Background: Autonomic dysfunction has been documented in cirrhosis liver. Its influence on variceal bleed is not known. Aim: To determine the autonomic function amongst variceal bleeders in cirrhosis of the liver.
Materials and methods: Fifty cirrhotics (variceal bleeders: 34) belonging to either sex, Childs B, age more than 15 years and non diabetic constituted the study group. Parasympathetic function tests included valsalva ratio (E:I ratio) and deep breathing test. (Max.-Min. heart rate); sympathetic function included postural fall of B.P and a rise in diastolic B.P. with sustained hand grip. A cirrhotic was considered to have ‘True’ autonomic dysfunction when both parasympathetic and one of the two sympathetic tests were abnormal.
Results: The mean age for men was 39.64 + 10.6 yrs and for women 39.54 + 15.8 yrs. The male female ratio was 3.5:1. Only 10 of the 50 patients (all bleeders) had ‘true’ autonomic dysfunction i.e. 20%. Parasympathetic dysfunction alone was positive in 19 (38%) and sympathetic in 10 patients (20%). The E:I ratio (p < 0.001) and an increase in diastolic B.P. during sustained hand grip (p < 0.04) were significantly positive amongst variceal bleeders.
Conclusion: ‘True’ autonomic dysfunction can predispose a cirrhotic to variceal bleed.
Chronic liver disease is accompanied by several circulatory changes. Hyperdynamic circulatory syndrome is a common feature of advanced cirrhosis.1 It is characterized by splanchnic blood pooling, opening of portal-systemic collaterals, arterial vasodilatation and compensatory increase in blood volume.1,2 The resultant autonomic regulatory system events results in an increase in heart rate and cardiac output and reduced peripheral vascular resistance.1,3-6
The autonomic regulatory system of the splanchnic circulation is complex. In healthy individuals, the splanchnic vascular bed contains a large, highly compliant, venous circulation to an extent of 25% of the blood volume at rest.7 It has been considered as the primary blood volume reservoir for reflex control of cardiovascular homeostasis during exercise.8 This richly innervated vascular bed’s vasoconstriction activity is mediated by α-1 receptor. An impaired autonomic function is expected to lead to impairment of cardiovascular autonomic reflexes and hemodynamic instability.
The prevalence autonomic dysfunction (AD) in cirrhosis has varied from 8% - 80% in different series. Its occurrence is irrespective of the etiology of chronic liver disease: ethanol or non ethanol related.9-14 (Bajaj et al) and increases in parallel with the severity of liver disease. Other factors contributing to AD in cirrhosis include that affecting nerve integrity such as alterations in lipid metabolism, vitamin E deficiency, alcohol consumption, immunologic mechanisms and retention of toxic metabolites.15,16 Vagal dysfunction due to elevated angiotensin II production and sympathetic dysfunction due to blunted responsiveness owing to either a production of weak neurotransmitters or a receptorial & postre-ceptorial defect has been documented.4,17-20 Presence of AD irrespective of the cause is often associated with an adverse prognosis.16,21-23
How does AD influence a bleed? Normally in a healthy individual, following a bleed, primarily there is a reduction in the splanchnic blood pool, and redistribution of the blood into the systemic circulation. This stimulates the cardiovascular responses by increasing the heart rate and blood pressure. In presence of AD, the vasoconstrictive phenomenon of the splanchnic circulation is lost and the secondary cardiovascular responses are ineffective.
In cirrhosis of the liver, there is primarily an increase in splanchnic blood pool. In presence of AD, a variceal bleed will fail to elicit cardiovascular response reflex and in fact may further increase the splanchnic blood pool further increasing the risk of further variceal bleed. To test this hypothesis, we under took a study to determine the risk of variceal bleed and bleed related mortality in cirrhotics with AD, with a basic understanding that the splanchnic vascular bed is richly innervated and is the major site of autonomic regulation during orthostatic stress.
Ethics committee of the Institution had approved the study.
MethodologyFifty patients with cirrhosis liver, both variceal bleeders and non bleeders, belonging to Childs A and B were included in the study.
Patient data included age, gender, duration of illness, etiology of cirrhosis, Childs Turcotte Pugh (CTP) score, grades of esophageal varices and bleed data. All the patients had autonomic function tests. Patients belonging to Childs C, absent esophageal varices, those above the age of 60 and/or with cardiac or respiratory ailment, diabetics and those on digoxin and calcium channel blockers were excluded from the study.
