Anisakis simplex is a helminth parasite belonging to the Nematode class. In 1876, Leucckart described the first case of human parasitic disease in a Greenlander child, although anisakiasis started to be known in 19601. In 1990, Kasuya et al. suggested that this parasite should be considered as an etiological factor to be ruled out in the allergic reactions induced by fish2. In 1995, Audicana et al. described the first case of Anisakis-induced anaphylaxis3.
When parasitic disease by Anisakis4 occurs, humans are occasional hosts who acquire the parasite through the ingestion of contaminated fish, and larvae in phase L3 cannot complete its vital cycle. A. Simplex larvae in phase L3 and L4 include antigenic components able to induce an immune response from the infested subject. There are three kinds of antigens: somatic, ES (excretion-secretion) and surface antigens. At least four antigens with allergenic power (major allergens) have been identified with very variable molecular weights Ani s1; Ani s2 (paramyosin); Ani s3 (tropomyosin), responsible for cross-reactions; and Ani s4, 5, 6 and 75.
Infestation and transmission of A. Simplex are associated to the ingestion of raw fish, and relates to the eating habits. It is particularly frequent among the Japanese population, although in recent years this disease is increasing its frequency in Europe, particularly in Holland, France, Germany and Spain.
We present a case of a sixty-nine year-old male who presents generalised itchy, erythematous hives, mainly in trunk, lower and upper limbs, as well as angioedema in ears, general malaise, dyspnoea, chest tightening, and finally lost of consciousness. The patient was assisted at home and during his transfer to the Emergency Department he had a cardiac arrest requiring resuscitation. The patient was admitted in hospital for 72 hours with good response to treatment corticosteroids and antihistamines. Three days after being discharged from hospital, the patient went back to the Emergency Department due to another episode.
When the patient came to our clinic, he was asymptomatic on treatment with hydroxizine and ceterizine. During the physical exam, no skin lesions were observed. Personal background: iron-deficiency anaemia and type 2 diabetes mellitus, reason why the patient used to eat fresh fish frequently as dietetic measure.
Skin tests resulted negative (the patient was on treatment with antihistamines). In the blood test, 5% eosinophil count was detected. The specific IgE to Anisakis was 1.08 kU/l. Stool examinations for pinworm and Visceral larva migrans were negative. Serology test for the latter worm was negative.
Levocetirizine 5mg every 24 hours and fish-free diet was advised until the study was finished. In spite of the diet, the patient reported persistence of daily, very itchy macular rash, with no time pattern. Skin tests were performed again (after stopping the antihistamine treatment) resulted positive to Anisakis.
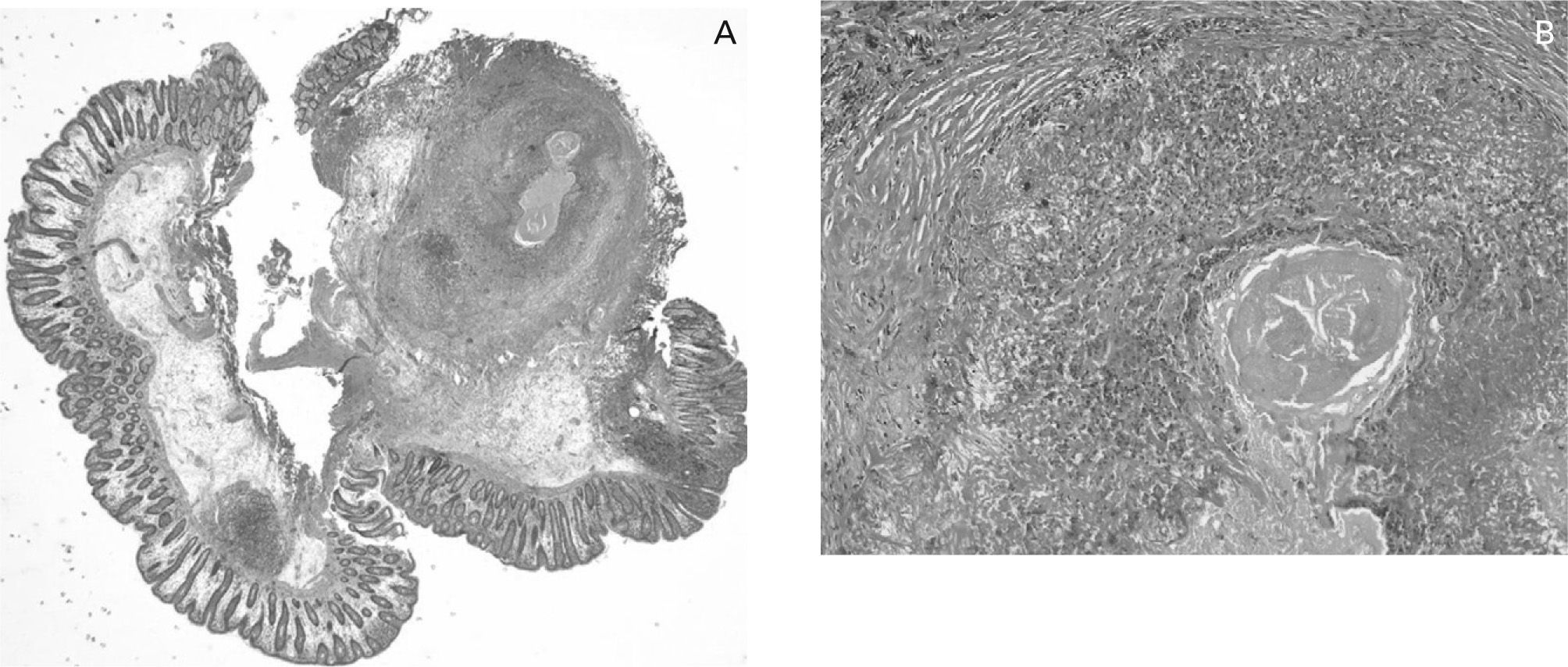
Due to his anaemia, the Department of Internal Medicine performed a gastroscopy and colonoscopy in order to find out its cause, and a 5mm of diameter submucosal lesion was observed at the hepatic angle of the colon, surrounded by normal mucosa. A biopsy of the area was performed and the pathological diagnosis was “granulomatous chronic inflammation related to the presence of a helminthtype parasite, probably Anisakis” (fig. 1–2). The serology of Visceral larva migrans was repeated being positive on this occasion.
