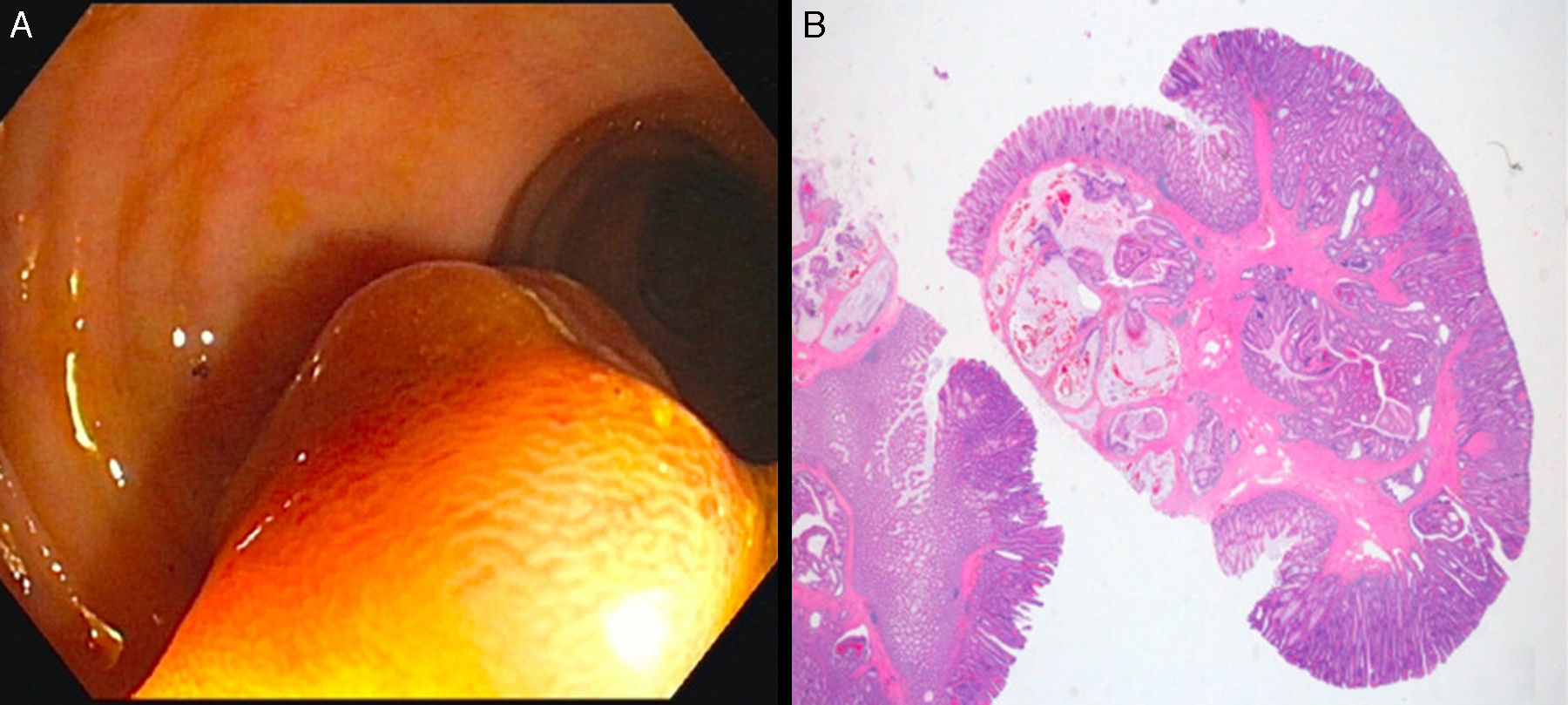
A 69-year-old man underwent colonoscopy following a positive fecal occult blood test, in which a 20mm pedunculated polyp with thick stalk (Fig. 1A) was found in the distal sigmoid colon. The polyp was resected by conventional snare polypectomy without complications. The microscopic evaluation revealed a mixed polyp (Fig. 1B) with hyperplastic glands, low-grade dysplastic areas and focal superficial high-grade dysplasia, containing many lobules of crypts and glands in the polyp stalk, enclosed by bundles and fascicles of muscularis mucosae. These lobules had an area of continuity with the superficial mucosa as well as identic cytological (with only slight focal atypia) and immunohistochemical (strong positivity for E-Cadherin) features compared with the superficial glands of the polyp. Complex and defective muscularis mucosae without desmoplasia surrounded the lobules, sometimes rimmed by sparse lamina propria with inflammation. Some glands had abundant extracellular mucus. Signs of remote hemorrhage with hemosiderin deposition and vascular congestion were observed throughout the stalk (Fig. 2). A diagnosis of adenoma with misplaced epithelium (pseudo-invasion) was made.
