Some myths and unsupported beliefs about asthma are very popular and enjoy general public acceptance and fairly strong support on the Internet. Onions for cough; dairy products avoidance for asthma; and some other popular myths are reviewed, along with some other medical and mixed (popular and medical) myths comparing their popular and scientific support. Classifying medical statements as realities or unsupported beliefs is a hard and serious work nowadays addressed by Evidence Based Medicine methods, which are not devoid of the influence of medical fashion: the medical community is more prone to accept fashionable statements compared to non-fashionable or old-fashioned statements.
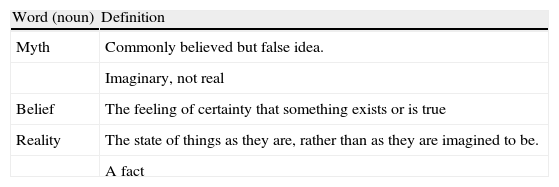
My primary school teachers taught me that there is no better way to find out a good definition than to look it up in a good dictionary. Table 1 presents the definitions of myth, belief, and reality offered by the Cambridge Advanced Learners Dictionary. From these definitions we may conclude that the word myth refers to statements that are not true (or that are considered not to be true) in contrast with reality, which are statements considered to be true. The word belief in English does not imply that the idea in which we believe is not true, but in the medical setting, popular beliefs refer to widely-held beliefs that may not be true. So, there is a radical difference between myths and reality: the same that there is between what is true and what is false.
Word definitions offered by Cambridge Advanced Learners Dictionary.
| Word (noun) | Definition |
| Myth | Commonly believed but false idea. |
| Imaginary, not real | |
| Belief | The feeling of certainty that something exists or is true |
| Reality | The state of things as they are, rather than as they are imagined to be. |
| A fact |
However, despite this apparent radical difference, myths and reality are not closed and definitive concepts. As paediatricians, we can easily remember a lot of statements about diagnostic tools, drug treatments and even pathophysiological concepts that we were taught during our early training as realities that current knowledge has discarded and labelled as unsupported beliefs or even myths. Reading textbooks of Medicine only 10–15 years old may be a good vaccine against the false belief or myth that today's realities are, actually and definitely, realities. Our successors and our successors’ successors will surely discard many of them, as we have done with most of our predecessors’ beliefs.
It is precisely this activity of classifying statements as realities or unsupported beliefs which constitutes the hard core of Science. In biomedical Sciences, Evidence Based Medicine (EBM) constitutes the standard method to verify if something (a medical issue) does have enough supporting data to be considered or not as a reality (at least temporarily). The word used in English to refer to this supporting data is evidence (a noun, uncountable), which is usually and erroneously translated into Spanish as evidencia. However, the Spanish word evidencia does not mean evidence, but something that is so obviously true that no one can have the slightest doubt about it. Although this wrong translation is clearly distorting the scope and meaning of Evidence Based Medicine in many native Spanish speaking doctors, this approach has gained general acceptance all over the world, including in Spanish speaking countries and nowadays constitutes the final method to reach a decision about any medical statement.
I do declare that it is not my intention in this paper to formally analyse the supporting data of the myths that I am going to address with an EBM approach. So, all my statements on these issues will be based on the most humble of available evidence: my own opinion. Accordingly, their value is limited, very, very limited.
Taking into account their origin, myths and unsupported beliefs can be classified as popular, when their origin and development come from popular and folk grounds, professional or medical, when originated and maintained in professional grounds, and mixed. Popular myths are easier to approach, because their falseness is more prominent, at least for the medical professional. Medical myths, on the other hand, are more difficult to address because it may be painful for the honest doctor to admit that a long-held belief about something turns out to be a myth and it may also produce long discussions among professionals. Finally, mixed myths are usually the most difficult to combat, because, although having popular origin, they also have long and strong roots in doctors’ beliefs (doctors who, incidentally, are part of the people that created those mixed myths). Some of the most important myths and unsupported beliefs in the field of asthma, paediatric respiratory medicine and allergy are the following:
Popular unsupported beliefsIt is not my intention to ridicule these beliefs or to make fun of the persons that honestly believe in and maintain them. They usually are witty, funny (in both senses), but false (or at least, devoid of the slightest supporting evidence). They do not deserve contempt, but gentle and affectionate education efforts.
