Total laryngectomy (TL), with eventual postoperative radiotherapy, has proven to be effective in treating cases of locally advanced hypopharyngeal cancer. The aim of this study was to analyse the oncological outcomes of this procedure in patients with hypopharyngeal cancer classified T3 and T4.
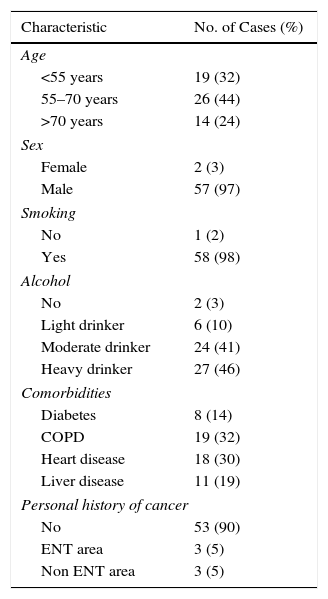
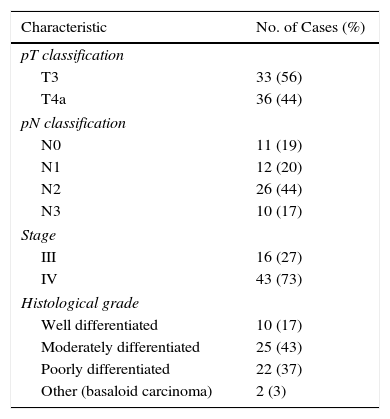
MethodsWe studied 59 patients (33 T3 and 26 T4a) with primary squamous cell carcinoma of the hypopharynx treated with TL from 1998 to 2012.
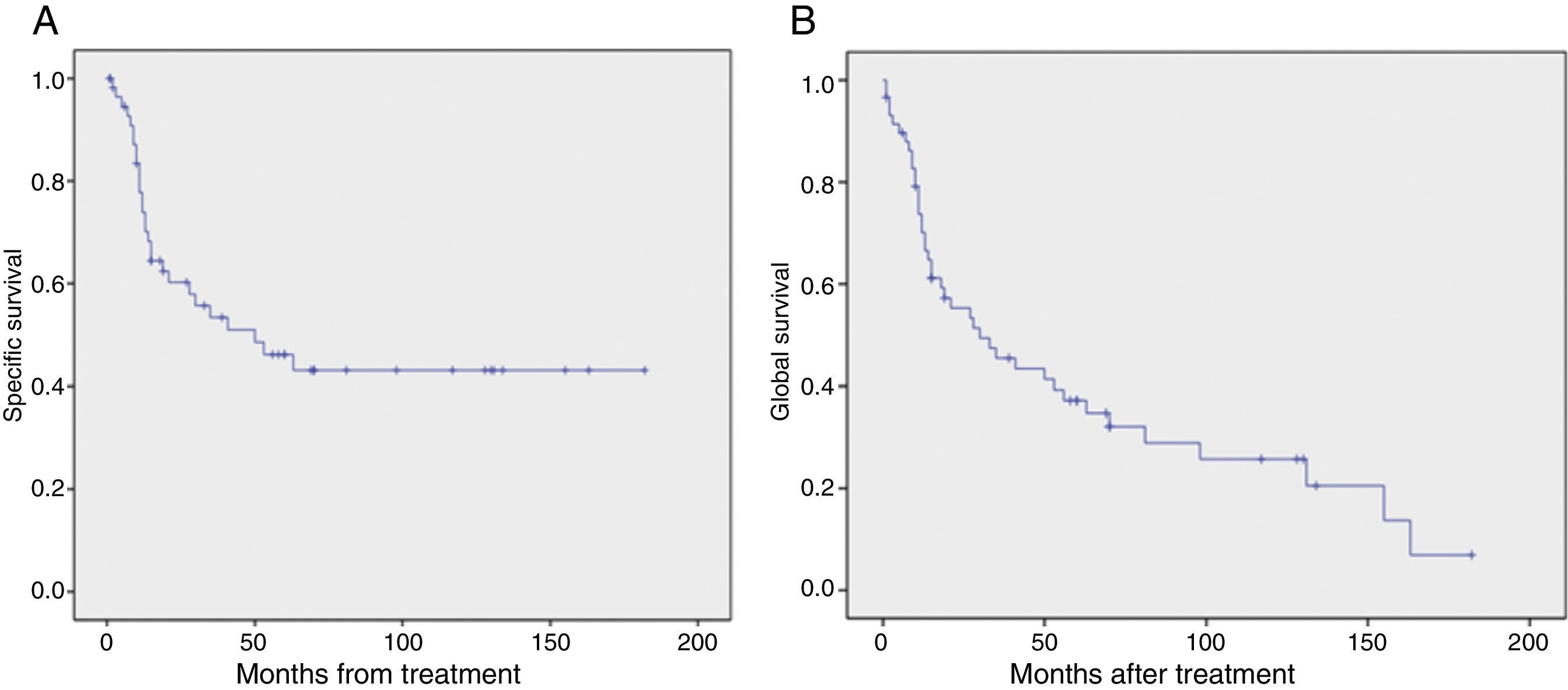
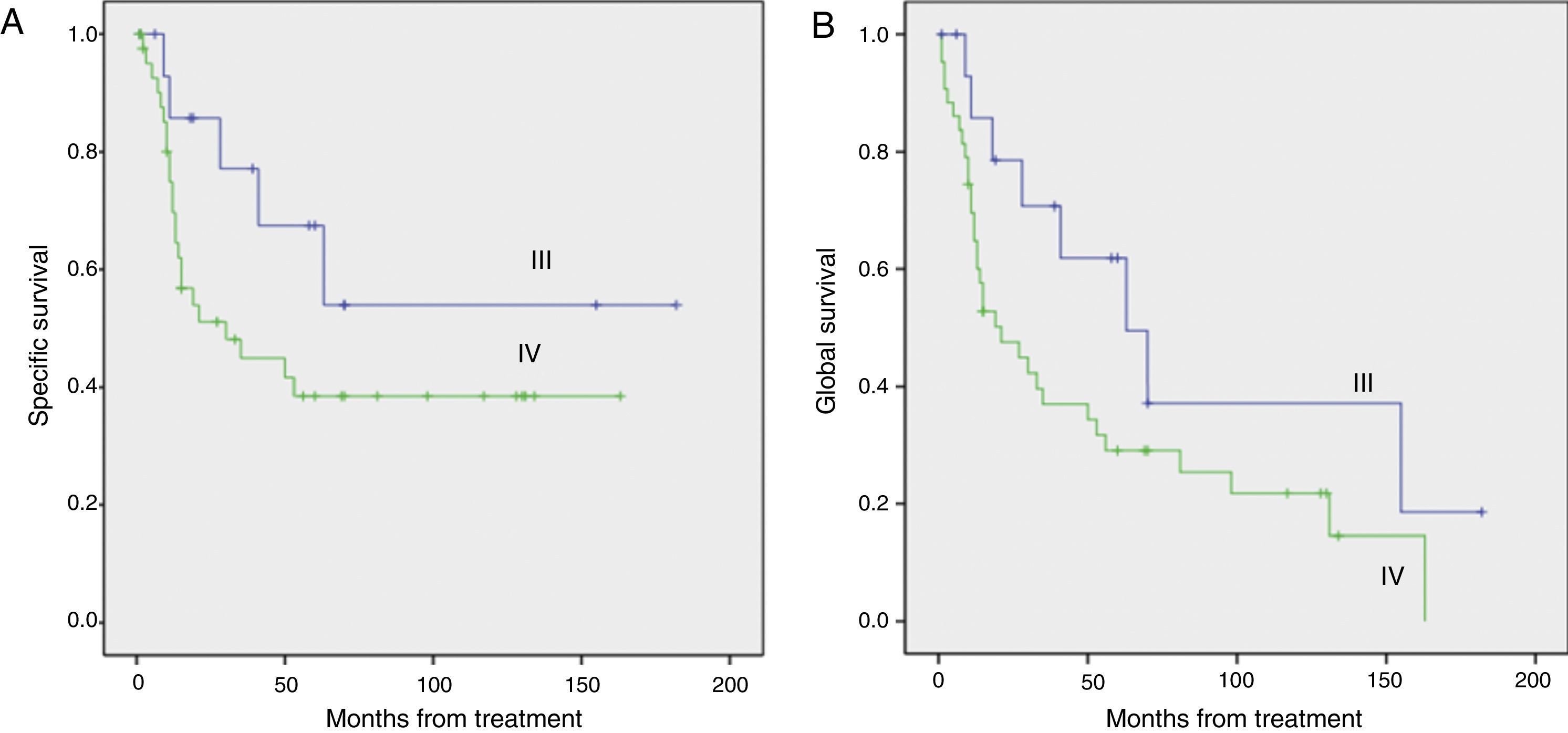
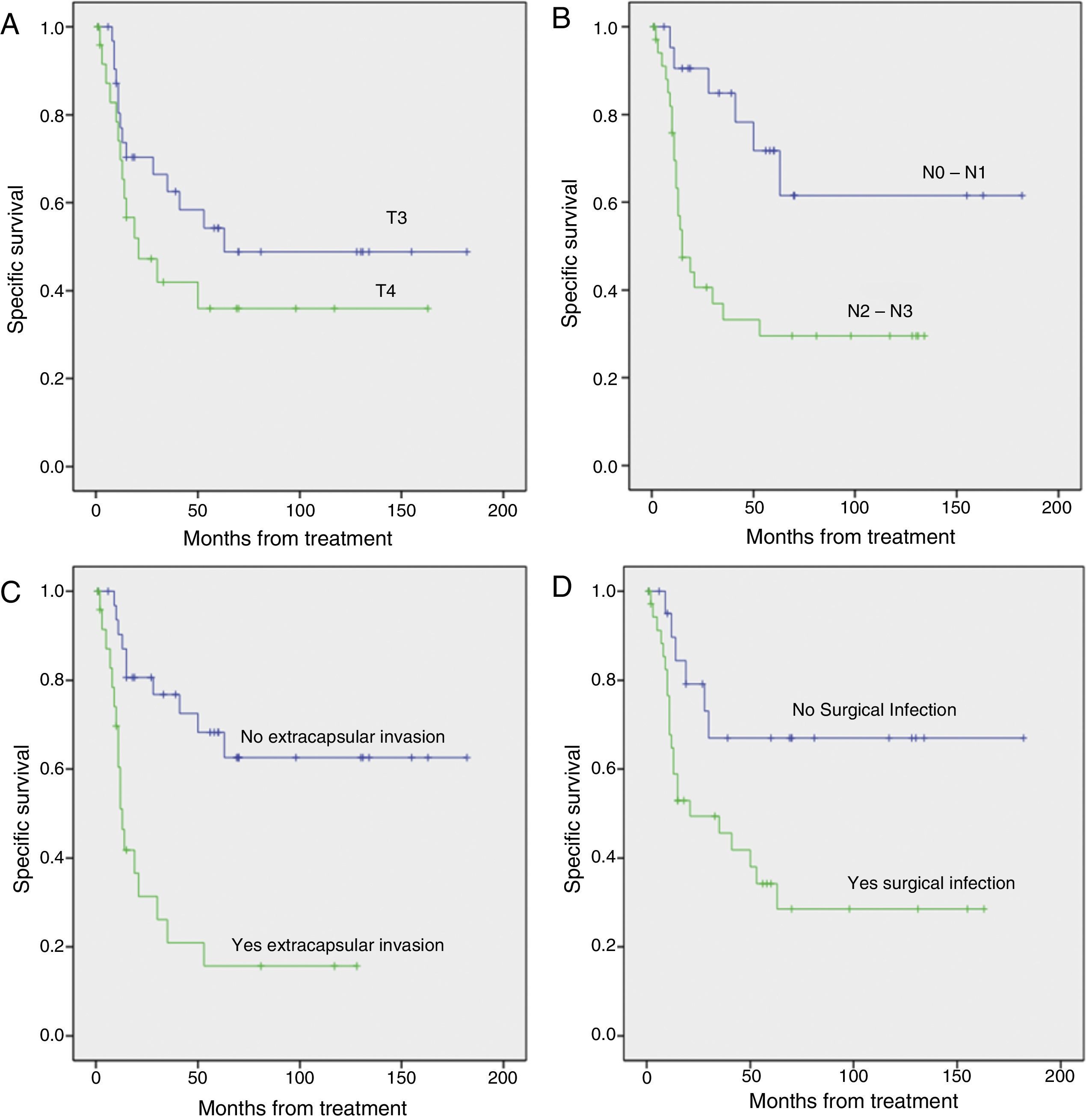
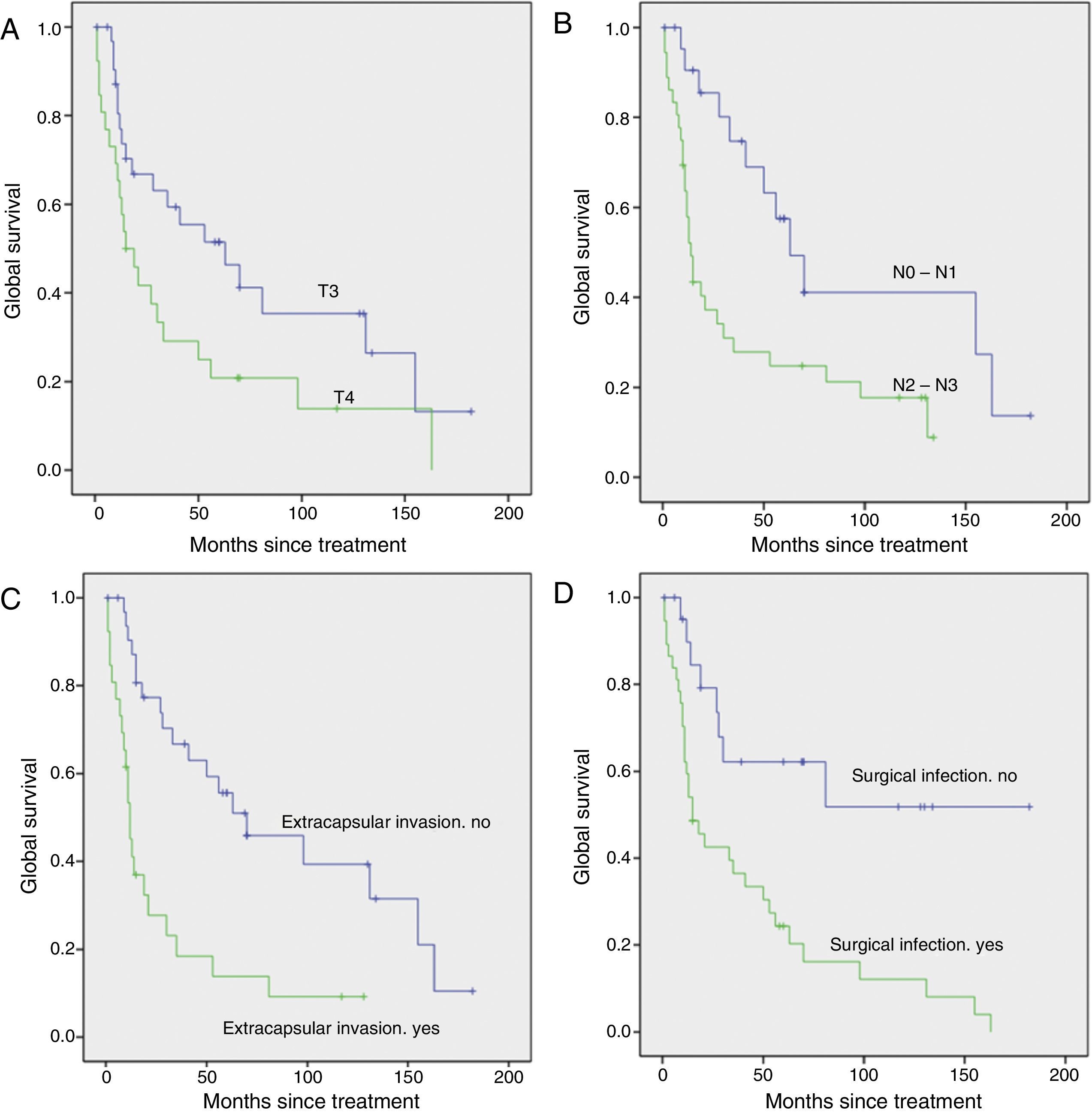
