In this issue of Allergologia et Immunopathologia, Esenboga et al. present a retrospective study on information, training and epinephrine autoinjector use.1 They found that patients/parents lacked information and training, and autoinjectors were not used properly when needed.
Only 44/190, i.e., 23 % of children and adolescents prescribed an autoinjector had an anaphylactic reaction during a five-year period. Fleischer et al.2 found that 367/512 subjects (72 %) reacted in their follow-up study over three years (mean), compared to 44/190 (Chi square, two tailed p<0.0001), i.e., 23 % in the Esenboga et al. study.1 The discrepancy in reaction rate indicates a possible difference in indications for prescription.
In most cases, the injection was performed by a physician (31/44) or by parents (10/44) and in only three cases by the child/adolescent. Ten of the 13 children/parents did not use the autoinjector correctly. Training was provided by allergy nurses (42 %) or by an allergy specialist (35 %). Only 37 % of patients/parents felt confident about using the EAI, similar to Topal et al. (39 %).3 Interestingly, Topal et al.3 reported a significant relation between feeling competent using the autoinjector and regular allergy visits (p=0.010), believing that it is necessary to have an adrenaline autoinjector (p=0.003), and previous history of severe anaphylaxis (p=0.010). Autoinjector competency score decreased as time elapsed from the last visit (p=0.002) and the first instruction (p=0.01). Regular visits (p=0.009) and history of severe anaphylaxis (p=0.007) were found as independent factors having an effect on adrenaline autoinjector competency.
These data indicate that good contact between personnel and patient/parents is of utmost importance, for the correct use of epinephrine autoinjectors. However, Topal et al.3 did not investigate the influence of these factors on the fear and anxiety of patients and parents, which is important. An important finding by Esenboga et al.1 is that both parents and children did not inject for fear of the pain caused by the injection.
This aspect has been touched upon by a project4,5 set up in the region of Dalecarlia in central Sweden. The hypothesis was to reduce anxiety about the injection, thereby increasing self-administration of adrenaline by children, adolescents and by parents to small children and this would increase the number of children receiving adrenaline in the community. The project included all kinds of health care personnel in the district, such as paediatric allergists, allergy nurses, school health care nurses, pharmacists, ambulatory allergy consultants, and local specialists in general medicine.
To increase confidence, reduce fear and increase the use of autoinjectors in acute situations individual instruction and training was instituted, videos, and most importantly, before the patient obtained an autoinjector prescription, all children and adolescents must inject themselves with an active autoinjector in the office of the allergist. In the case of young children, the parent was instructed how to use a training autoinjector and then to use an active autoinjector on themselves. The autoinjector used can be one with a low dose and a short needle, since the aim is to overcome fear, not to treat anaphylaxis.
The Dalecarlia project4,5 has been successful for many years and is officially promoted by the Allergy Section of the Swedish Society on Paediatric Allergology and is available on the net.4
In a short communication, the group summarizes its results. The numbers presented are low, 15 children. The group was concerned that the training sessions with active substance would increase rather than decrease the anxiety level. This seemed not to be the case.
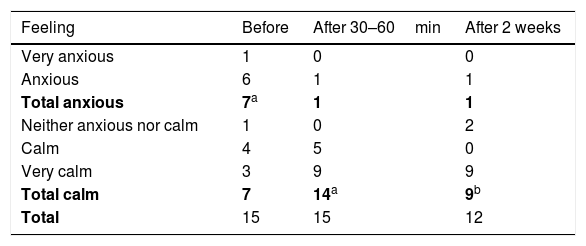
However, as perceived by children/parents, the anxiety was substantially reduced directly after the injection by child or parent (p<0.014, Fischer exact test, two-tailed), Table 1. The anxiety levels decreased after the injection, and all individuals felt good about the training session.5 One child was singled out as being very anxious and needed special attention.
Feelings about using self-administrated epinephrine answered before injection, 30–60min after injection and two weeks after injection After Hellström et al.5
Hellström et al.5 concluded that using epinephrine autoinjectors in training sessions is well received, reduces anxiety and can be used to identify individuals fearful of using an autoinjector.
In conclusion, a truthful relation between the family members, the allergist and the allergists team must be the basis. Training in self-administration is necessary to overcome the fear that it is destructive and can be life-threatening.
Personally, I have used the concept since 1990, with very positive experience.6 However, the documentation of the value of this approach is limited and further studies are needed for proper evaluation of the method.
FundingNone.
Financial disclosureNothing to disclose.
Conflicts of interestsSten Dreborg has no conflict of interest.
None.