We describe the case of a four-year-old girl admitted to our hospital to attend a specific oral tolerance induction (SOTI) to wheat. She was born at term, without perinatal problems. On the second day of life, she developed a perioral dermatitis that worsened during the following days into a scaling eczema localised on face, neck and skin folds. Because of this her diet was changed from cow's milk to soy formula. Specific IgE result was positive for cow's milk 6.61kUA/L, egg white 30.6kUA/L and wheat 67kUA/L, so these foods were never introduced into her diet.
Later on she experienced two severe allergic reactions, characterised by urticaria, abdominal pain with or without vomiting and bronchospasm, due to accidental ingestion of a very small amount of wheat.
When she was first evaluated in our department she presented total alopecia with seborrhoeic dermatitis of the scalp. Her dermatitis was extremely severe involving the entire body (Fig. 1). We decided to treat strongly the skin and then, after a good improvement, to try a SOTI for wheat.1
On the day of admission she was in good clinical condition; her weight was just below the 3rd percentile, her height in the 10th percentile for age.
On physical examination she had downy, short, brittle hair, and sparse eye brows especially laterally. The skin showed good improvement compared to prior evaluation, but an erythematous desquamating eczema was evident on the eyelids, arms, trunk and legs. Teeth, nails and mucous membranes were normal.
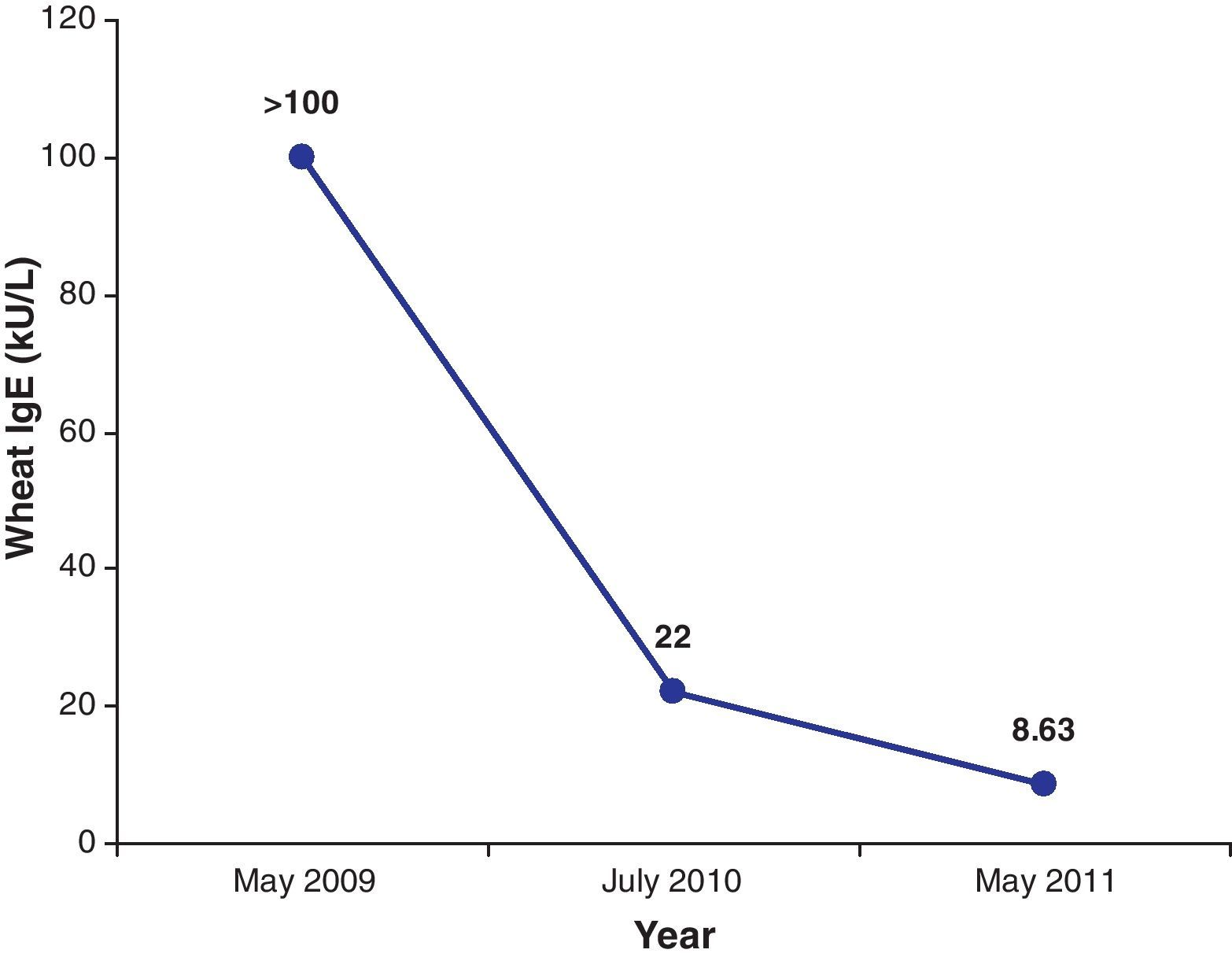
Laboratory investigations showed high levels of eosinophils (930/μL, normal values 0–3500/μL), high serum level of total IgE (9436mg/dL, normal values 0–52UI/mL) with wheat-specific and milk-specific IgE>100kUA/L.