Onions are good for coughThis is one of the most widely held popular beliefs in Spain. It states that onions have cough suppressing properties. This therapy is usually administered by laying a dish with an onion cut in two or more parts on the child's bedside table. Onions would exert their action by means of their vapours which would contain chemicals with therapeutic properties when inhaled. As with most popular beliefs, its efficacy is assessed by personal experience, which is heavily influenced by how much the evaluator believes in the intervention. A mother (the evaluator) with faith enough in the intervention to put a fairly good dish of onions on her child's bedside table would probably be very prone to a positive assessment of its efficacy (enthusiasm bias). As expert's opinion (in this case, mothers’ opinion) is the lowest of the degrees of evidence, we looked for more appropriate evidence making a simple search in secondary sources. Neither systematic reviews nor meta-analysis on the issue were found. A search on primary sources looking for randomised double-blind clinical trials yielded no study of quality, and to be honest, no clinical study at all on the issue. Using technical language, we could conclude that there is not enough evidence to support (or discard) its efficacy and that more well-designed and appropriately powered clinical studies are needed to reach a conclusion. Appropriately designed studies should address unique methodological problems, mainly double-blinding, which would need innovative design methods to solve them.
For the sake of completeness, we made a search in general browsers on the Internet using as key words “onions for cough” in Spanish, French and English. The results were astonishing: thousands of web pages in each language address this issue, almost every one reporting positive results with oniontherapy. There are detailed descriptions of how it is used (cut in two, four or more pieces or chopped, that is, a standard dose ranging question), its safety in infants and toddlers (a standard question of age limits and off-label use in paediatrics), some associated inconveniencies (a fairly peculiar scent in the child's room, that is, a standard adverse events issue) and some explanations of its efficacy (standard pharmacokinetic and pharmacodynamics questions). Web pages in Spanish and French focus on the aforementioned described inhaled oniontherapy while English web pages focus in per os oniontherapy with onion syrup, made with onion, sugar, vinegar (optional) and water. Delicious!
Although I insist in my relativist approach when classifying beliefs in myths or realities, oniontherapy may be considered a paradigm of unsupported popular belief devoid of any scientific evidence. However, it can also be considered a harmless intervention (although with the same weak degree of evidence) in as much it does not substitute for appropriate medical care.
Dairy products produce phlegm and make asthma worseThis approach is used commonly by alternative medicine practitioners and it is loosely based in “milk allergy” as asthma trigger. These practitioners recommend their patients to use soya or other vegetable drinks instead of milk. As oniontherapy, it lacks any scientific support but enjoys strong support on the Internet.
Exercise is too risky for asthma and must be avoidedLargely influenced by film stereotypes and despite large educational efforts of most asthma management programmes many parents keep on trying to avoid asthma symptoms by avoiding one of their triggers: exercise. It is true that exercise may exacerbate asthma but it is the only asthma trigger that must not be avoided. Exercise is part of normal life for children and it is important for normal growth and development. With appropriate physical training and drug treatment most asthmatic children can enjoy exercise without problems. A large proportion of elite athletes and players suffer asthma and this condition does not preclude them to achieve very high sport standards. With appropriate counselling, most parents will let their asthmatic children perform their favourite sports at the level of their choice.
Medical and mixed mythsThis is a real minefield. Contrary to popular beliefs, medical and mixed myths have some degree of supporting evidence, although usually outdated. Many honest colleagues may still believe in them, thus making it difficult to completely discard them. Even new, fashionable statements may be devoid of appropriate evidence and could be considered as unsupported beliefs. It is in this field in which scientific relativism becomes more and more important. Some of the most used asthma drugs 10 to 20 years ago (nedocromil, cromolyn) are now considered almost useless. So, it is possible that many of our therapeutic and even pathophysiological concepts will eventually be considered old myths. So, let's be modest!
