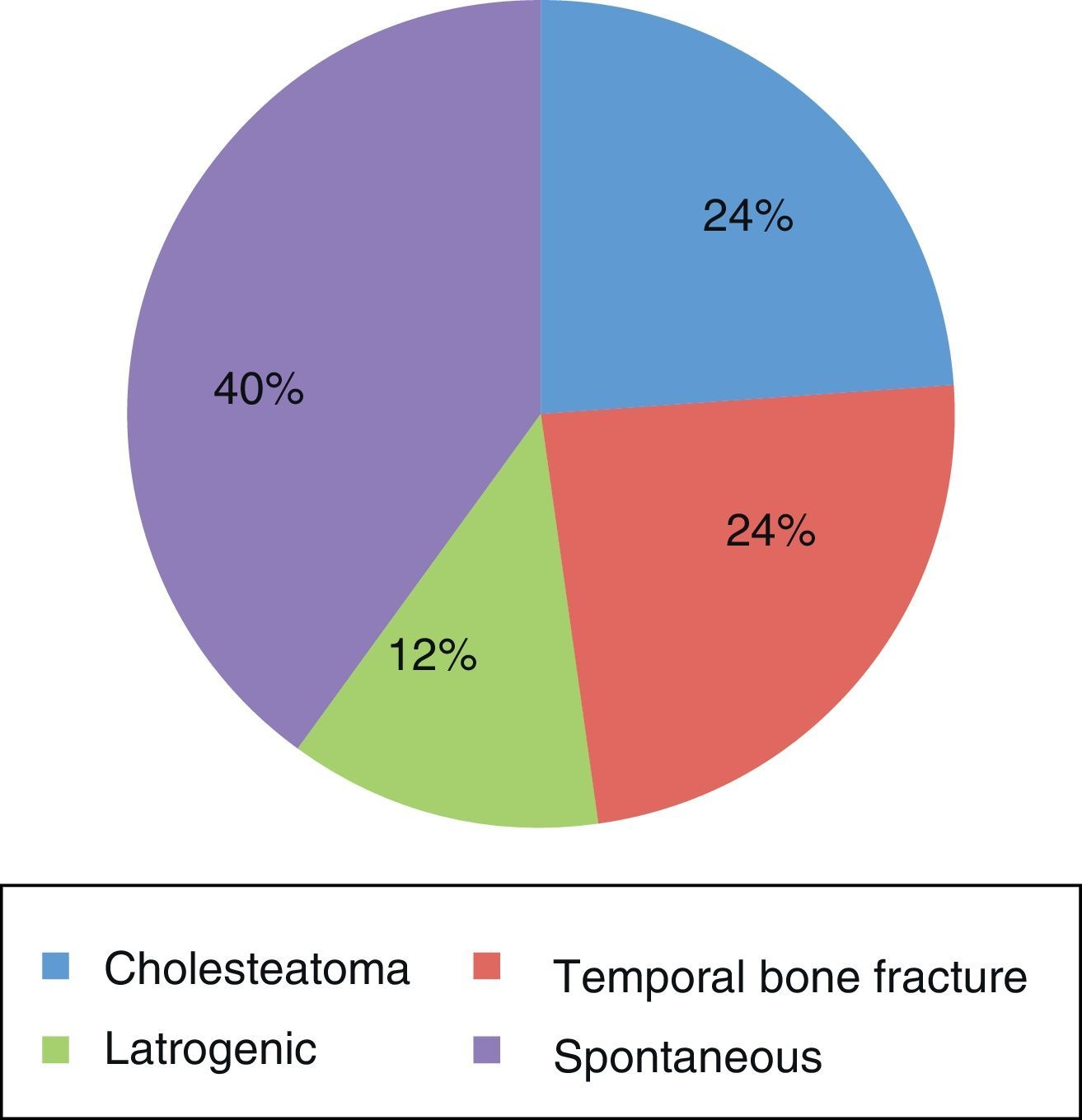
Cerebrospinal fluid otorrhea results from an abnormal communication between the subarachnoid space and tympanomastoid compartment; most of them are of traumatic aetiology. They have clinical interest due to the potential risk of meningitis, directly related to the aetiology. Our aim was to show our experience in the management of this process.
MethodsA total of 17 patients were diagnosed and treated for cerebrospinal fluid otorrhea from 2003 to 2011.
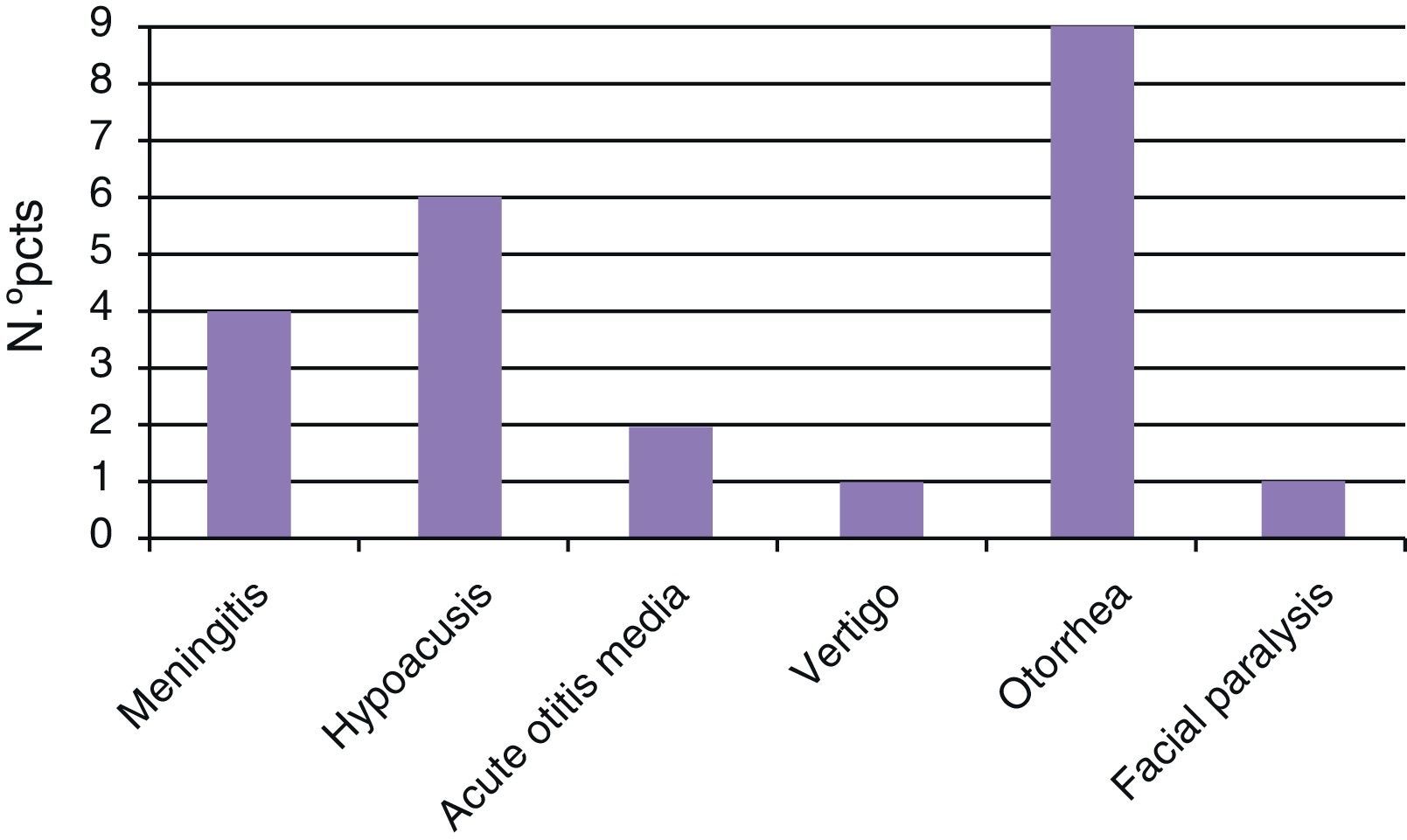
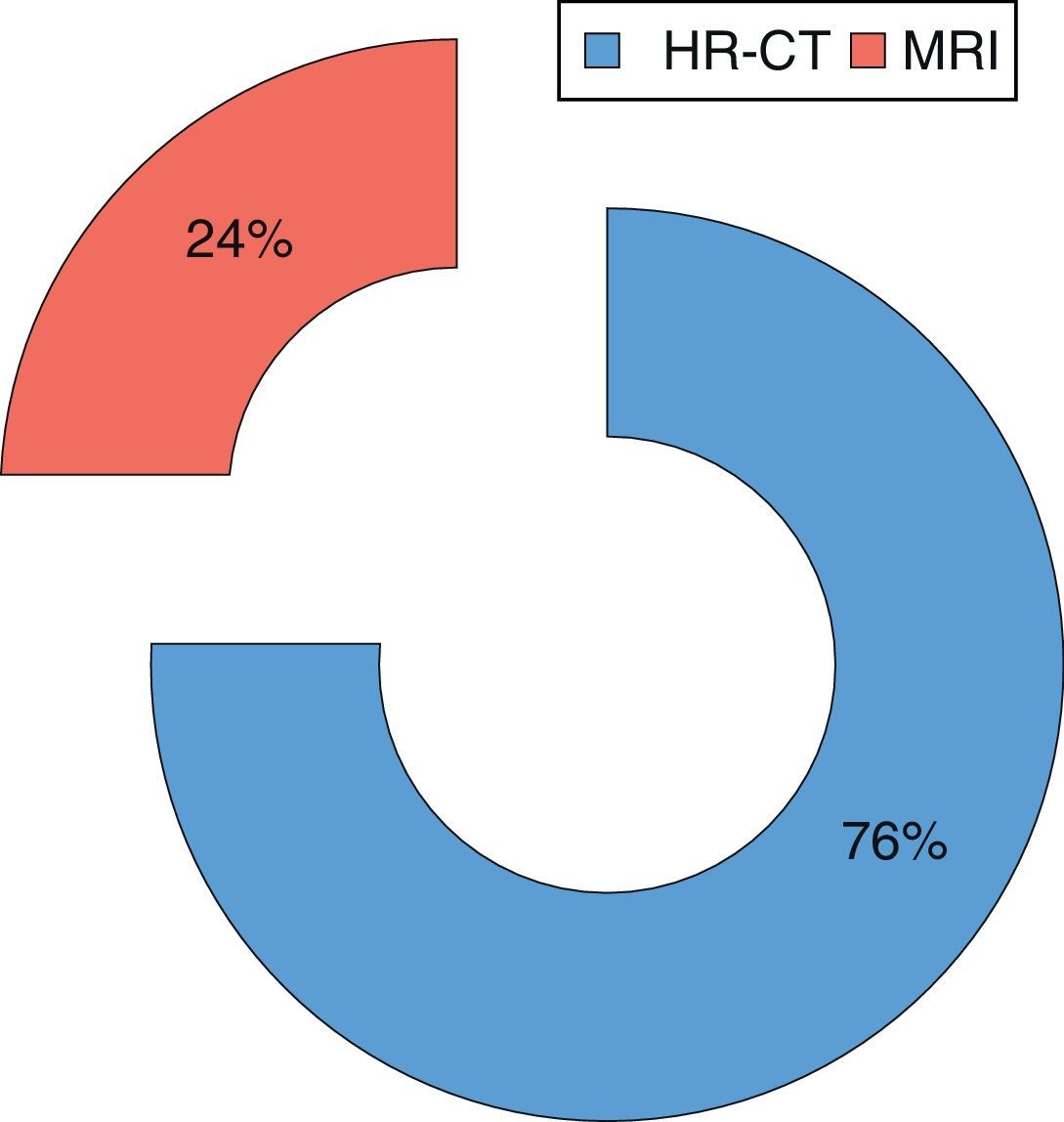
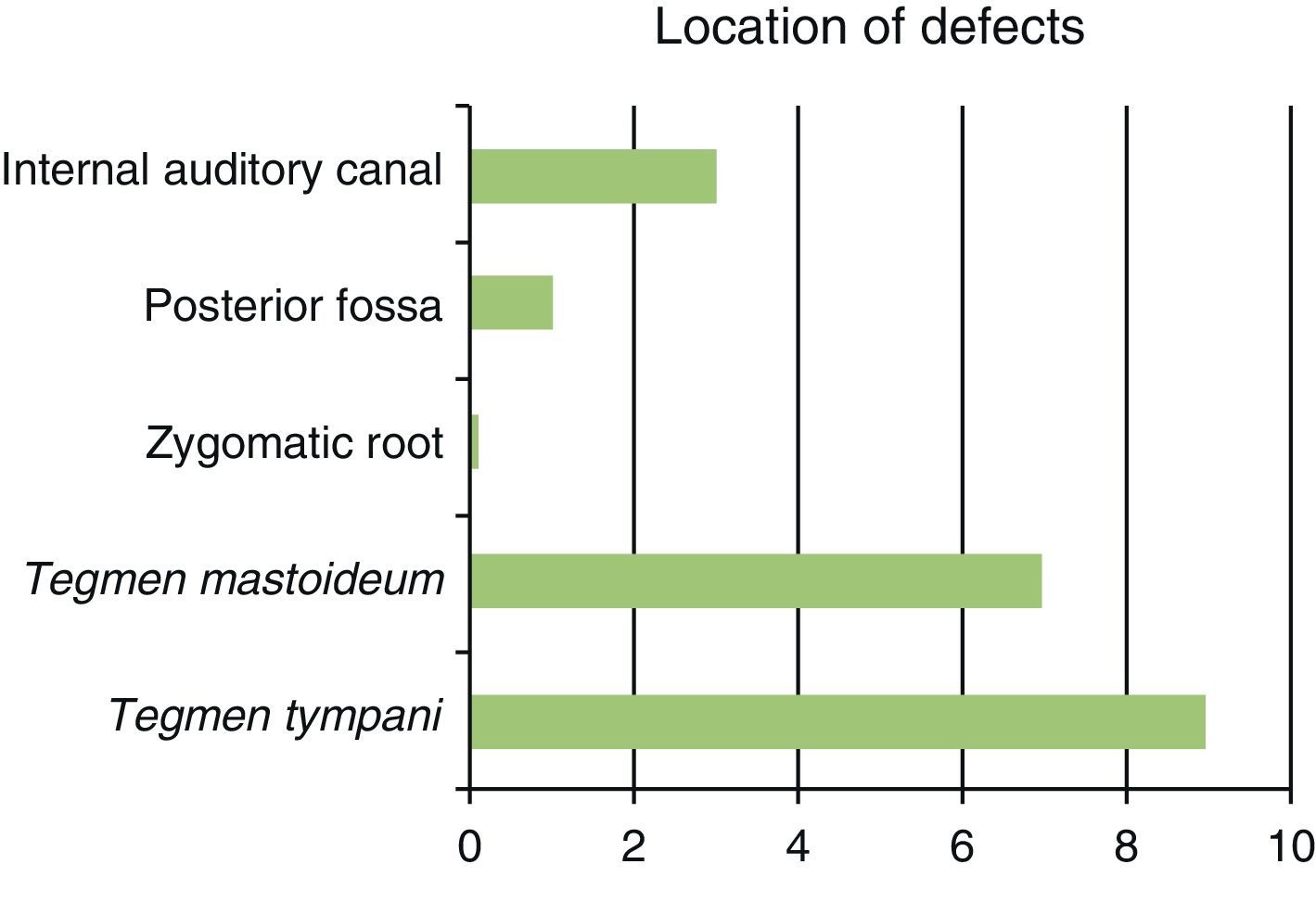
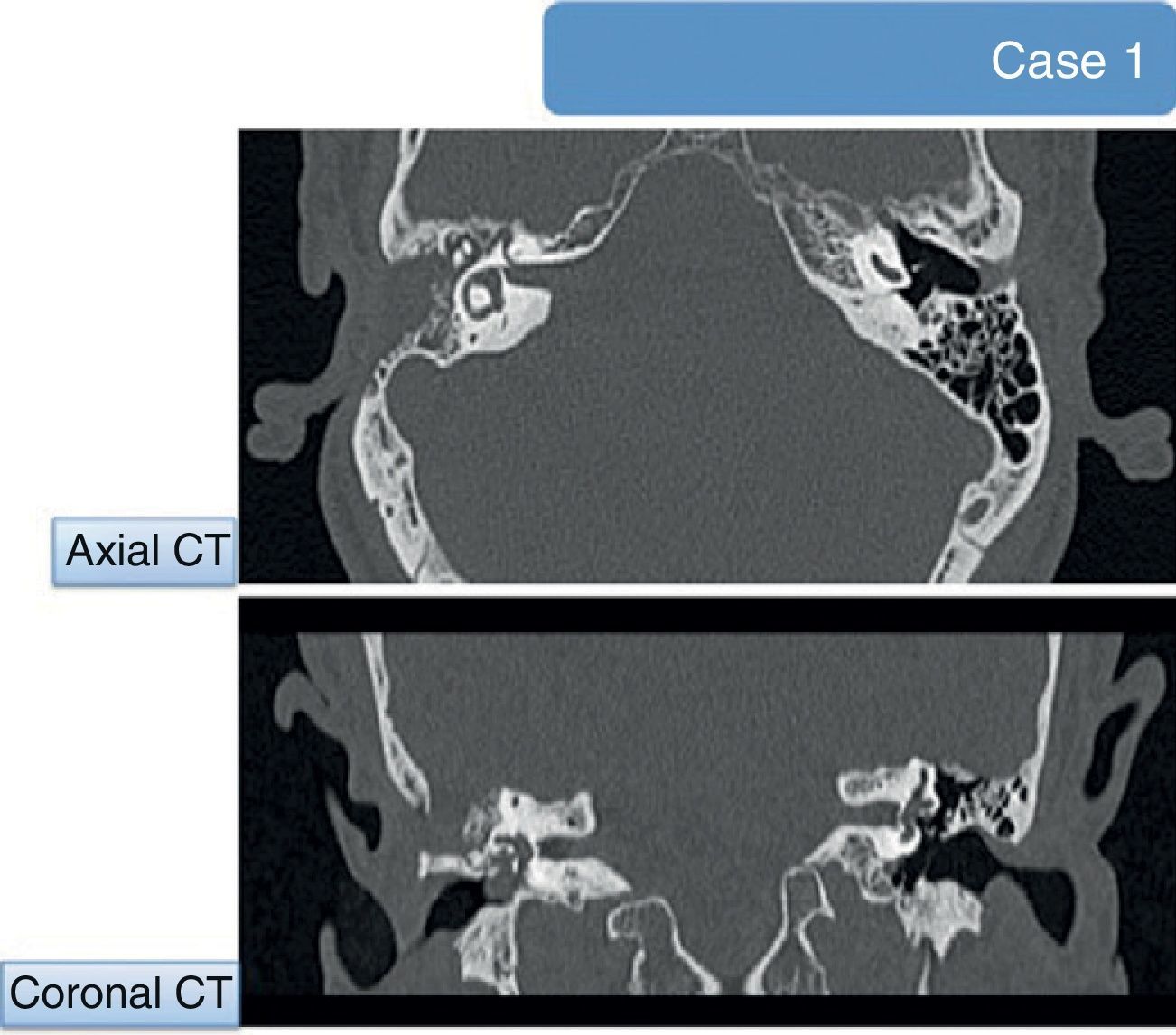
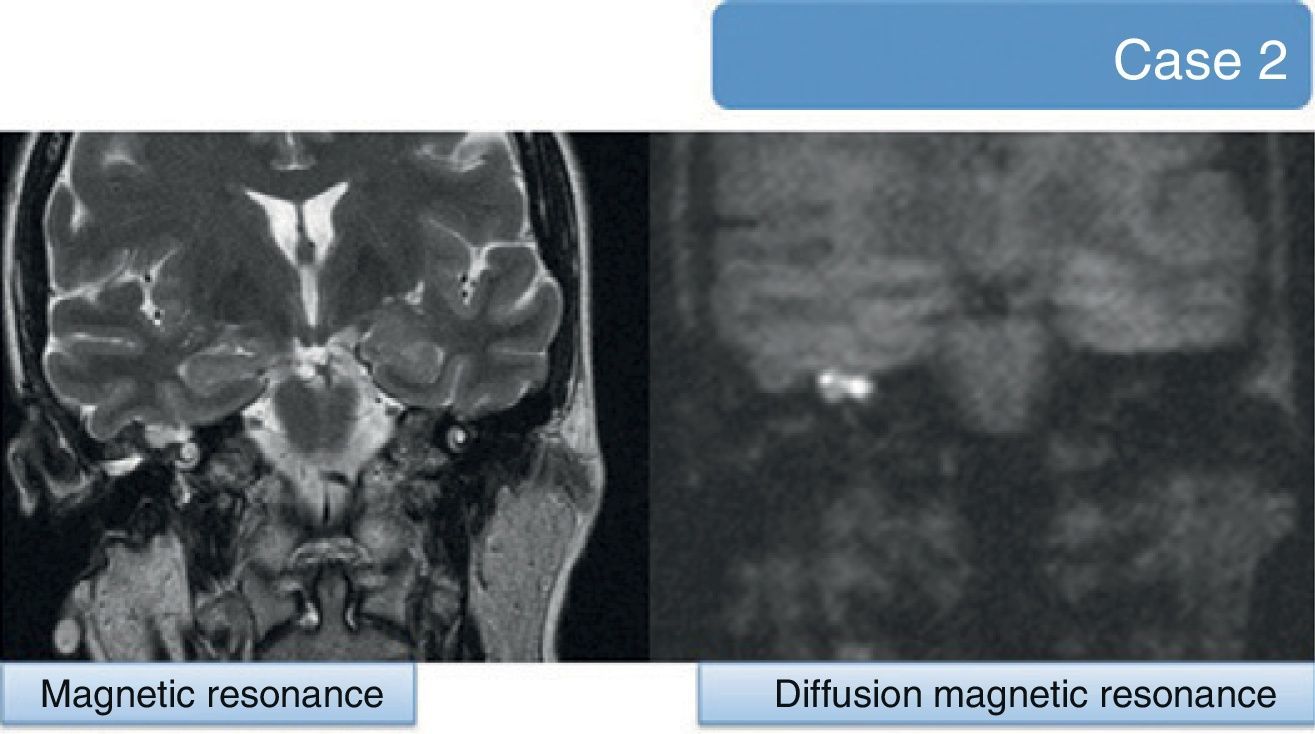
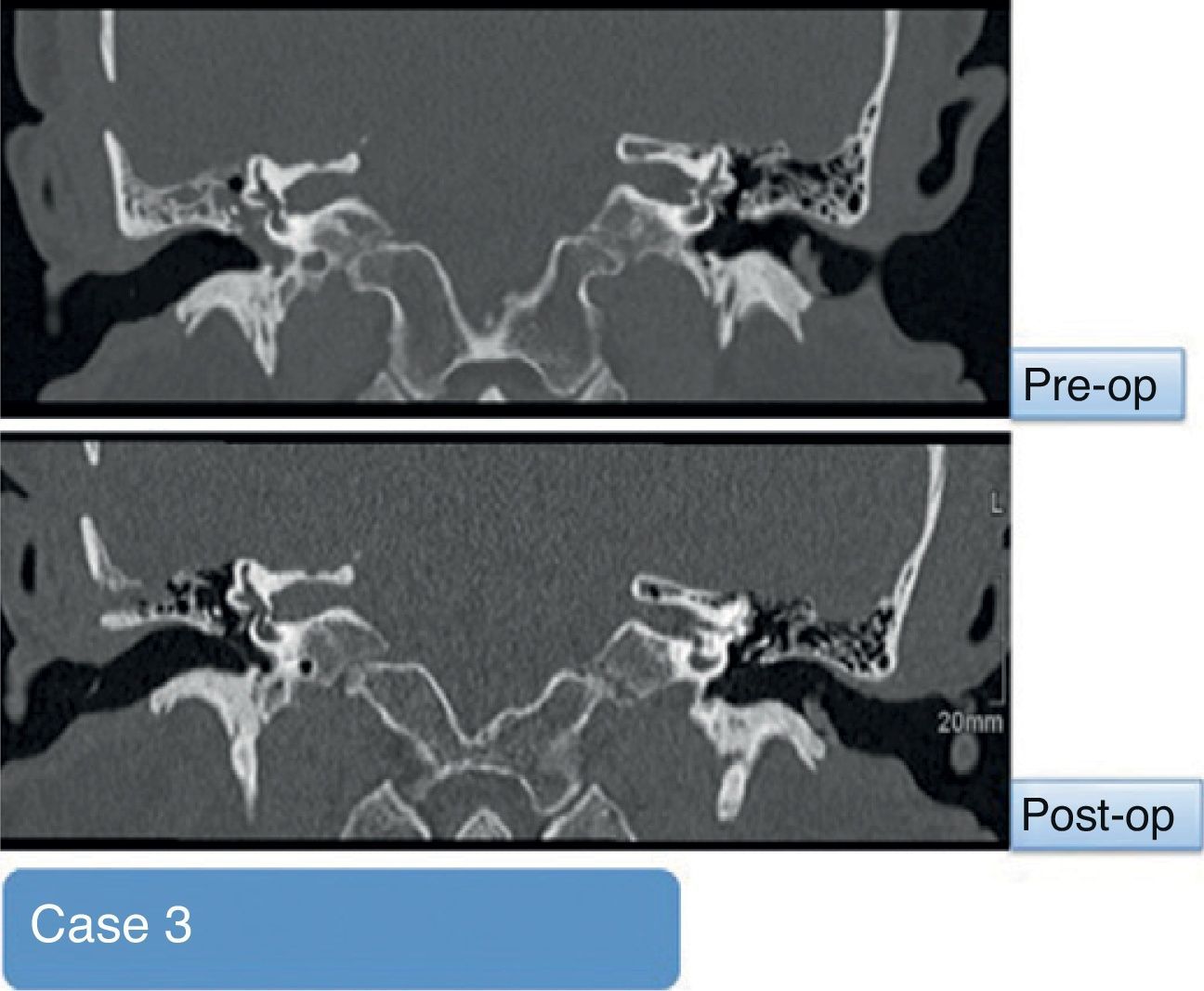
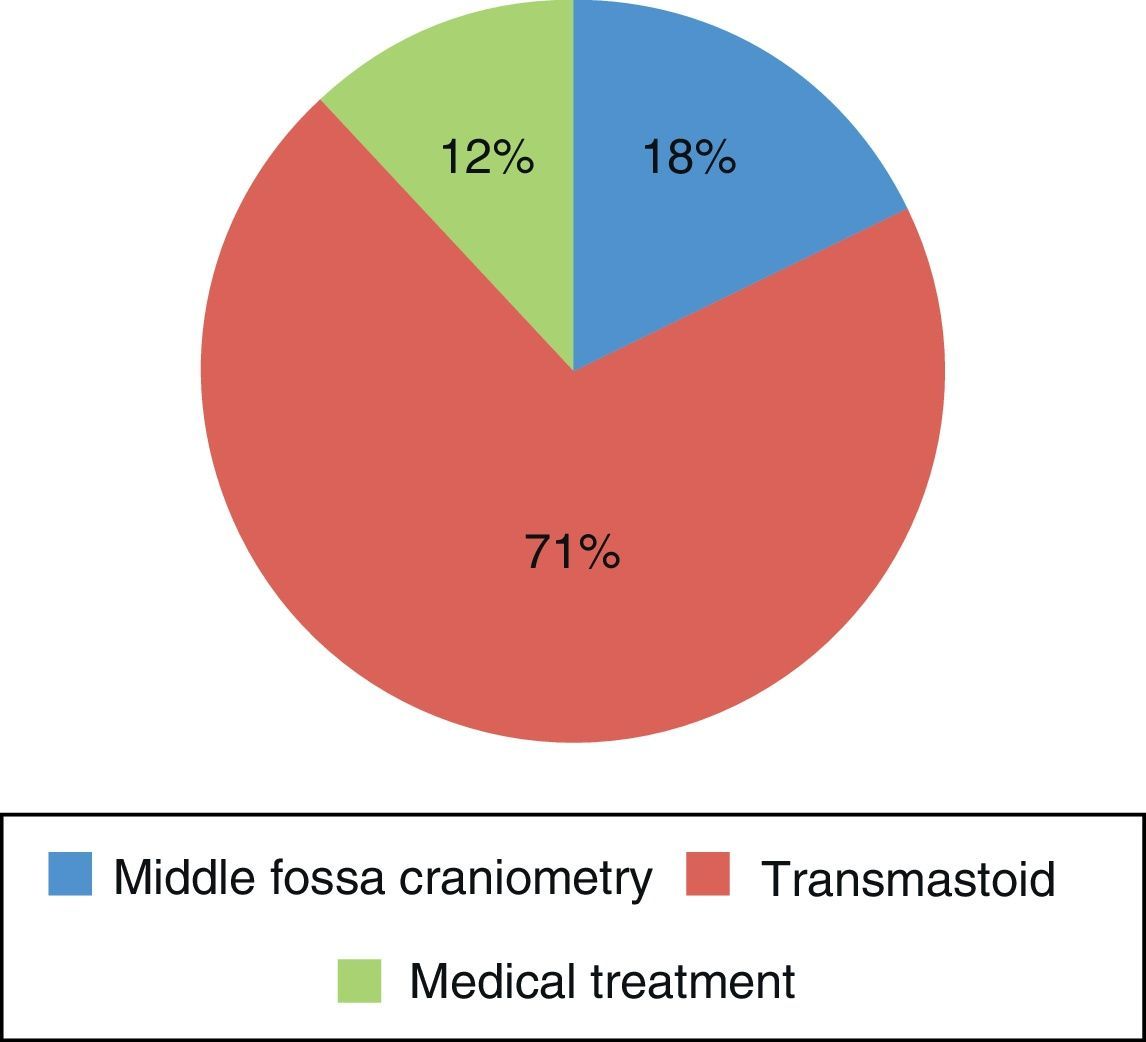
ResultsIn our study, the highest percentage of cases was spontaneous cerebrospinal fluid otorrhea, with a wide clinical presentation. The diagnosis was based on the determination of beta-2-transferrin and radiological studies, especially important for its locator value. The treatment of choice was surgery.
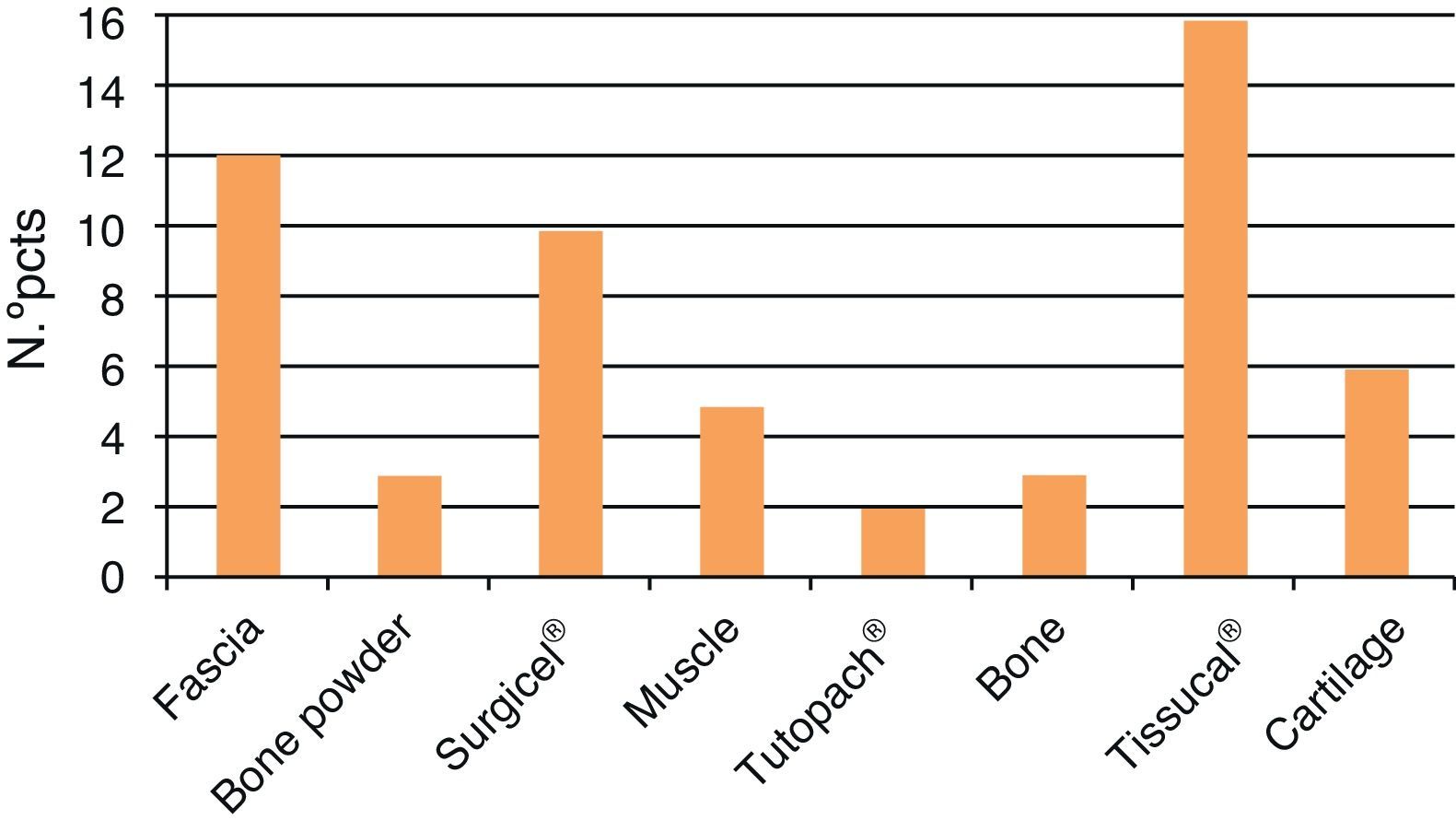
ConclusionsCerebrospinal fluid otorrhea is a rare entity in otorhinolaryngological pathology. Its diagnosis is suspected through otorrhea, hearing loss and aural fullness, while computed tomography and magnetic resonance help us to locate the defect. Surgery is the preferred technique, and its success is based on multilayer technology with 2 or more support materials.
Las fístulas de líquido cefalorraquídeo en el oído derivan de una comunicación anormal entre el espacio subaracnoideo y el timpanomastoideo, la mayoría de etiología traumática. Tienen gran interés desde el punto de vista clínico por el potencial riesgo de meningitis, directamente relacionado con la etiología. Nuestro objetivo es mostrar nuestra experiencia en el manejo de dicho proceso.
MétodosPresentamos un total de 17 pacientes diagnosticados y tratados de fístulas de líquido cefalorraquídeo en el oído desde el año 2003 hasta el 2011.
ResultadosEn nuestro estudio el mayor porcentaje de casos correspondían a otolicuorreas de tipo espontáneo, con una presentación clínica variada. El diagnóstico se basó en la determinación de la beta-2-transferrina y en estudios de imagen, especialmente importantes por su valour localizador del defecto. El tratamiento quirúrgico fue el de elección.
ConclusionesLas fístulas de líquido cefalorraquídeo en el oído constituyen una entidad rara en la patología otorrinolaringológica. Su diagnóstico se sospecha por signos característicos como la otolicuorrea, pérdida auditiva y sensación de plenitud ótica, mientras que la tomografía computarizada y la resonancia magnética nos ayudan a su localización. La cirugía es la técnica de elección, y su éxito se basa en la técnica multicapas con 2 o más materiales de soporte.