Based on clinical history and physical signs we hypothesized a Netherton syndrome.2 Scalp hair examination on light microscopy showed typical bamboo deformity of trichorrhexis invaginata (Fig. 2) suggestive of Netherton syndrome. Genetic analysis established this diagnosis, showing mutations in the gene SPINK5.
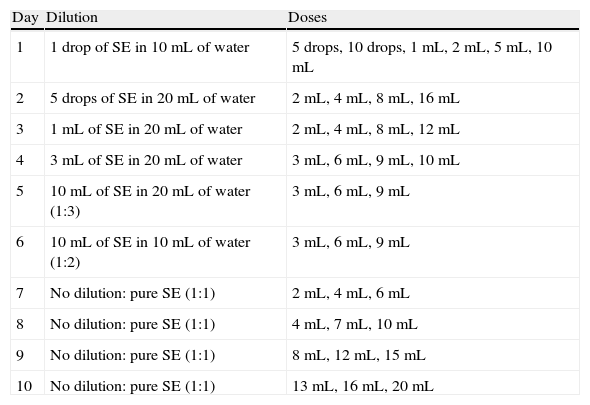
Wheat SOTI was performed using semolina. The process consisted in a rapid increase of dosage, starting with very low amounts of diluted semolina, as previously described for milk (Table 1). During hospital admission, she was administered an antihistaminic daily (cetirizine, 1gtt/2kg per day), she had a venous line placed and a complete emergency kit was always available.
In-hospital treatment schedule: rush phase. Doses were administered at 1-h intervals on the first day and at 2-h intervals on subsequent days (from the second to the 10th day).
| Day | Dilution | Doses |
| 1 | 1 drop of SE in 10mL of water | 5 drops, 10 drops, 1mL, 2mL, 5mL, 10mL |
| 2 | 5 drops of SE in 20mL of water | 2mL, 4mL, 8mL, 16mL |
| 3 | 1mL of SE in 20mL of water | 2mL, 4mL, 8mL, 12mL |
| 4 | 3mL of SE in 20mL of water | 3mL, 6mL, 9mL, 10mL |
| 5 | 10mL of SE in 20mL of water (1:3) | 3mL, 6mL, 9mL |
| 6 | 10mL of SE in 10mL of water (1:2) | 3mL, 6mL, 9mL |
| 7 | No dilution: pure SE (1:1) | 2mL, 4mL, 6mL |
| 8 | No dilution: pure SE (1:1) | 4mL, 7mL, 10mL |
| 9 | No dilution: pure SE (1:1) | 8mL, 12mL, 15mL |
| 10 | No dilution: pure SE (1:1) | 13mL, 16mL, 20mL |
SE: semolina.
At 15mL of pure semolina she presented bronchospasm and urticaria, with a complete recovery of symptoms using nebulised epinephrine (1mg/10kg diluted in 3mL of saline solution). Semolina dosage was temporarily decreased (8mL), but on the last day of admission (11th day) she was able to tolerate 20mL of pure semolina without any allergic reactions occurring. Afterwards the desensitisation treatment continued at home until she was able to take 150mL of semolina as a single dose, without adverse reactions. An appropriate training to manage adverse reactions, including the use of nebulised and self-injectable epinephrine was provided to the girl's parents. We recommended avoiding physical exercise for 3h after semolina intake to minimise the risk of food/exercise-induced anaphylaxis. Antihistamine treatment was continued at home until the 150mL was reached and then reduced over four weeks.3
After one year she was able to ingest cereals without any restrictions. On the way, she experienced some mild allergic reactions but never life-threatening events.
At this point the girl was newly hospitalised for an attempt to specific oral tolerance induction to cow's milk proteins. Wheat-specific IgE were significantly reduced (22kUA/L), whereas IgE for milk and egg were still very high (>100kUA/L).
At the moment SOTI for milk allowed to reach the dose of 60mL of pure milk after eight months with two moderate respiratory and cutaneous reactions treated with nebulised adrenaline. An unrestricted diet for wheat is maintained without any problem and wheat-specific IgE are 8.63kUA/L.
To the best of our knowledge, this is the first case in the literature of successfully SOTI in a child affected by Netherton syndrome.
Netherton syndrome is an autosomal recessive disorder of cornification characterised by congenital ichthyosiform erythroderma or ichthyosis linearis circumflexa4, trichorrhexis invaginata or other hair shaft anomalies, and atopic diathesis. The erythroderma is often intensified after infection. Infants may suffer from failure to thrive, recurrent bacterial and candidal infections, and marked hypernatremic dehydration. The most frequent allergic manifestations are urticaria, angio-oedema, atopic dermatitis, and asthma.
The first take home message of this report is that Netherton syndrome should be suspected in any child with severe eczema developing in the first days of life, abnormal hair growth, and severe food allergies especially in the case of high levels of specific IgE. The light microscopy allows to identify the characteristic hair abnormality suggestive of this disease.
Furthermore, the improving outcome of our case enhances the role of SOTI also in patients in which allergy is part of a genetically determined condition. This optimal result suggests that desensitisation trials might be successfully applied in patients affected by severe congenital atopies although their condition is genetically determined.
Conflict of interestEvery author contributed to this work. No author is US, UK, Canadian or Australian Government employee or contractor. We declare no conflict of interest. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript.