HVH (hepatic vascular hamartoma) is a tumor like malformation arising from the vascular tissue of the liver. HVH has been previously reported in animals and presents distintive features from the most frequent benign tumor like malformation of the liver, the hepatic mesenchymal hamartoma (HMH). Herein we report a case of HVH localized in hepatic segment 4b, involving the gastro hepatic ligament, successfully treated with total excision. We describe the anatomo-pathologic findings focusing on the clinical and radiological presentation, the intraoperative characteristics and the differential diagnosis.
Hamartoma derives from the Greek word “ap,apTia”, Hamartia, and refers to a defect or an error. It is a tumorlike malformation resembling a neoplasm, composed by an overgrowth of indigenous mature cells and tissues which show disorganized architectural pattern with predominance of one of its components.1 Hamartoma can arise from any organ and tissue, in particular, it has been commonly observed in lung, pancreas, spleen, liver and kidney.
In liver hamartomas usually originates from mesenchimal tissue: hepatic mesenchimal hamartoma (HMH) was initially described by Edmondson2 and is generally regarded as the second most common benign liver lesion in children.3
In this article, we describe a case of hepatic hamartoma arising from vascular tissue (hepatic vascular hamartoma, HVH), that to the best of our knowledge has never been reported in human.
Case ReportA 48-year-old female with a history of intermittent right upper abdominal pain was referred to our service. The physical examination and medical history weren’t significant. The laboratory tests, including complete blood count, liver function, serological markers for viral B, C hepatitis and tumoral markers, were within the normal limits. Antiechinococcal antibodies were negative.
On abdominal ultrasound, a 10 cm multiloculated hepatic cyst was reported. A computed tomography scan (Figure 1) and a magnetic resonance imaging showed a multiloculated liver mass, involving the porta haepatis and extending to the IV duodenal portion. Additionally, endoscopic ultrasound confirmed the intrahepatic lesion involving the gastro-hepatic ligament and excluded a vascular compromise; the endoscopic ultrasound-guided fine-needle aspiration was compatible with a benign epithelial tumor.
The surgical resection was planned and a bilateral subcostal laparotomy performed. A heterogeneous, capsulated, 8 cm hepatic mass located in segment 4b was surrounding gallbladder and involving portal vein, right and left hepatic artery and the proper hepatic artery without signs of direct infiltration. The mass depended on the hepatic parenchyma and no communication between hepatic artery, portal vein and the tumor was observed. An accurate dissection of ilar structures, guided by intraoperative cholangiography, was performed and “en block” resection of the involved hepatic segment, gallbladder and the extrahepatic part of the lesion was finally obtained.
The postoperative course was uneventful and the patient was discharged on 8th postoperative day. Currently, the patient is asymptomatic with no evidence of recurrence at 4 years of follow up.
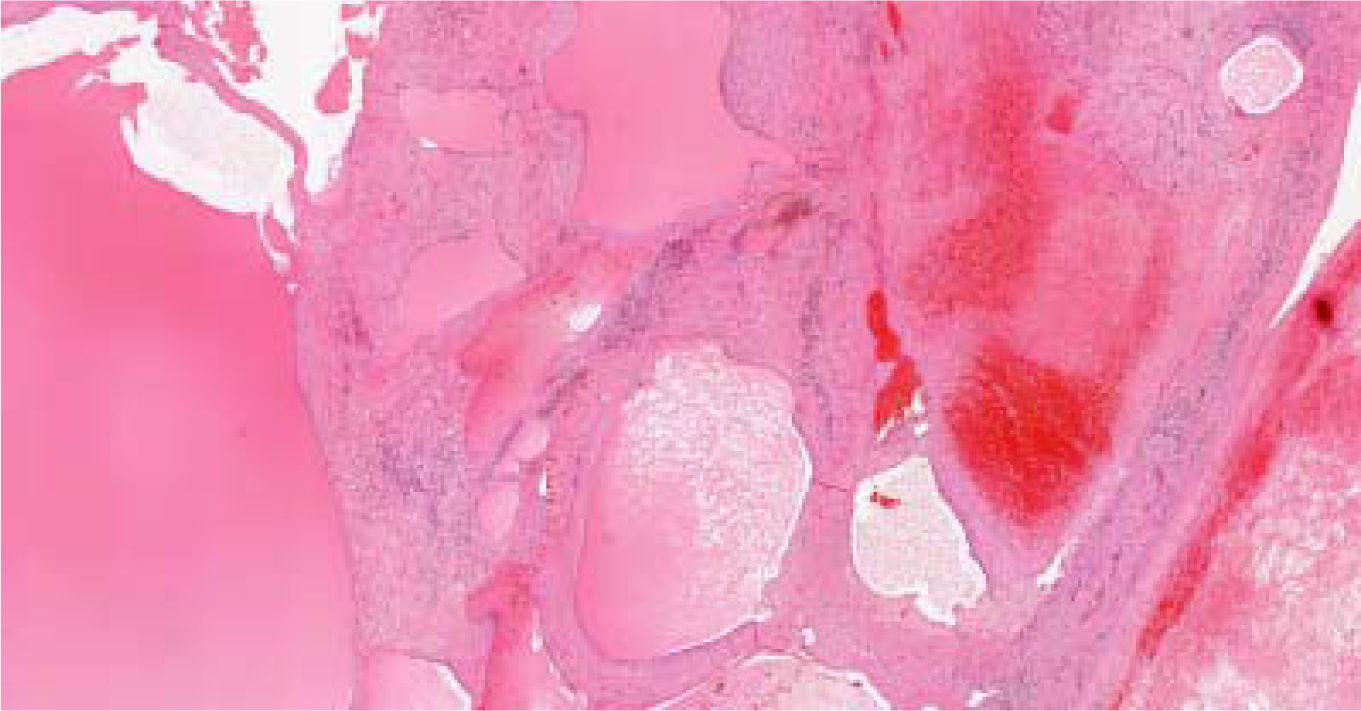
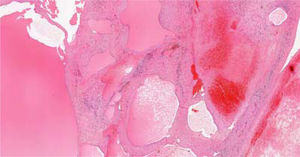
On cut section, a multiloculated cystic mass of cm 7 x 6.9 x 5.9 cm was revealed with cystic spaces contained hematic and necrotic material. The lesion was coated with a smooth membrane compressing the adjacent normal hepatic parenchyma.
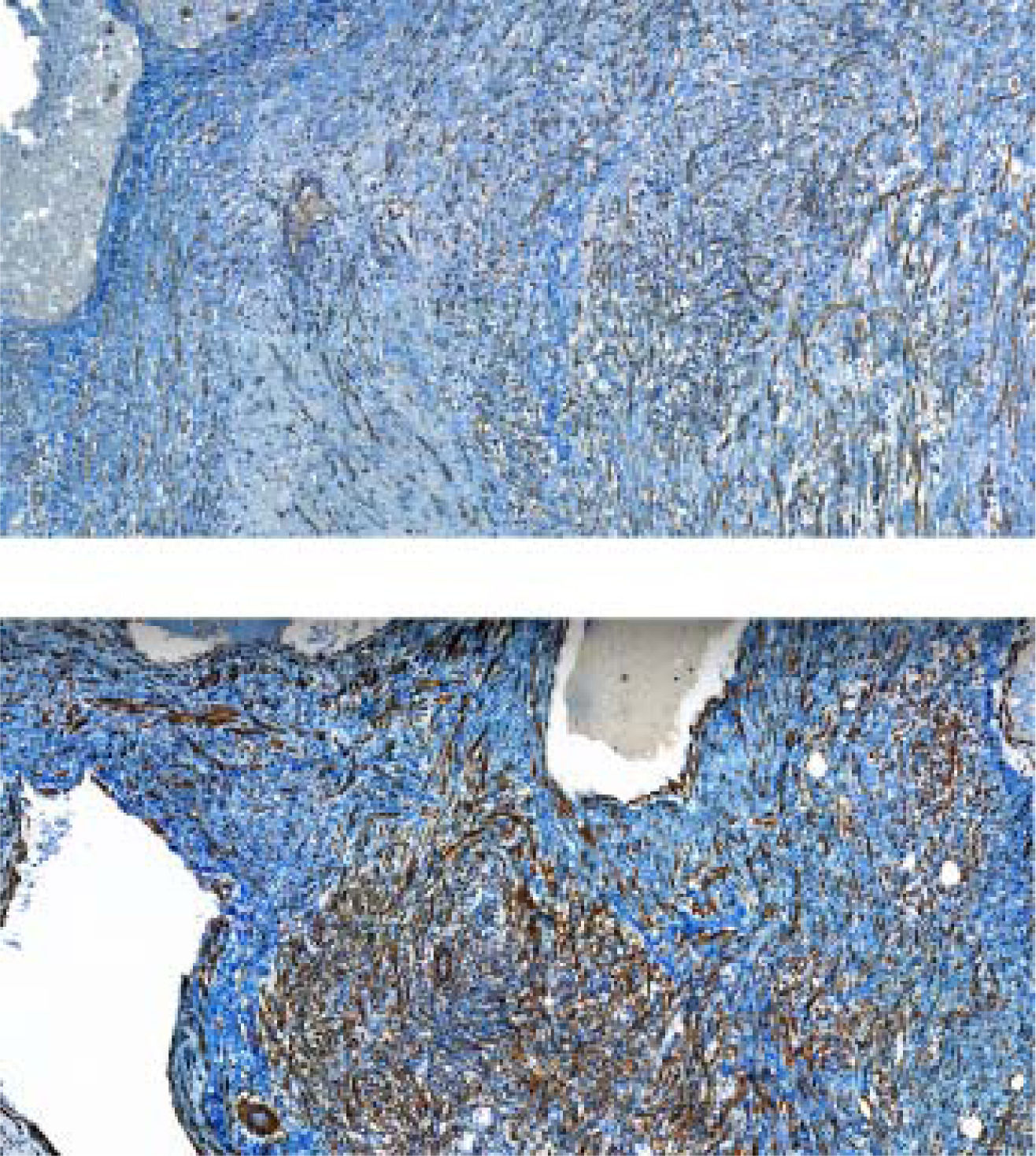
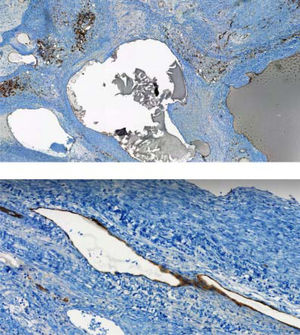
In the hematoxylin eosin stained vascular spaces lined with plump endothelial cells without atypia and the intravascular areas enclosed focal adipose tissue with a connecting network of fibrosis were observed. There were extended areas of necrosis and hemorrhage as well as he-mosiderophages (Figure 2). Mesenchymal, fusiform cells expressing actine and caldesmon delimitated vascular spaces enclosing arteries and veins with different size and shape (Figure 3).
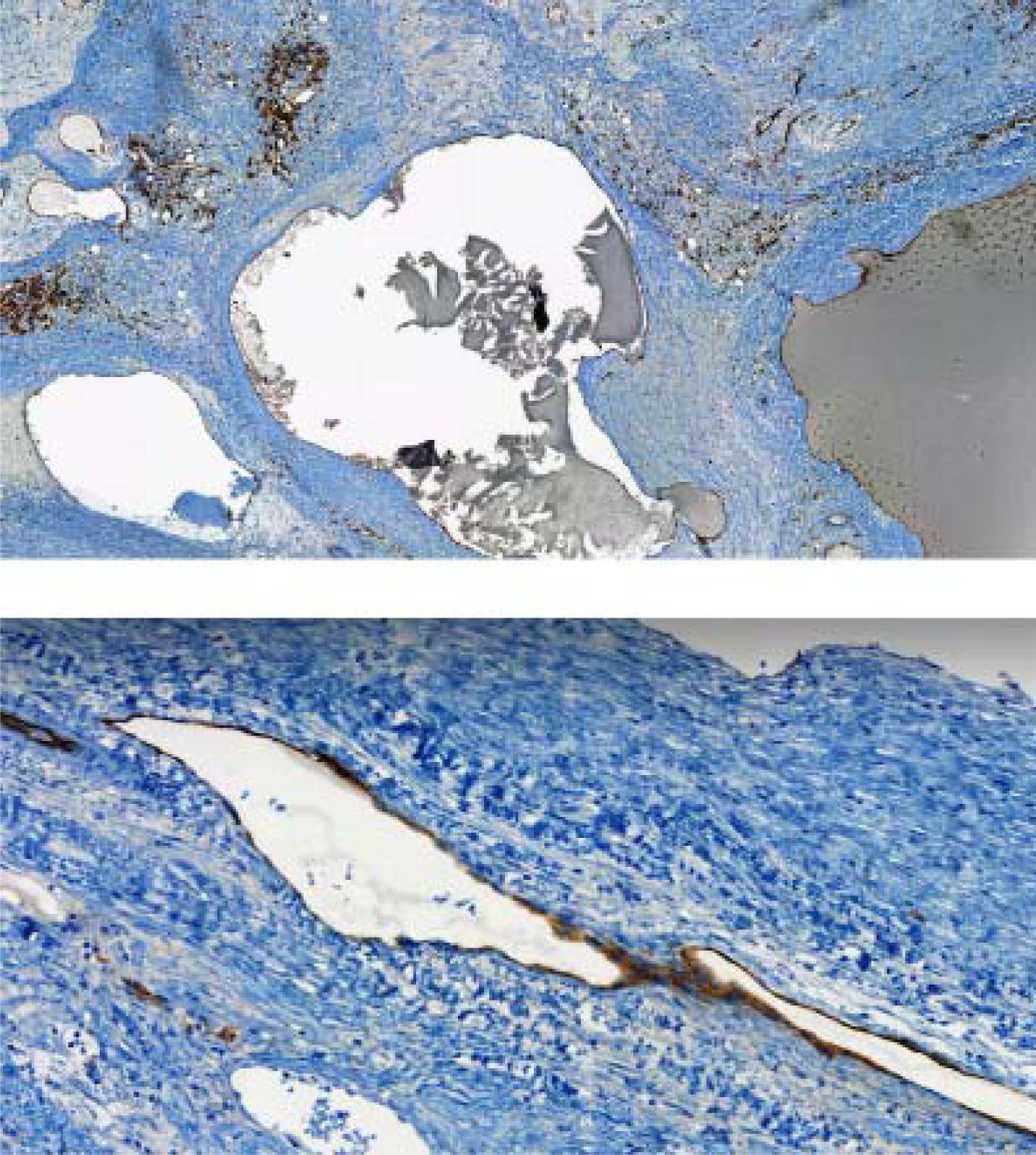
The lining endothelial cells of the vascular channels were positive for CD31 and CD34 immunostain (Figure 4). The final pathological diagnosis was a HVH.
