To determine the factors associated with the development of infectious complications in patients undergoing prostatectomy for benign or malignant prostatic disease in Hospital Universitario Mayor.
Materials and methodsA descriptive cross-sectional study was conducted between 2012 and 2013 on 866 patients subjected to prostate surgery. Univariate and multivariate analyses were performed using logistic regression analysis of perioperative variables using the statistical analysis program Wizard for Mac.
ResultsA total of 284 patients (32.7%) received preoperative prophylaxis, and 167 (19.3%) patients had permanent urinary catheter. There were 89 (10%) patients with Diabetes Mellitus. Complications were identified in 149 (17.2%) patients, and among these, 59 (65.5%) had a urinary infection, 21 (23.3%) patients had orchiepididymitis, and 10 (11.1%) had a surgical wound infection. In the bivariate analysis the presence of diabetes mellitus was significantly associated with the development of UTI, OR 2.04, p=0.025. The presence of asymptomatic bacteriuria was associated with the development of vesicocutaneous fistula (p=0.00, OR 1.91), and the occurrence of surgical wound infection (p=0.004, OR 12.6). It was found that failure to use preoperative prophylactic antibiotics is associated with the formation of vesicocutaneous fistula (OR 0048, p=0.04).
ConclusionsDiabetes mellitus patients are at increased risk of infectious complications, such as urinary tract infection or orchiepididymitis. The presence of asymptomatic bacteriuria is associated with a higher frequency of surgical wound infection. There was no relationship between patients with permanent urinary catheter use and the development of infectious complications.
Determinar los factores asociados a complicaciones infecciosas postoperatorias en pacientes sometidos a cirugía de próstata por enfermedad benigna y maligna en el Hospital Universitario Mayor.
Materiales y métodosEstudio descriptivo tipo transversal. Se incluyó a 866 pacientes intervenidos por enfermedad prostática benigna y maligna entre el año 2012 y el año 2013 en el Hospital Universitario Mayor. Se realizó un análisis estratificado y multivariado por medio de regresión logística con el programa SPSS statistics V20.
ResultadosLa prevalencia de bacteriuria asintomática fue del 21%; 284 pacientes (32,7%) recibieron tratamiento antibiótico días previos a la cirugía. Los portadores de sonda en el estudio fueron 167 pacientes (19,3%) y los pacientes con diabetes mellitus 89 (10%). Se identificó a 19 pacientes (12,6%) con complicaciones; dentro de ellas 85 pacientes presentaron infección del tracto genitourinario y 10 (11,1%) pacientes tuvieron infección de herida quirúrgica. En el análisis bivariado se evidenció asociación estadísticamente significativa entre la presencia de diabetes mellitus y el desarrollo de infección del tracto genitourinario en menores de 65 años sometidos a RTU (p=0,025; OR: 2,04).
ConclusionesLa diabetes tipo 2 no representa diferencias estadísticamente significativas para el desarrollo de complicaciones infecciosas en el postoperatorio.
Interventions on the urinary system require a detailed evaluation of the risk factors associated with postoperative complications in general and with urological infections in particular. Several studies have described that infections in the postoperative period depend on various factors characteristic of the patient, the procedure, and the hospital environment.1–5
According to the patient classification system of the American Society of Anesthesiology, the presence of diabetes mellitus, the use of urinary catheter, and asymptomatic bacteriuria (AB) are some of the most identifiable and described risk factors. However, AB is the most changeable risk factor in terms of its operational definitions and preoperative prophylaxis.2,6–11 On the other hand, its management is changeable in different reference sites.
Therefore, this study aims to determine the socio-demographic, microbiological, and clinical variables associated with the development of infectious complications in patients subjected to prostate surgery for benign and malignant prostatic disease.
Materials and methodsIn order to fulfill the general objective of our research, an observational, cross-sectional study was carried out to find associations between the different factors evaluated and the postoperative infectious outcome.
Data collectionThrough an authorized access to the operating system of the Hospital Universitario Mayor, we performed a search of clinical records of male patients subjected to prostate surgery, transurethral resection of the prostate (TURP), open adenomectomy (OA), and radical prostatectomy (RP) between 2012 and 2013, and applied to them the inclusion and exclusion criteria described below.
Inclusion criteriaPatients operated between 2012 and 2013 at the Hospital Universitario Mayor for TURP, OA, and RP.
Evidence in clinical records of complications in the postoperative period.
Record of age.
Record of preoperative asymptomatic bacteriuria, and presence and record of extended-spectrum beta-lactamase (ESBL) and non-ESBL germs.
History of the following diseases:
- -
Urolithiasis.
- -
Use of urinary catheter.
- -
Diabetes mellitus.
- -
Heart disease.
- -
Chronic kidney disease.
- -
Neoplasia.
- -
Hospitalization prior to complication in the last 3 months.
- -
Use of antibiotics in the last 3 months prior to complication.
- -
HIV.
Patients admitted to procedure with AB were given a dose of antibiotics according to the germ and sensitivity of the antibiogram one hour before the procedure, subsequently completing 7 days of antibiotics. Those who had negative preoperative urine culture were given a dose of antibiotics according to the hospital protocol (one dose of preoperative antibiotics, first-generation cephalosporin, and subsequently completing four postoperative doses).
Exclusion criteriaPatients who underwent emergency surgeryPatients who presented with complications of organs or systems different from the genitourinary system associated with the procedure.
Population and sample designWe do not know the real prevalence of postoperative infectious complications in patients operated due to benign and malignant prostatic pathology in Colombia. In order to find the highest number of possible associations, we considered working with the total of data.
