To investigate the prevalence, related risk factors, and survival of intrahepatic cholangiocarcinoma in a Mexican population.
Material and methodsWe conducted a cross-sectional study at Medica Sur Hospital in Mexico City with approval of the local research ethics committee. We found cases by reviewing all clinical records of inpatients between October 2005 and January 2016 who had been diagnosed with malignant liver tumors. Clinical characteristics and comorbidities were obtained to evaluate the probable risk factors and the Charlson index. The cases were staged based on the TNM staging system for bile duct tumors used by the American Joint Committee on Cancer and median patient survival rates were calculated using the Kaplan-Meier method.
ResultsWe reviewed 233 cases of hepatic cancer. Amongst these, hepatocellular carcinomas represented 19.3% (n = 45), followed by intrahepatic cholangiocarcinomas, which accounted for 7.7% (n = 18). The median age of patients with intrahepatic cholangiocarcinoma was 63 years, and most of them presented with cholestasis and intrahepatic biliary ductal dilation. Unfortunately, 89% (n = 16) of them were in an advanced stage and 80% had multicentric tumors. Median survival was 286 days among patients with advanced stage tumors (25th-75th interquartile range, 174-645 days). No correlation was found between the presence of comorbidities defined by the Charlson index, and survival. We evaluated the presence of definite and probable risk factors for the development of intrahepatic cholangiocarcinoma, that is, smoking, alcohol consumption, and primary sclerosing cholangitis.
DiscussionWe found an overall prevalence of intrahepatic cholangiocarcinoma of 7.7%; unfortunately, these patients were diagnosed at advanced stages. Smoking and primary sclerosing cholangitis were the positive risk factors for its development in this population.
Intrahepatic cholangiocarcinoma (IH-CCA) is the second most common primary hepatic cancer after hepato-cellular carcinoma1 and is associated with high mortality because it mostly presents with advanced stages at diagnosis.2 Most patients present with non-resectable disease at the time of diagnosis and have a median reported survival of 12-36 months.3 The 5-year overall survival rates for patients with stages III and IV cholangiocarcinoma are 10% and 0%, respectively.4 The mortality and incidence of IH-CCA have been reported to be increasing worldwide,5,6 with an overall incidence of 0.71 per 100,000.7,8
In Mexico, there is no information related to the epidemiology of IH-CCA. Established risk factors for IH-CCA are primary sclerosing cholangitis (PSC), parasitic infections, biliary ducts cysts, and hepatolithiasis. These conditions are not common in Mexico. However, conditions such as hepatitis C, hepatitis B, diabetes, obesity, alcohol consumption, cirrhosis, and inflammatory bowel disease have been identified as emerging risk factors.9-11 The contribution of these to IH-CCA in Mexico is unknown. Therefore, the aim of this study was to investigate the prevalence, risk factors, and survival of patients with IH-CCA in a Mexican population.
Material and MethodsStudy designWe conducted a cross-sectional study from October 29, 2005 to January 1, 2016 to analyze the prevalence, related risk factors, and survival rates of patients with IH-CCA at the MedicaSur Hospital in Mexico City. The local research ethics committee approved this study (permit # 2016-EXT-189).
PatientsWe reviewed the clinical records of all inpatients diagnosed with malignant liver tumors. Each of the cases were re-evaluated for histological and staging confirmation, and regardless of any prior diagnosis or record of a discharge from hospital. Tumors that did not meet the histological criteria of IH-CCA were excluded. Staging was performed by an expert oncoradiologist based on the TNM 7 staging system for intrahepatic bile duct tumors of the American Joint Committee on Cancer.12
Data collectionDemographic data, Charlson comorbidity indices, bio-chemistry results, and established and probable risk factors were collected retrospectively. We contacted the relatives of each patient to investigate their clinical status; in cases of death, the date of the event was requested.
Statistical analysesQuantitative variables with normal distribution are expressed as the mean and standard deviation (SD), otherwise are presented as median with interquartile range, 25th-75th percentile. Qualitative results are presented as percentages. We evaluated the probable risk factors and the Charlson index using Pearson's coefficient correlation. Median survival times were calculated using the Kaplan-Meier method. The statistical analyses were performed with Stata 12.0 software.