DiscussionHamartoma is a benign, polyclonal lesion derived from an uncontrolled proliferation of cell of the tissue of origin and can arise from any tissue and organ. This tumor-like lesion has been associated with numerous genetic syndromes such as the tuberous sclerosis and the PTEN hamartoma tumor syndrome (PHTS), including Cowden syndrome (CS), Bannayan-Riley-Ruvalcaba syndrome (BRRS) and adult Lhermitte-Duclos disease (LDD).4Hamartoma can be pathologically sub-classified, depending on the relative abundance of a particular endogenous tissue (mesenchimal, vascular, neurovascular, etc.).
In case of vascular hamartoma, normal vascular tissue and blood vessel are arranged in a disorganized structure forming mass and represents congenital defects of vascular formation and development.5
Although uncommon, vascular hamartoma has been described in several organs: in spleen, lung, gastrointestinal tract, mediastinum, lower genital tract, in tongue, paranasal sinus, and parotid gland. As far as we are aware, this is the first case of hepatic vascular hamartoma (HVH) reported in humans, even if several cases have been reported in different animal species such as in dogs,6,7 and cow.8
Differential diagnosis, on the gross and histopathologic finding, includes HMH and hemangioma. Firstly hemangioma shows common histologic findings with vascular hamartoma such as the presence of dilated vascular spaces of varying size, lined by cells without atypia and expressing endothelial markers. Unlike vascular hamartoma, he-magionama’s structure is characterized by a large and compact clonal cell population, while in the case herein reported the histopathological finding is represented by a set of arterial and venous vessels (non-clonal origin) and is accompanied by intralesional adipose tissue. Otherwise, in HVH, blood vessels have a normal structure (endothelium, connective tissue, muscle tissue,5,9 while hemangioma lacks the muscular part of the vessels. Regarding the second differential diagnosis, the hepatic mesenchymal hamartoma, this tumor originates from mesenchimal tissues and can appear as a solid or cystic lesion.10 Histological, HMV consists of malformed bile ducts included in a fibromyxoid stroma. Epithelial-lined cysts, and foci of nonepithelial-lined cystic spaces within the stroma (which may resemble lymphangioma), and entrapped islands of otherwise normal-appearing hepatocytes have also been described.11 In vascular hamartoma neither biliar element not hepatocytes are present.
In most cases vascular hamartoma is asymptomatic or associated with only minor symptoms, depending on the localization.5 In the case of splenic vascular hamartoma only 20% of the lesion are able to manifest clinical symptoms, such as palpable mass, spontaneous rupture with intra-abdominal bleeding, and hypersplenism (thrombocytopenia, anemia, pancytopenia.9,12 In lung most pulmonary vascular hamartoma is nonexpanding or slowly growing neoplasms, but some authors believe that surgery is necessary when expansion is detected or accompanying by pulmonary symptoms. In fact, in some cases, a malignant behavior, such as invasion of pulmonary arteries and esophagus has been described.13
Despite the benign nature, even for hepatic vascular hamartoma, a strict follow up and an early surgery can be recommended to avoid an uncontrolled growth of the lesion with functional damage of the organ involved or severe bleeding complications.
ConclusionIn conclusion, hepatic vascular hamartoma is a benign vascular proliferation with the characteristic positive im-munophenotype of the lining endothelial cells. In this case report, we describe the first case of hepatic vascular hamartoma ever reported in human. Although this tumor is very rare, it must be included in the differential diagnosis of hepatic mass-forming lesions; it is essential to be able to recognize HVH to learn more about its natural history and response to treatment.
Abbreviations- •
BRRS: Bannayan-Riley-Ruvalcaba syndrome.
- •
CS: Cowden syndrome.
- •
HMH: hepatic mesenchimal hamartoma.
- •
HVH: hepatic vascular hamartoma.
- •
LDD: Lhermitte-Duclos disease.
- •
PHTS: PTEN hamartoma tumor syndrome.
The authors declares that there is no conflict of interest regarding the publication of this article.