Short acting beta agonists are not effective in infants and toddlersThis myth is based in two arguments: early studies that found no or few beta receptors in bronchial smooth muscle of infants and toddlers and the failure to find a significant clinical effect of beta agonists in bronchiolitis. However, it is now well known that beta receptors do exist in bronchial smooth muscle of infants and toddlers and that, with the important exception of bronchiolitis, beta agonists are the cornerstone of treatment of acute episodes of preschool and infant wheezing disorders.
Ipratropium bromide is especially effective in infants and toddlersThis statement is based upon physiological reasoning: cholinergic receptors blockade produces bronchodilation and decrease bronchial glandular secretion. Taking into account that in infants and toddlers the most important component of bronchial obstruction would be occupation of bronchial lumen by mucus (more than contracture of bronchial muscle and swelling of bronchial mucosa), anticholinergic agents would be especially effective in this setting. Although this argument is apparently convincing, evidence coming from randomised clinical trials does not support it. Ipratropium bromide has a limited value in the treatment of acute exacerbation of wheezing disorders when used with short acting beta agonists, slightly reducing the hospitalisation risk, but not especially in infants and toddlers. We may conclude that the aforementioned statement is not supported by appropriate evidence.
Daycare attendance reduces the risk of recurrent wheezingThis is a tricky issue, in which epidemiological data are confronted with common sense data. Epidemiological data suggest that daycare attendance may reduce the risk of asthma in school age. Some other epidemiological data suggest that early exposure to respiratory infections may be protective to the development of atopic asthma. These data are at the base of the Hygiene hypothesis, and have been misinterpreted as if daycare attendance were good for wheezing children to avoid future asthma development. However, it is common knowledge and common experience that the main trigger of wheezing exacerbation in toddlers and preschool children are respiratory infections, mainly viral. Children attending daycare suffer more respiratory infections than those raised at home and sometimes it may be wise avoid daycare attendance of children with very frequent wheezing exacerbations related to viral infection, not to diminish the risk of future asthma, but to offer the child some months without an excessive number of colds and reduce the number of wheezing episodes.
Food allergy is a common cause of recurrent wheeze in infants and toddlersAny recurrent ailment is easily and arbitrarily attributed to allergy. Parents of children with recurrent wheeze usually accept uncritically this diagnosis and they believe more easily in allergy than in viral infections. As allergy to aeroallergens is rare at this age, food allergy has been frequently considered as a cause of recurrent wheeze and skin prick test and specific IgE measurement in blood to several common foods have been frequently ordered in this group of children in order to find a causative agent. Recurrent wheeze is not produced by food allergy. Children with food allergy may wheeze when they are exposed to offending food, but this is different to the standard wheezing child who wheezes when they suffer a viral infection. Should food allergy be the cause of their wheeze, they would only wheeze when exposed to the offending food, and every time they were exposed. This clinical association is extremely rare and searching for food allergy in this setting is only confusing for the parents and the doctor.
Allergy to their own respiratory tract bacteria is a common cause of infant and preschool wheezingThe concept of allergy to their own respiratory tract bacteria as a cause of infant and preschool children wheeze was widespread in Spain in the 1970s and 1980s. It was based upon the fact that many of these children had reportedly positive skin prick test to bacterial hydrolysates. Allergy vaccines against their own bacteria were commonly prescribed and thousands of children received this special form of allergy shots, with apparent excellent results, for many years. Today, this concept and this form of therapy have been abandoned. Their apparent benefit probably reflects the natural history of preschool wheeze although this treatment approach has never been properly evaluated. I doubt it really deserves it.
Having pets at home increases the risk of future allergy and asthmaAs pets allergens are common asthma triggers, we thought that having pets at home from the very new born period increased the risk of developing allergy and asthma. However, many studies have shown that the degree of exposure to common allergens does not necessarily increase the risk of developing asthma and that, in fact, sometimes it seems even to be protective. This is also one of the cornerstones of the Hygiene hypothesis: early contact with relevant allergens may foster tolerance instead of allergy. So, we must no longer recommend avoiding contact with pets as a primary prevention measure. Of course, in children with asthma and allergy to pets allergens, pet avoidance is reasonable.