Parasympathetic tests:- a.
Heart rate variation on deep breathing (Expiration: inspiration ratio: E:I Ratio)
The patient is asked to breathe deeply and evenly at a rate of six breaths per minute, i.e. five seconds for inspiration and five seconds for expiration and electrocardiogram is recorded. The ratio of the mean of the longest R-R interval during expiration (E) to the mean of the shortest R-R interval during inspiration (I) is calculated (E: I ratio). A ratio of < 1.1 suggests autonomic dysfunction. This test is a sensitive for diagnosis of cardiac dysautonomia.
- b.
Heart rate response to Valsalva maneuver (Max. - Min. R-R interval)
The subject is asked to blow into a mouthpiece attached to a modified manometer and to hold it at a pressure of 40 mm Hg for 15 seconds while a continuous ECG is recorded. The maneuver is repeated on three occasions with a minute interval between the recordings. The Valsalva ratio is expressed as: longest R-R interval after the maneuver to the shortest R-R Interval during the maneuver. The mean of the three Valsalva ratio is calculated.
- a.
Blood Pressure response to standing
Subject’s blood pressure is recorded in the supine posture and a minute later in the upright posture. The postural fall in blood pressure is taken as the difference between the systolic pressure in the supine and upright posture. The test is repeated on three occasions and the mean calculated.
- b.
Increase in diastolic BP during sustained hand grip
The resting blood pressure of the patient is recorded on three occasions. The patient is then asked to grip an inflatable rubber bag and to apply maximum voluntary pressure possible. The reading during maximum voluntary contraction is noted. The patient is then asked to maintain 30% of maximum voluntary contraction for as long as is possible (minimum upto five minutes). Blood pressure is measured at one minute interval during the handgrip. The result is expressed as the difference between the highest diastolic blood pressure during the handgrip exercise and the mean of the three diastolic blood pressure readings before commencing the handgrip.
A cirrhotic was considered to have ‘true’ AD when both the parasympathetic tests and any one of the sympathetic tests enlisted were positive. For purpose of analysis, the patients were classified as Group I: Variceal bleeders and Group II-Non variceal bleeders. The AD between the two groups was compared.
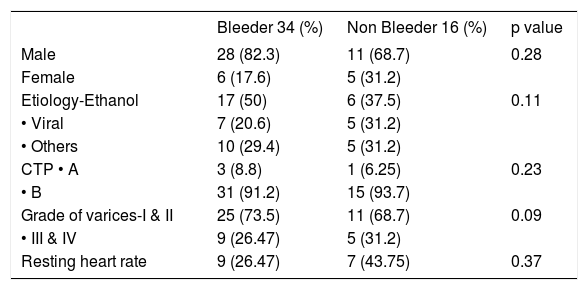
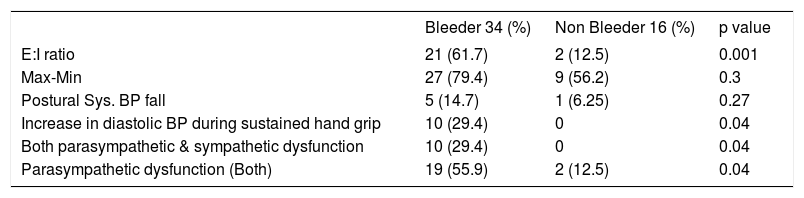
ResultsThere were 39 male and 11 female patients. The mean age for men was 39.64 + 10.6 yrs and for women was 39.54 + 15.8 yrs. There were 34 variceal bleeders (Group I) and 16 non bleeders (Group II). The male female ratio was 3.5:1. TheTable I summarizes the demographic and clinical data.Table II summarizes the autonomic function tests amongst variceal bleeders and non bleeders. The overall prevalence of AD was 20%. In Gp I, 10 patients with variceal bleed i.e. 20% and all were true AD. Isolated parasympathetic dysfunction was present in 19 (38%) and sympathetic in 10 patients (20%). An abnormal E:I ratio was present in 21 (61.7%), Max - Min heart rate abnormality in deep breathing in 27 (79.4%), postural hypotension in 5 (14.7%) and an increase in diastolic B.P. during sustained hand grip in 10 (29.4%) patients. In Gp II, none had true AD. An abnormal E:I ratio was present in 2(12.5%), Max - Min heart rate abnormality in deep breathing in 9 (56.2%), postural hypotension in 1 (6.25%) and none had an increase in diastolic B.P. during sustained hand grip. The E:I ratio (p < 0.001) and an increase in diastolic B.P. during sustained hand grip (p < 0.04) were significantly positive amongst variceal bleeders.