(A) Endoscopic image showing a 20mm pedunculated polyp with thick stalk; (B) histological image showing a pedunculated polyp with thick stalk having numerous glands in the muscularis mucosae and submucosae, some with mucus dilatation, surrounded by an haphazard and fibrotic muscularis mucosae with congestive ectatic vessels, showing continuity with the overlying mucosae (HE, 1.5×).
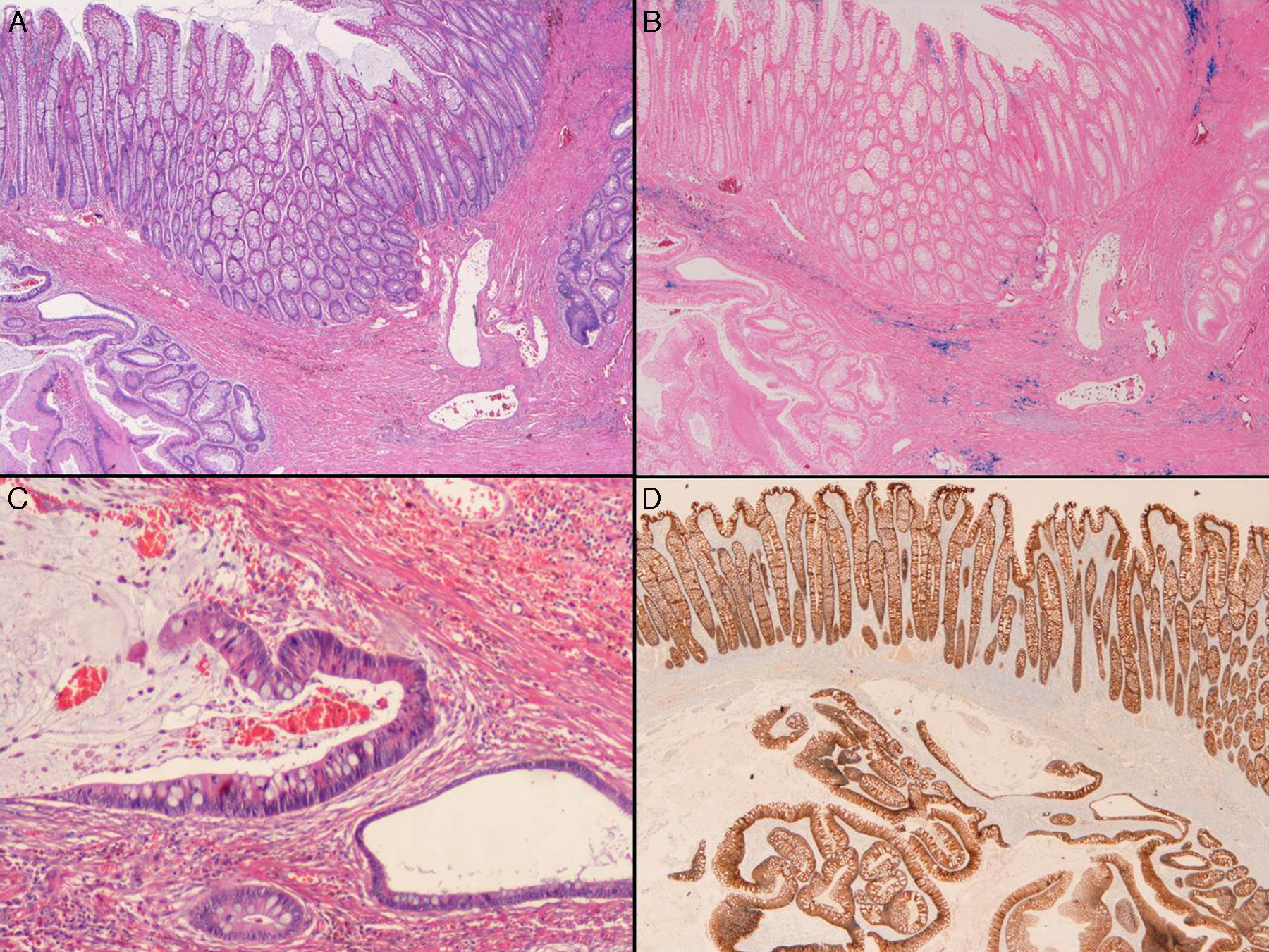
The crypts within muscularis mucosae are lobular and well demarcated (left side) or more irregular (right side) [A – HE, 20×] and multiple foci of hemosiderin are seen throughout the muscularis mucosae [B – Perls, 20×]. Some glands are irregular and dilated by extracelullar mucus [C – HE, 100×]. There is no decreased intensity of E-Cadherin in the misplaced epithelium [D – 20×].
