To analyze the impact of infectious complications and microbiology in the postoperative period after major oncologic neck surgeries.
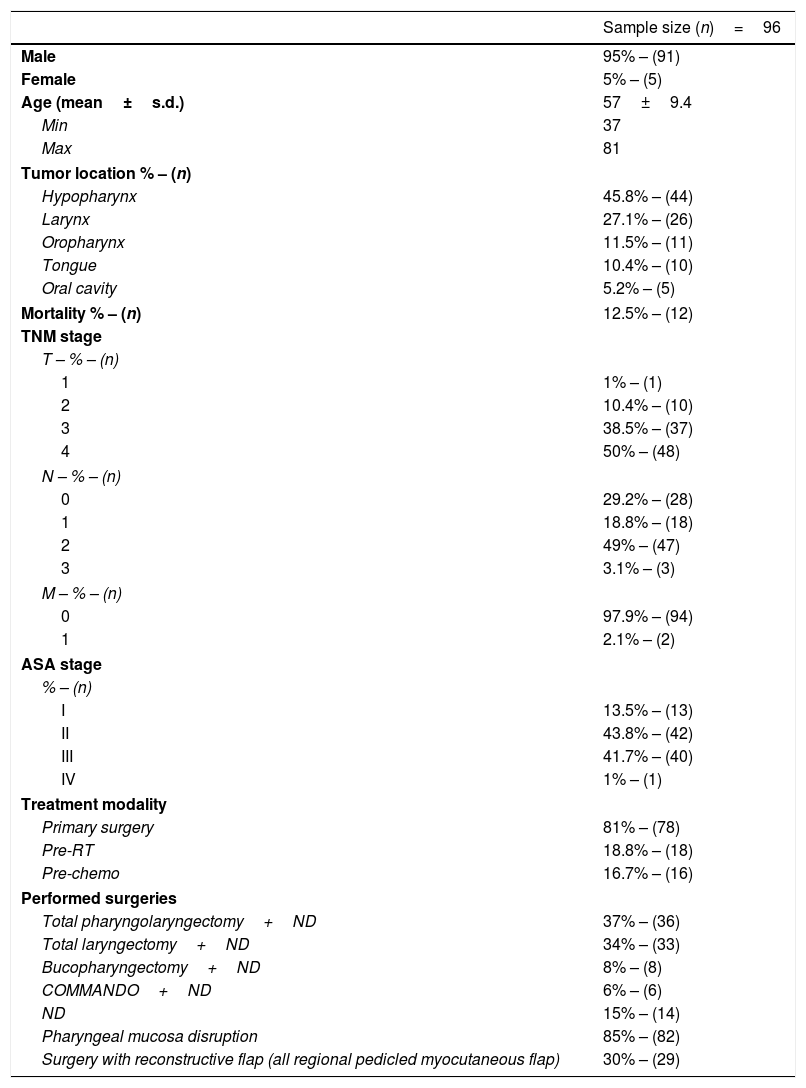
MethodsA retrospective study conducted in an oncology center, including all the consecutive patients who developed infectious complications after major neck cancer surgery, from October 2012 to May 2016 (44 months). Among other data, we collected TNM stage, ASA score, body mass index, comorbidities and habits, pre and postoperative hemoglobin levels, albumin serum levels, pre-surgical treatments, length of inpatient stay, isolated microbiological agents and the recorded complications and mortality rate.