| Bleeder 34 (%) | Non Bleeder 16 (%) | p value | |
|---|---|---|---|
| Male | 28 (82.3) | 11 (68.7) | 0.28 |
| Female | 6 (17.6) | 5 (31.2) | |
| Etiology-Ethanol | 17 (50) | 6 (37.5) | 0.11 |
| • Viral | 7 (20.6) | 5 (31.2) | |
| • Others | 10 (29.4) | 5 (31.2) | |
| CTP • A | 3 (8.8) | 1 (6.25) | 0.23 |
| • B | 31 (91.2) | 15 (93.7) | |
| Grade of varices-I & II | 25 (73.5) | 11 (68.7) | 0.09 |
| • III & IV | 9 (26.47) | 5 (31.2) | |
| Resting heart rate | 9 (26.47) | 7 (43.75) | 0.37 |
| Bleeder 34 (%) | Non Bleeder 16 (%) | p value | |
|---|---|---|---|
| E:I ratio | 21 (61.7) | 2 (12.5) | 0.001 |
| Max-Min | 27 (79.4) | 9 (56.2) | 0.3 |
| Postural Sys. BP fall | 5 (14.7) | 1 (6.25) | 0.27 |
| Increase in diastolic BP during sustained hand grip | 10 (29.4) | 0 | 0.04 |
| Both parasympathetic & sympathetic dysfunction | 10 (29.4) | 0 | 0.04 |
| Parasympathetic dysfunction (Both) | 19 (55.9) | 2 (12.5) | 0.04 |
The present study has shown significant autonomic dysfunction amongst cirrhosis with variceal bleed compared to non bleeders. All the 10 patients (100%) with sympathetic dysfunction and 19 patients (90.4%) with parasympathetic dysfunction had bled. While major emphasis has been laid on the role of sympathetic dysfunction in AD, not much has been highlighted on the role of parasympathetic dysfunction in cirrhosis liver. Studies have documented the role of parasympathetic function in hyperdynamic circulatory syndrome. A sympatho-vagal imbalance with a prevalent parasympathetic dysfunction can result in a defective inhibitory vagal tone on the cardiac pacemaker. This will result in an acceleration of heart rate and an increase in cardiac output along with an enhanced cardiac preload. The tests based on heart rate changes are much more sensitive than those based on blood pressure variations in revealing subtle autonomic defects.24,25 and hence it is not uncommon to document parasympathetic system dysfunction as well in cirrhotic individuals. Also today, it is an established fact that cardiovascular tests mainly those based on heart rate variations are influenced by both branches of the autonomic nervous system and classified as parasympathetic or sympathetic according to the predominant operating branch24
While the cardiovascular tests in the present study showed dual abnormality of both sympathetic and parasympathetic nervous system, the failure of splanchnic vasoconstriction due to sympathetic under activity is the most likely factor that is responsible for splanchnic pooling, predisposing our patients to a high risk of variceal bleed and also for failed endo and pharmacotherapy.
Points to ponder- a)
In the presence of splanchnic vasodilatation, sympathetic dysfunction increases the risk of variceal bleed. What would be the role of ß-blocker and other splanchnic vasoconstrictors in cirrhosis with variceal bleed with AD? This needs to be studied prospectively.
- b)
In the future, it may be necessary to perform autonomic nervous system functions tests during the initial evaluation of patients with cirrhosis liver to predict the outcome of variceal bleed apart from Childs grading and higher grades of varices.
- c)
Liver transplantation-Can this revert the autonomic dysfunction? and studies are showing AN may be associated with a greater surgical risk during LT.
We thank Mr. Vengatesan A, Lecture in Statistics, Clinical Epidemiology Unit, Stanley Medical College Hospital, Chennai