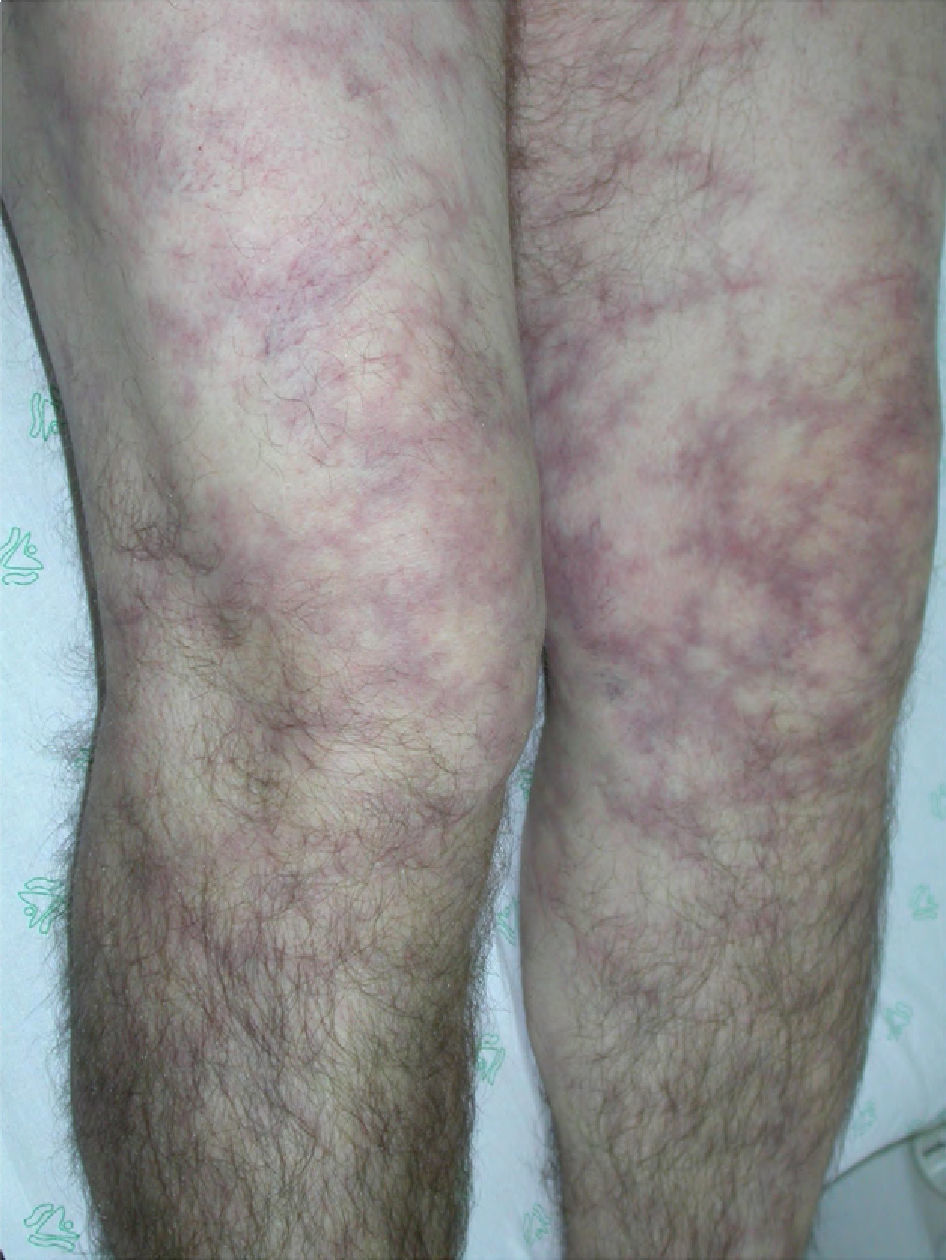
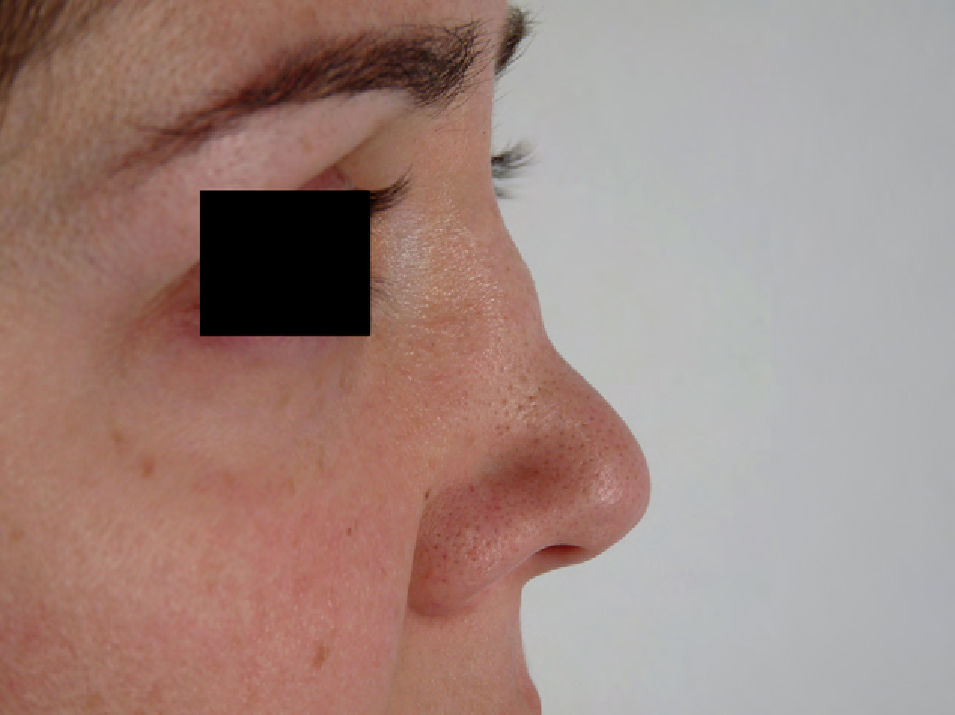
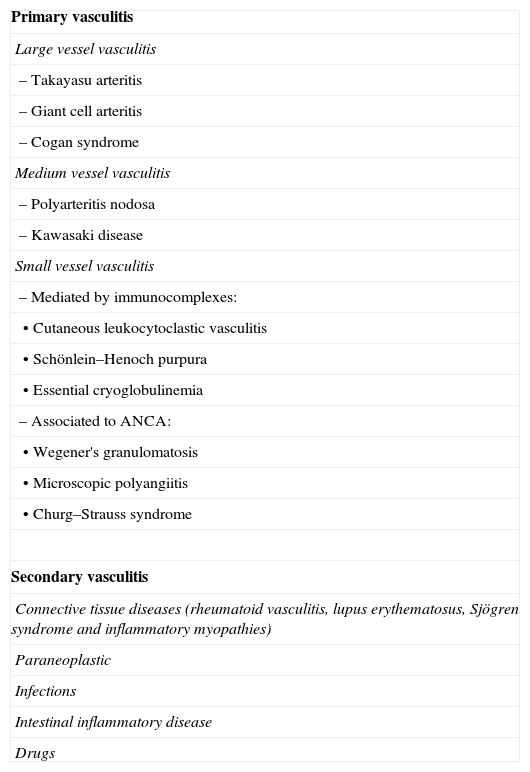
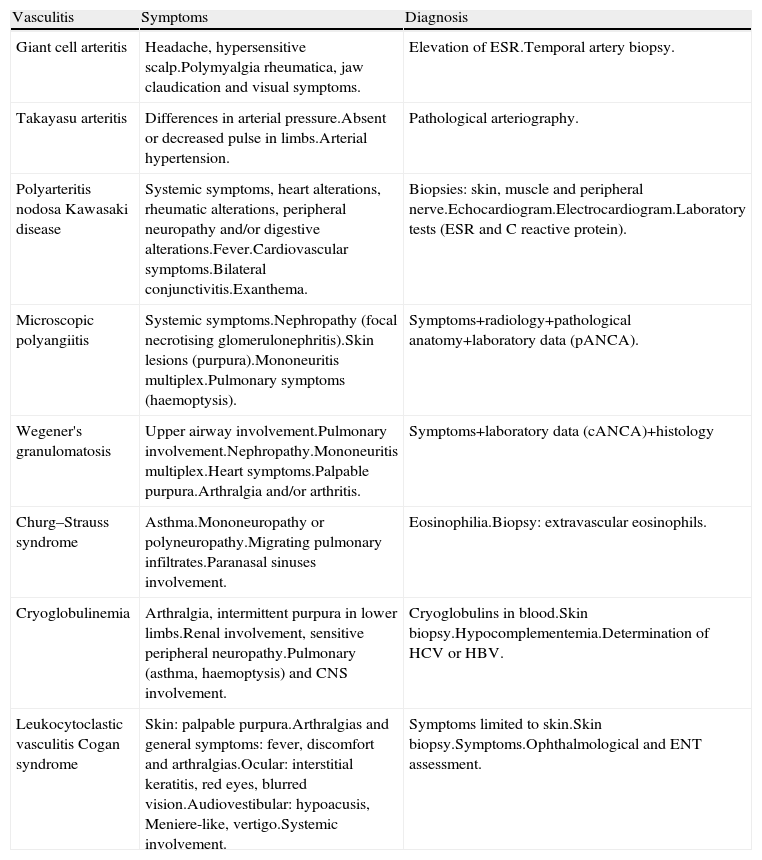
Systemic vasculitis is a heterogeneous group of diseases of various aetiologies and manifestations. In general, the clinical results derive from ischemia caused by vascular inflammation, which depends on the organ affected. Such vasculitis cases are classified according to the classification of the Chapel Hill conference. They can present with relative frequency as ENT manifestations in both their debut and throughout their evolution. Consequently, the ENT specialist should include them in the differential diagnosis in patients with ENT manifestations that are difficult to control or of atypical presentation. Our objective was to review the most common ENT clinical signs and symptoms in each of these diseases.
Las vasculitis sistémicas son un grupo muy heterogéneo de enfermedades de diversas etiologías y manifestaciones. En general, la clínica se deriva de la isquemia producida por la inflamación vascular de la cual depende el órgano afecto. Se clasifican según el consenso de la conferencia de Chapel Hill. Se pueden presentar con relativa frecuencia como manifestaciones otorrinolaringológicas tanto en su debut como a lo largo de su evolución, por lo tanto deben incluirse en el diagnóstico diferencial del especialista en otorrinolaringología en pacientes de difícil control o presentación atípica de manifestaciones ORL. Es nuestra intención revisar la clínica otorrinolaringológica más frecuente en cada una de estas enfermedades.