ResultsIn the 11-year study period, 233 cases of hepatic tumors were identified in our pathology department. Cases of IH-CCA represented 7.7% (18 cases) of the total, and meta-static tumors accounted for 60.9% (142 cases). Hepatocellular carcinomas only accounted for19.3% (45 cases) and other malignant tumors accounted for 12.1% (28 cases) of all hepatic neoplasms.
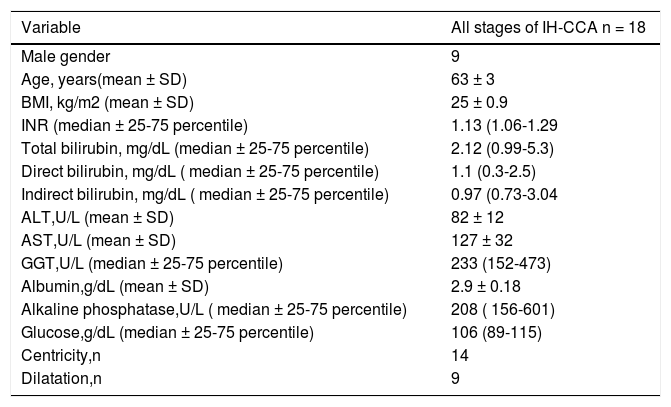
The demographic features and biochemical test results of patients with IH-CCA at the time of diagnosis are listed in table 1. In general, patients presented with biochemical cholestasis and half with clear dilation of the intrahepatic biliary tract. At the time of diagnosis, most patients were in an advanced stage of tumor progression (TNM stage IV A/B), and only two patients were found at stages I and II. About 80% of the patients had multicentric tumors. Fifteen cases were moderately differentiated and three were poorly differentiated.
Baseline characteristics of patients.
| Variable | All stages of IH-CCA n = 18 |
|---|---|
| Male gender | 9 |
| Age, years(mean ± SD) | 63 ± 3 |
| BMI, kg/m2 (mean ± SD) | 25 ± 0.9 |
| INR (median ± 25-75 percentile) | 1.13 (1.06-1.29 |
| Total bilirubin, mg/dL (median ± 25-75 percentile) | 2.12 (0.99-5.3) |
| Direct bilirubin, mg/dL ( median ± 25-75 percentile) | 1.1 (0.3-2.5) |
| Indirect bilirubin, mg/dL ( median ± 25-75 percentile) | 0.97 (0.73-3.04 |
| ALT,U/L (mean ± SD) | 82 ± 12 |
| AST,U/L (mean ± SD) | 127 ± 32 |
| GGT,U/L (median ± 25-75 percentile) | 233 (152-473) |
| Albumin,g/dL (mean ± SD) | 2.9 ± 0.18 |
| Alkaline phosphatase,U/L ( median ± 25-75 percentile) | 208 ( 156-601) |
| Glucose,g/dL (median ± 25-75 percentile) | 106 (89-115) |
| Centricity,n | 14 |
| Dilatation,n | 9 |
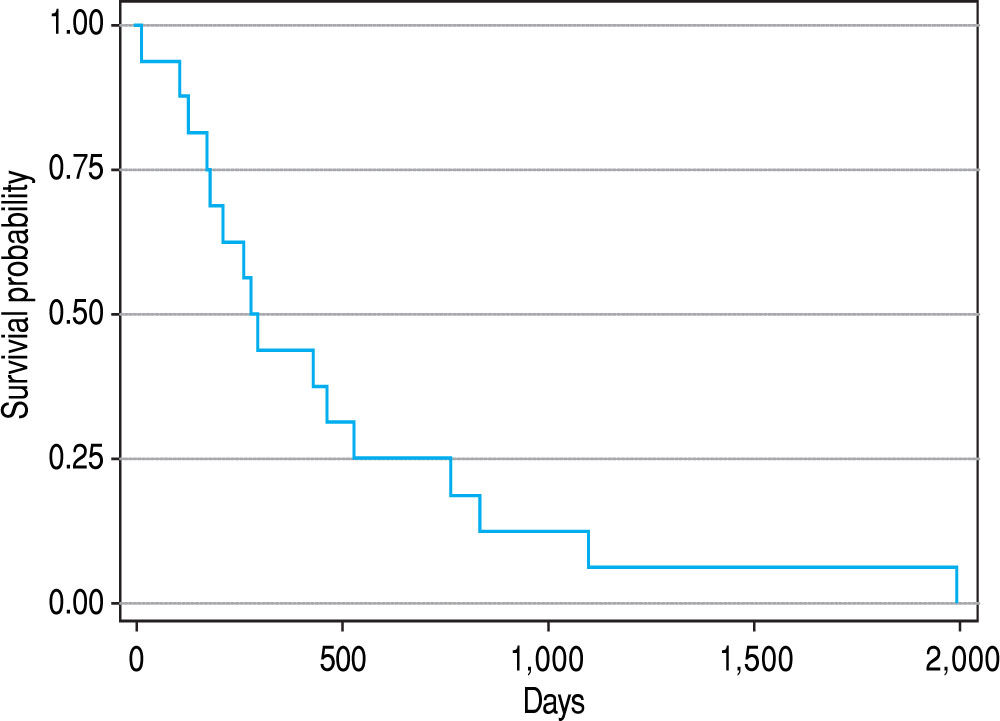
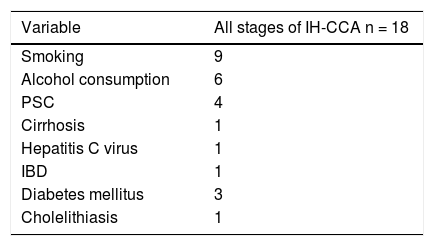
The median survival was 286 days among the 16 patients with TNM stage IVA/B tumors (25th-75th interquartile range, 174-645 days; Figure 1). No correlation was found between the presence of comorbidities by the Charlson index and survival in days (Pearson's correlation coefficient = -0.22). The presence of definite and probable risk factors for the development of IH-CCA was evaluated (Table 2). The most prevalent risk factors in our study group were smoking and PSC.
Among our cases, the prevalence of IH-CCA was 7.7%; most of the patients (89%) were in TNM stage IV with a median survival of 286 days. The global prevalence of IH-CCA reported in the literature is 10-15% of all primary liver malignancies,13 and its incidence has been reported to be increasing in many Western countries.14,15 Age-adjusted rates of this tumor type are reported to be highest in Hispanic and Asian populations (2.8-3.3 per 100,000) and lowest in non-Hispanic white and black people (both 2.1 per 100,000).16 IH-CCA appears to be more prevalent among men in different areas of the world; the incidence ratios of men to women vary between 1.3 among white Americans to 3.3 among the French.17