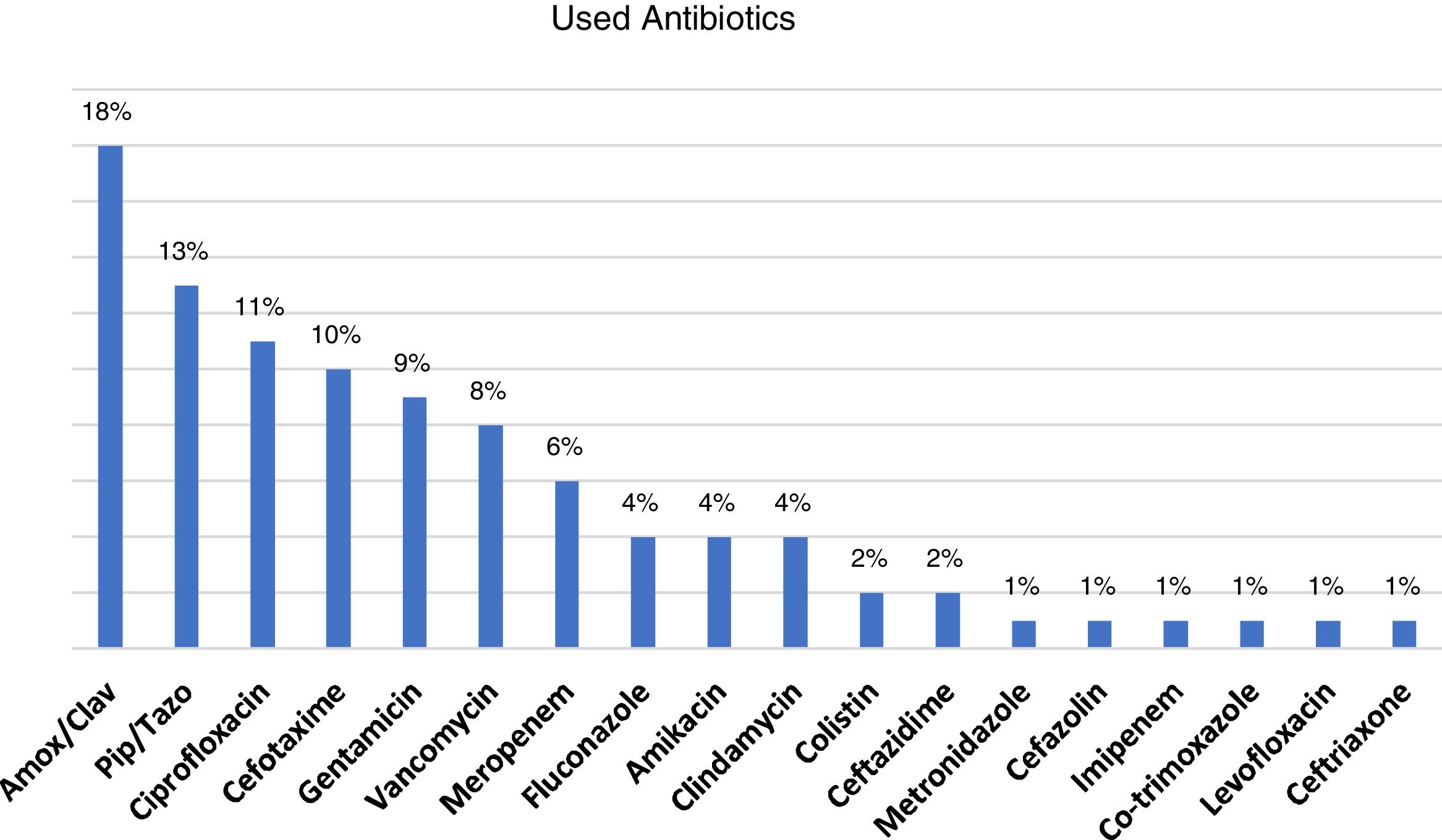
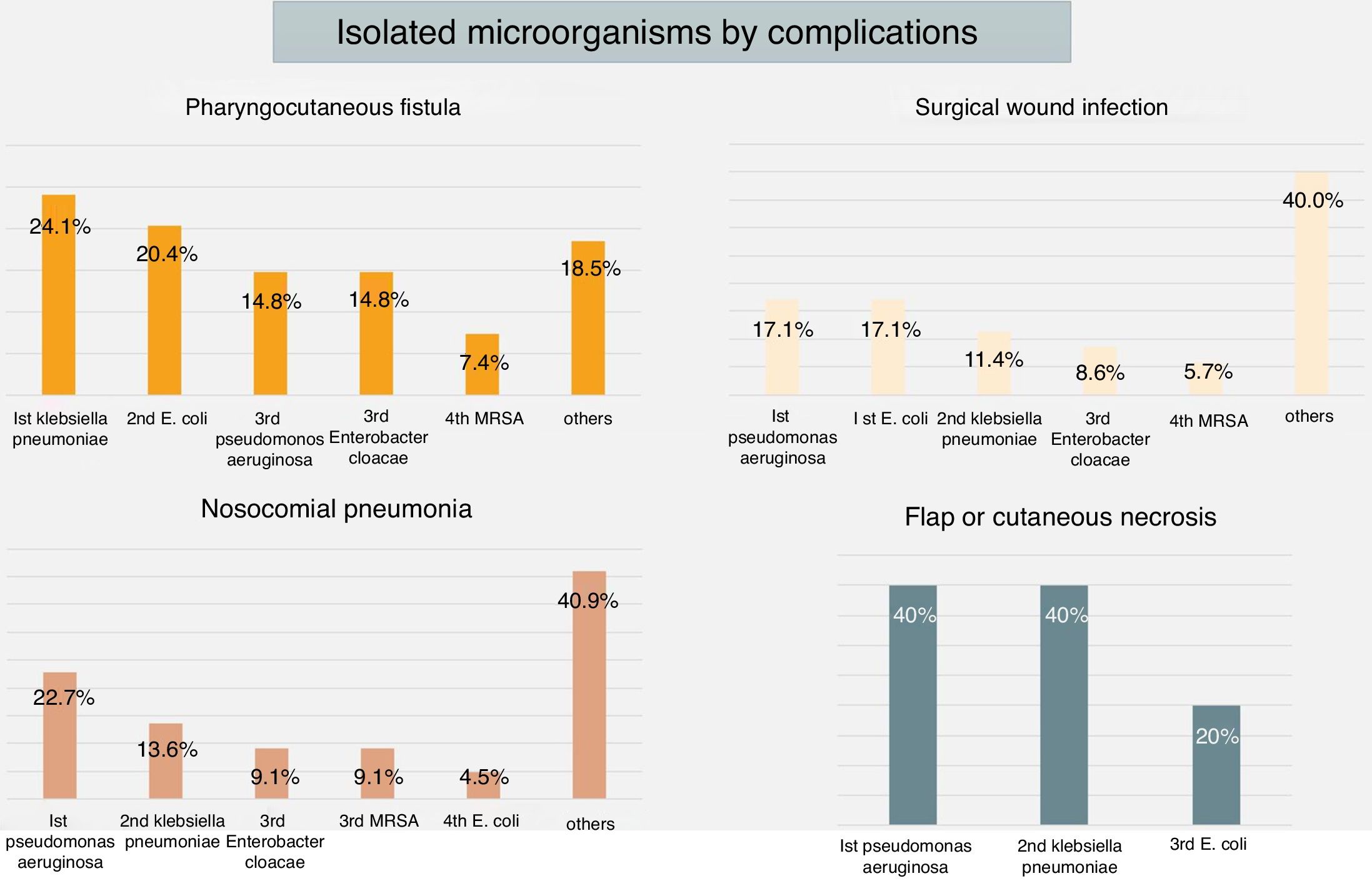
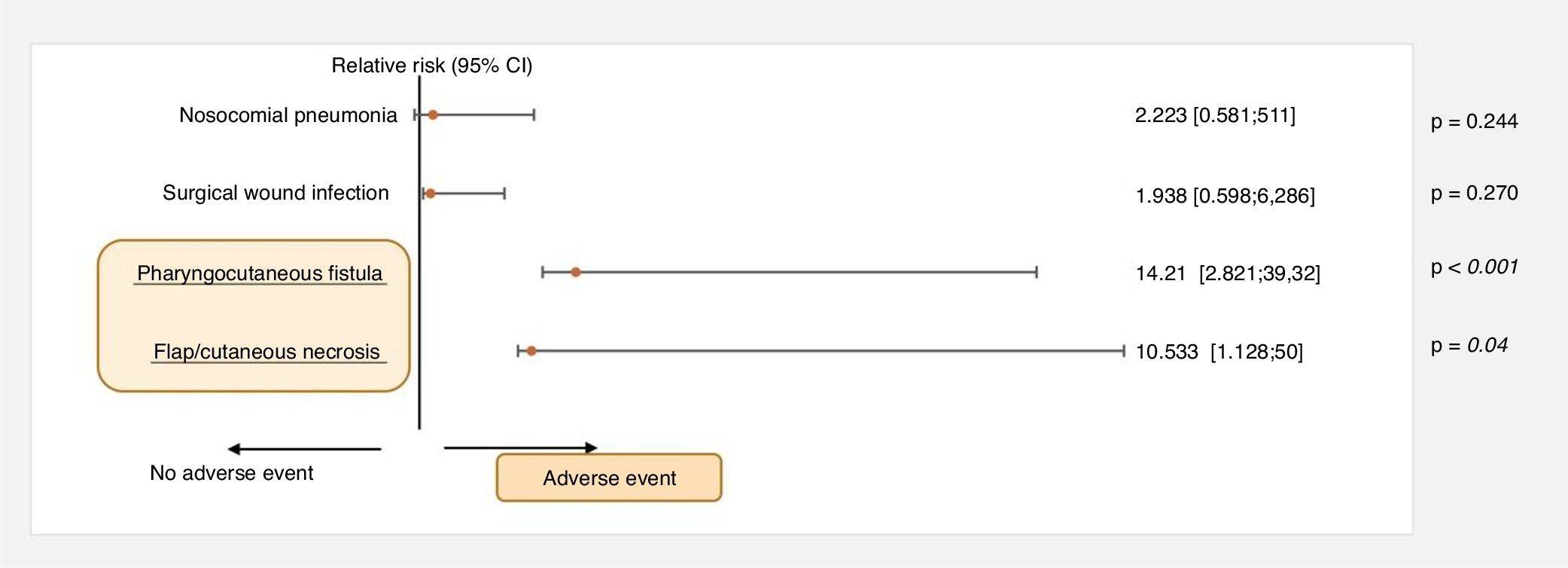
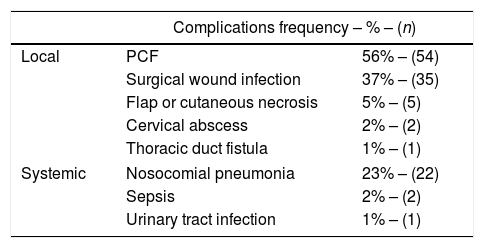
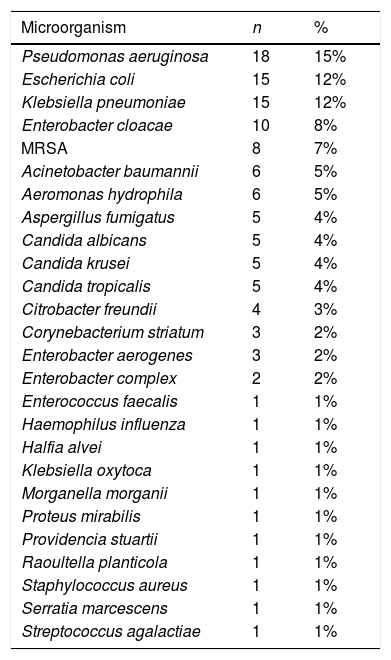
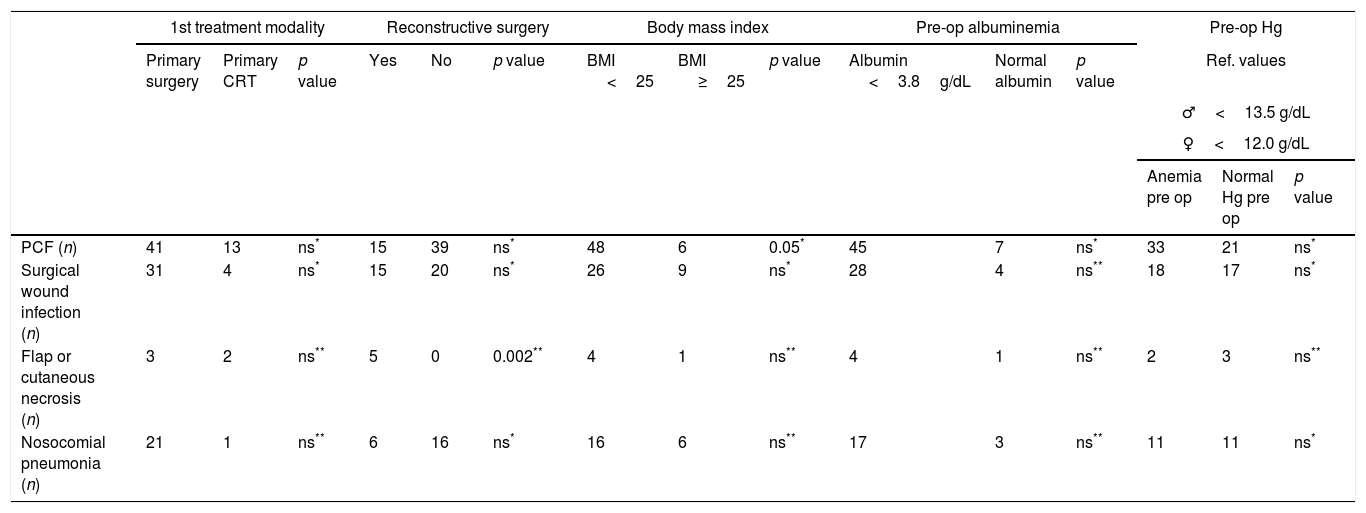
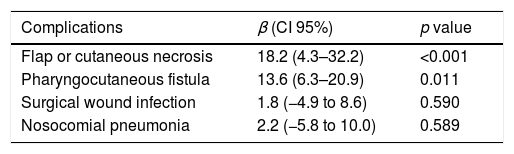
ResultsIn the studied period, 761 major neck surgeries were performed. Of these, 96 patients had complications (12.6%). Pharyngocutaneous fistula (PCF) was the most frequent complication (56%) and nosocomial pneumonia was the most common systemic complication (23%). Pseudomonas aeruginosa was the principal microorganism of the 26 species isolated (15%). 12 deaths were registered. Using multiple linear regression we concluded that flap/cutaneous necrosis and PCF were complications