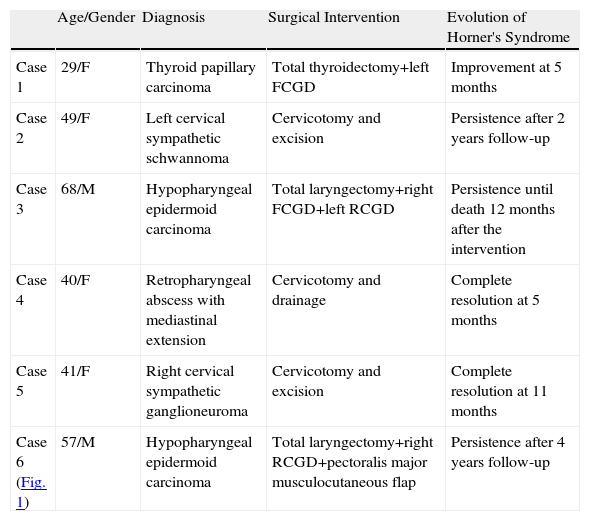
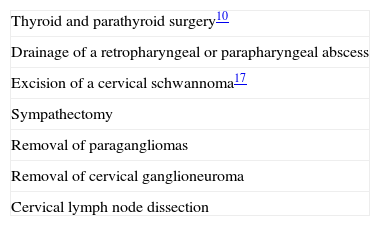
Horner's syndrome (oculosympathetic paresis) is characterised by the classic triad of ipsilateral palpebral ptosis, pupillary miosis and facial anhidrosis. The syndrome arises from the interruption of sympathetic innervation to the eye and adnexa at varying levels. It is a rare complication of neck surgery.We describe 6 patients who presented with Horner's syndrome after a neck procedure in our department during the last 5 years and review the different neck procedures that can cause it.
El síndrome de Horner (oculosimpatoparesis) consiste en la clásica triada de ptosis palpebral, miosis pupilar y anhidrosis facial ipsilateral. El síndrome resulta tras la interrupción de la inervación simpática del ojo y de los anexos oculares a diferentes niveles, siendo una complicación poco frecuente de la cirugía cervical.
Describimos los casos de 6 pacientes que presentaron síndrome de Horner tras cirugía cervical en nuestro servicio en los últimos 5 años y una revisión de los diferentes procedimientos cervicales que producen dicha entidad.