a stronger “second prothrombotic hit” (i.e. ascitis, infection).
- •
Thrombosis is a late finding in hepatic failure (i.e. thrombotic episodes being suspected only as an exclusion diagnosis in the most severely ill patients). Notably, only 15% did have a complete deep vein thrombosis ultrasonography screening, including portal and pulmonary thrombosis, thus it cannot be assumed that the reported prevalence corresponds to the real prevalence of thrombotic events. Given the high rate of positive findings (70% of Doppler evaluations yielded positive results) a prospective routine evaluation of thrombotic complications in critically ill cirrhotic patients may reveal a much higher prevalence, and may not be associated with a higher severity score, duration of cirrhosis or a worst clinical outcome.
Critically ill cirrhotic patients represent an especially vulnerable population to coagulation abnormalities. Such a vulnerability derives from both long standing morbidities and high prevalence of hemodynamic, metabolic and inflammatory triggers that may determine the appearance of bleeding or thrombosis.
The high prevalence of hemorrhagic events may not be explained in terms of decreased coagulation factors synthesis only, but rather by the complex relationship between poor hepatic reserve and external acute onset triggers.
The history of being under anticoagulation, antiagregation or thrombophrophylaxis is not associated with an increased prevalence of bleeding, and conventional coagulation tests are not useful predictors nor screening tests for bleeding nor thrombotic complications.
The exact prevalence, risk factors and clinical implications of thrombotic episodes in the ICU cannot be assumed to be the ones reported in this work, given the lack of systematic screening of thrombotic complication by ultrasound and tomographic methods. Prospective protocolized studies remain to be done for assessing both the real prevalence and the clinical relevance of thrombotic episodes in critically ill cirrhotic patients.