ResultsMean age was 61 years with a male predominance (96.6%). All the patients were smokers and 96% consumed alcohol. Unilateral selective neck dissection (ND) was performed in 12 patients, unilateral radical ND in 11 patients, bilateral selective ND in 20 patients and radical ND plus selective ND in 14 patients. Sixty-six percentage of the patients received postoperative radiotherapy. Lymph node metastases occurred in 81% of the patients and extranodal invasion in 56% of them. Twenty-nine percentage of the patients had loco-regional recurrence, 17% developed distant metastases, and 25% a second primary tumour. The 5-year disease-specific survival was 46%.
ConclusionsTL extended to pharynx (with eventual postoperative radiotherapy) offers good oncological results in terms of loco-regional control and survival in locally advanced hypopharyngeal cancer, so organ preservation protocols should achieve similar oncological results to those shown by TL.
La laringectomía total (LT), más eventual radioterapia, ha demostrado ser un tratamiento eficaz en los casos de cáncer de hipofaringe localmente avanzado. El objetivo de este trabajo es analizar los resultados oncológicos de este procedimiento en pacientes con cáncer de hipofaringe T3 y T4.
MétodosSe incluyeron 59 pacientes (33 pacientes con estadio T3 y 26 con estadio T4a) con carcinoma epidermoide primario de hipofaringe tratados mediante LT entre los años 1998 y 2012.
ResultadosLa edad media fue de 61 años, con predominio de varones (96,6%). Todos los pacientes excepto uno eran fumadores y el 96% consumía alcohol. Se realizó vaciamiento cervical funcional unilateral en 12 pacientes, radical unilateral en 11 pacientes, funcional bilateral en 20 pacientes y funcional más radical en 14. El 66% de los pacientes recibieron radioterapia postoperatoria. Un 81% de los pacientes presentaba metástasis ganglionares y de estos un 56% presentaba invasión extracapsular. Un 29% de los pacientes presentaron recidiva locorregional, un 17% desarrollaron metástasis a distancia y un 25% un segundo tumour primario. La supervivencia específica fue del 46% a los 5 años.
ConclusionesLa LT ampliada a faringe (con eventual radioterapia complementaria) ofrece buenos resultados oncológicos en términos de control locorregional de la enfermedad y supervivencia en el cáncer de hipofaringe localmente avanzado, de modo que los protocolos de preservación de órgano deben alcanzar resultados oncológicos similares a los demostrados por la LT.