According to European guidelines,18 the clinical presentation of IH-CCA is nonspecific and insufficient to establish a diagnosis. Consequently, 60% of patients with this disease present with advanced stages that make them unsuitable for curative resection.19 These patients have a median survival of 12 months.18
We found that the main risk factors related with the development of IH-CCA were smoking, alcohol consumption, and PSC. The traditional risk factors for this tumor type are biliary cysts, primary sclerosis, cholangitis (PSC), hepatolithiasis, inflammatory bowel disease, and infections of the biliary tract with Opisthorchis viverrini and Clonorchis sinensis.20 Evidence continues to increase about other risk factors associated with developing IH-CCA, including infections with hepatitis virus types C and B, obesity, type 2 diabetes mellitus, and smoking.20,21 In Mexico, liver fluke infections are not reported, and this indication was not included in our study. The risk of cholangiocarcinoma is higher in areas where fluke infections are common, such as South East Asia. These infections are not endemic in Mexico and therefore we did not examine this indication in our study.22
Our study had several limitations. These are rare tumors, and the sample size was small. The second were obtained retrospectively, and the study was performed in only one private medical center. However, it is important to recognize that this is the first reported study from Mexico to evaluate IH-CCA. It will be necessary to perform prospective studies of suitable size in our country to establish the most prevalent risk factors for early diagnosis, and to increase the chances of successful treatment.
In conclusion, IH-CCA was the second most prevalent primary malignant liver tumor in this Mexican population. It is typically diagnosed at advanced stages, which reduces the patient's chances of survival. We found associations with PSC, smoking, and alcohol consumption; however, further studies are needed to establish the risk factors in our country.
AcknowledgmentsThis study was supported in part by Medica Sur Clinic & Foundation.
Compliance with Ethical Standards- •
Conflict of interest. None of the listed authors have a conflict of interest.
- •
Ethical approval. We were in accordance with the ethical standards of the international and institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. No human intervention was performed.