with statistical significance that prolonged inpatient stay. The same complications had significant relative risk for more than 30 days of hospitalization.
ConclusionThe postoperative period is critical for the successful treatment of head and neck oncology patients. PCF and flap/cutaneous necrosis were the principal complications which worsened the outcomes during this critical period. The early recognition and treatment of these complications is crucial.
Analizar el impacto de las complicaciones infecciosas en el período posoperatorio de las cirugías oncológicas mayores de cabeza y cuello, y estudio de los agentes microbianos implicados.
MétodosEstudio retrospectivo realizado en un instituto oncológico, en pacientes que desarrollaron complicaciones infecciosas después de la cirugía oncológica mayor de cuello, entre octubre de 2012 y mayo de 2016 (44 meses). Entre otros se recogieron el estadio TNM, la puntuación ASA, el índice de masa corporal, las comorbilidades, los hábitos tóxicos, los niveles de hemoglobina pre y postoperatoria, los niveles séricos de albúmina, los tratamientos previos a la cirugía, la duración de la hospitalización y los microorganismos aislados, así como las complicaciones sufridas y la tasa de mortalidad.
ResultadosEn este período se realizaron 761 cirugías cervicales mayores. De estas, 96 pacientes presentaron complicaciones (12,6%). Las que con mayor frecuencia se registraron fueron la fístula faringocutánea (FFC) (56%) y la neumonía nosocomial (23%). Fueron aislados 26 tipos de microorganismos, siendo la Pseudomonas aeruginosa la más frecuente (15%). Se registraron 12 fallecimientos. Tras el estudio estadístico con regresión lineal múltiple, se detecta que la necrosis cutánea o del colgajo y la FFC fueron las complicaciones con un mayor impacto estadístico en la estancia hospitalaria. Asimismo, fueron los factores que más influyeron en las hospitalizaciones de 30 días o más.
ConclusiónUna buena evolución durante el período postoperatorio es fundamental para obtener éxito en el tratamiento de los pacientes oncológicos de cabeza y cuello. La FFC y la necrosis de colgajo o cutánea constituyeron las principales complicaciones con un mayor impacto en los resultados obtenidos. La detección precoz de estas complicaciones, así como su tratamiento, son cruciales.