Considering the medical profile of the patient, the results of skin tests, the eosinophil count, specific IgE and serology, the diagnosis was anaphylaxis induced by sensitisation to the fish parasite Anisakis simplex. After five months, the patient came back to consultation. He reported being asymptomatic with the fish-free diet and treatment with mebendazole and dexchlorpheniramine. Colonoscopy and biopsy of the area were performed again, with negative results.
Anaphylaxis is an immediate hypersensitivity reaction which entails vital risk. Although drugs are the main allergens involved in anaphylaxis, followed by hymenoptera and some foods, parasites are increasingly responsible for anaphylactic reactions, being Anisakis simplex the most frequent6.
Induction of a Th2 response, involving the action of cytokines IL3, IL4, IL5 that control the mast cell activation, IgE response and high eosinophil count are typical of infestation by nematodes7,8. Specific IgE to some Anisakis simplex antigens is detected in the sera of patients with anisakiasis, reason why reactions are considered to be of hypersensitivity to the parasite. For this kind of IgE-mediated reactions to take place the active infestation is necessary, like in the case we report. For this, the allergens of A. simplex must interact with the immune system of the host and this only happens when the parasite inoculates them in the tissues.
According to the present report and in agreement with other authors9, it is important to highlight the importance of the allergy study (skin tests and specific IgE quantification) to show the existence of a sensitisation to Anisakis and to recommend the preventive measures, as well as to reach a diagnosis, particularly in the case of anaphylaxis.
Furthermore, the importance of a positive serology to Viscera larva migrans (Ascaris lumbricoides)8 must be considered because it can help to reach the diagnosis due to its cross-reactivity with Anisakis simplex, via a common protein (ABA-1)7.
Because of the increasing knowledge of the sensitisation to Anisakis simplex, and the clinical importance of those severe situations such as anaphylaxis, the competent Food Safety Authorities advised by the experts are introducing some measures to decrease the infestation. It is important for them to consider all links in the production-consumption chain10. In this sense, and according to the current regulations, we advise the sensitised patients to avoid the ingestion of raw or rare or scarcely processed fish, (salted, smoked, in vinegar, etc); to eat fish previously frozen at −20°C or even better frozen while on the seas, because the guts are removed immediately after the capture; to avoid the hipoaxial region, eating preferably the tail of big fish; and to advise about the sensitisation to Anisakis when eating in restaurants.
Taking into account that our patient suffers from diabetes and therefore fish is necessary in his diet, once the sensitisation was treated and under control, we allowed eating fish following the recommendations mentioned before.
In any anaphylaxis case, one must try to reach its aetiology and Anisakis is an important allergen to be borne in mind. In the search for Anisakis sensitisation, to take a good clinical history, to perform skin tests and to measure specific IgE are essential.
For recurrent episodes of urticaria and/or anaphylaxis with sensitisation to Anisakis, apart from the fish-free diet and depending on the patient's clinical course, to perform an endoscopic study should be considered.