Asthma begins in the first years of lifeLike many other paediatricians, I must admit that I was wrong. For many years I have been teaching that most infants and preschool children with recurrent wheeze had asthma, defined on clinical grounds as recurrent episodes of wheezing, breathlessness, chest tightness and coughing, when other causes have been discarded. One of the most important developments in recent months has been the definitive dismissal of the term asthma below the age of six. An ERS task force has recently published evidence based guidelines on the diagnosis and treatment of preschool wheeze and they definitely do not recommend the use of the term asthma below the age of six, because there is not enough evidence on the inflammatory nature of this condition at this age.1 Taking into account that the reluctance to use the term asthma in preschool children is only related to the first sentence of the current GINA definition of asthma (pathological and molecular biology component), an alternative working definition of preschool wheeze, according to the arguments of the aforementioned working group would be the following:
“Preschool wheeze may be a non-chronic or non-inflammatory disorder of the airways in which no cell or cellular element play any role. This non-chronic or non-inflammatory disorder is associated with airway hyperresponsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread, but variable, airflow obstruction within the lung that is often reversible either spontaneously or with treatment”.
So, recurrent wheeze in preschool children is no longer asthma. Despite the fact that it is heavily epidemiologically linked to childhood and adult asthma in most prospective epidemiological cohort studies, it is not asthma. Despite the fact that every drug used in its treatment is also used as asthma treatment in older children and adults, it is not asthma. Despite the fact that most studies on this condition bear the word asthma in their title, it is not asthma. Despite all these apparent arguments, it is not asthma; it is only recurrent wheeze (and may be, recurrent cough, recurrent breathlessness, recurrent fever, recurrent malaise, and so on). So, the myth of preschool and infant asthma is over.
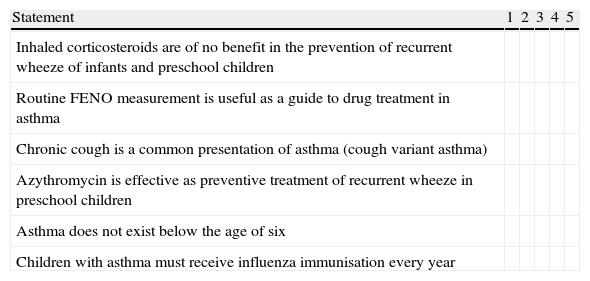
Myths and scientific fashionDoctors and scientists are human beings and are also prone to fashion. Inexplicably, they are prone to happily admit some fashionable statements and to reject some other non-fashionable statements. Fashionable statements are usually enthusiastically accepted despite being devoid of appropriate evidence. For instance, the routine use of FENO as a guide to drug treatment in asthma has been promoted and accepted by the medical audience despite the fact that no study has ever shown that this strategy is any better than using clinical and lung function data when properly assessed by appropriate primary endpoints. On the other hand, the statement that inhaled corticosteroids were almost useless in viral preschool wheeze has been common place for the last years, despite the fact that a good deal of evidence exists supporting their benefits.2 Some old-fashioned drugs, like ketotifen, have also been discarded despite the existence of positive systematic reviews.3 We doctors are human, and prone to fashion. And fashion changes and statements that today we considered as being highly fashionable and true, may eventually turn out to be real myths in some years. I propose you a simple game. Table 2 includes some statements which you have to judge as myths or realities, based on the evidence that, in your opinion, supports them. Try it again in three or four years, and I assure you that you may laugh at the changes.
Some statements which you have to judge as myths or realities.
| Statement | 1 | 2 | 3 | 4 | 5 |
| Inhaled corticosteroids are of no benefit in the prevention of recurrent wheeze of infants and preschool children | |||||
| Routine FENO measurement is useful as a guide to drug treatment in asthma | |||||
| Chronic cough is a common presentation of asthma (cough variant asthma) | |||||
| Azythromycin is effective as preventive treatment of recurrent wheeze in preschool children | |||||
| Asthma does not exist below the age of six | |||||
| Children with asthma must receive influenza immunisation every year |
Mark with an X.
1:It is actually a myth.
2:It seems to be a myth.
3:I am not sure.
4:It seems a fact.
5:It is actually a fact.
The authors have no conflict of interest to declare.