Pseudo-invasive adenomatous polyps result from trauma and prolapse of adenomatous epithelium in areas of defective or weak muscularis mucosae into their stalk.1 They are rare lesions and may be unfamiliar to some endoscopists.2
The distinction between pseudoinvasion and invasive carcinoma by endoscopic and morphologic examination may be very difficult.3
The pathological criteria of misplaced epithelium in hyperplastic as well as adenomatous polyps include: typical localization in the sigmoid colon; presence of crypts in the submucosa and/or stalk more often lobular and well defined than irregular; invariable circumscription of the glands by lamina propria and a defective muscularis mucosae with fibromuscular splaying; frequent vascular congestion, signs of recent hemorrhage and focal or obvious continuity with the superficial mucosal epithelium; occasional chronic inflammation and/or granulation tissue and hemosiderin deposition indicating remote hemorrhage. No morphological aspects of muscularis mucosae or submucosa by the neoplastic epithelium (as desmoplasia or frank atypia or pleomorphism of the epithelium) should be seen.1,4
The presence of dissecting mucin can be worrisome but it may be present in pseudoinvasive lesions and should not by itself mean malignancy.2 In difficult cases the use of immunohistochemical stains can help as Collagen type IV strongly stains the basement membrane that continuously surrounds the misplaced epithelial nests and E-Cadherin shows the same staining intensity as the overlying polyp.5,6
The main differential diagnosis of adenoma with misplaced epithelium is an adenoma with invasive adenocarcinoma. The diagnosis between them depends on pathological findings. In invasive adenocarcinoma there is usually: more significant cytological atypia in the invasive glands; glands with irregular and infiltrative nature, not surrounded by lamina propria and importantly with desmoplastic stromal reaction; presence of small angulated glands and isolated infiltrative cells; hemosiderin restricted to head of the polyp; weak and discontinuous collagen type IV and decreased E-Cadherin staining compared to the overlying adenoma, contrary to nuclear p53 which can be increased in the infiltrative component.1,5,7 The utility of a new immunhistochemical stromal marker such as MMP-1 showing increased staining in the desmoplastic stroma that surrounds the glands has been highlighted.5 Invasive adenocarcinoma may occur throughout the colon, whereas adenoma with misplaced epithelium is preferentially localized to the sigmoid colon.6
Given the stress the term “pseudo-invasion” can potentially cause to a physician unware of this entity or the patient and taking into account the pathogenesis of this lesion the term misplaced epithelium in an adenoma or hyperplastic polyp is preferred.1
It is important for clinicians and pathologists to be aware of pseudoinvasive adenomatous polyps and recognize their histopathologic characteristics, since the recognition of these lesions may prevent unnecessary surgical treatments.3
Conflict of interestThe authors do not have any interest which might be interpreted as influential in this review. This revision did not receive any support from corporations industrial or private.






![The crypts within muscularis mucosae are lobular and well demarcated (left side) or more irregular (right side) [A – HE, 20×] and multiple foci of hemosiderin are seen throughout the muscularis mucosae [B – Perls, 20×]. Some glands are irregular and dilated by extracelullar mucus [C – HE, 100×]. There is no decreased intensity of E-Cadherin in the misplaced epithelium [D – 20×]. The crypts within muscularis mucosae are lobular and well demarcated (left side) or more irregular (right side) [A – HE, 20×] and multiple foci of hemosiderin are seen throughout the muscularis mucosae [B – Perls, 20×]. Some glands are irregular and dilated by extracelullar mucus [C – HE, 100×]. There is no decreased intensity of E-Cadherin in the misplaced epithelium [D – 20×].](https://static.elsevier.es/multimedia/02105705/0000004000000002/v1_201702050027/S0210570516000133/v1_201702050027/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)