Subjects were identified in a secondary information source, n=866.
Control of bias and confusionAs our outcome was postoperative infection, we had to adjust the associations for surgical event, age group, and the presence of type 2 diabetes. We performed a stratified analysis to control the confounding variables. Selection bias was controlled by working with the entire population. For possible confusion biases, a multivariate analysis was performed.
Data analysisData analysis was performed using the IBM SPSS statistics software (version 20) and Wizard for Macintosh.
In the first stage of analysis, a demographic description of variables was carried out, using central tendency measures for the case of continuous variables, and percentage and proportion measures for the categorical variables. Subsequently, a stratified analysis was performed looking for statistically significant associations through the chi-square test.
ResultsA total of 866 patients with an average age of 67.64±7.4 years were identified; 66% of the population was over 65 years of age. The most frequently performed procedure was TURP (Table 1). Within the demographic and microbiological characteristics we found that 185 patients (21%) were intervened due to AB, with the most frequently isolated germ being Escherichia coli in 100 patients (11.84%). Beta-lactamase-producing germs were isolated in 47 patients (30%) (Table 2). The most commonly used preoperative antibiotics were cephalosporins in 157 patients (55.2%), sulfa drugs in 44 (15.4%), and carbapenems in 36 (12.6%). In the study population, hospitalization in the 3 months prior to the procedure was documented in 20 patients (2.3%). Only 24 patients (2.77%) received a complete antibiotic regimen prior to the surgical event.
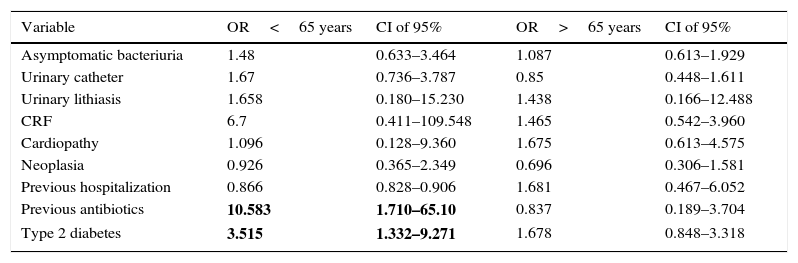
Association for age group.
| Variable | OR<65 years | CI of 95% | OR>65 years | CI of 95% |
|---|---|---|---|---|
| Asymptomatic bacteriuria | 1.48 | 0.633–3.464 | 1.087 | 0.613–1.929 |
| Urinary catheter | 1.67 | 0.736–3.787 | 0.85 | 0.448–1.611 |
| Urinary lithiasis | 1.658 | 0.180–15.230 | 1.438 | 0.166–12.488 |
| CRF | 6.7 | 0.411–109.548 | 1.465 | 0.542–3.960 |
| Cardiopathy | 1.096 | 0.128–9.360 | 1.675 | 0.613–4.575 |
| Neoplasia | 0.926 | 0.365–2.349 | 0.696 | 0.306–1.581 |
| Previous hospitalization | 0.866 | 0.828–0.906 | 1.681 | 0.467–6.052 |
| Previous antibiotics | 10.583 | 1.710–65.10 | 0.837 | 0.189–3.704 |
| Type 2 diabetes | 3.515 | 1.332–9.271 | 1.678 | 0.848–3.318 |
CRF: chronic renal failure.
Bold: statistically significant odds ratio in patients under 65 years of age with a confidence interval of 95%.
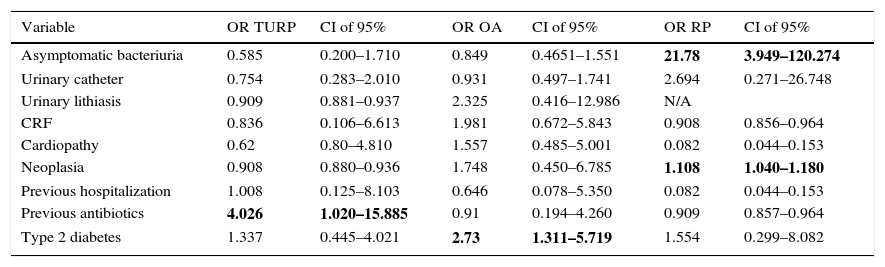
Associations for surgical event.
| Variable | OR TURP | CI of 95% | OR OA | CI of 95% | OR RP | CI of 95% |
|---|---|---|---|---|---|---|
| Asymptomatic bacteriuria | 0.585 | 0.200–1.710 | 0.849 | 0.4651–1.551 | 21.78 | 3.949–120.274 |
| Urinary catheter | 0.754 | 0.283–2.010 | 0.931 | 0.497–1.741 | 2.694 | 0.271–26.748 |
| Urinary lithiasis | 0.909 | 0.881–0.937 | 2.325 | 0.416–12.986 | N/A | |
| CRF | 0.836 | 0.106–6.613 | 1.981 | 0.672–5.843 | 0.908 | 0.856–0.964 |
| Cardiopathy | 0.62 | 0.80–4.810 | 1.557 | 0.485–5.001 | 0.082 | 0.044–0.153 |
| Neoplasia | 0.908 | 0.880–0.936 | 1.748 | 0.450–6.785 | 1.108 | 1.040–1.180 |
| Previous hospitalization | 1.008 | 0.125–8.103 | 0.646 | 0.078–5.350 | 0.082 | 0.044–0.153 |
| Previous antibiotics | 4.026 | 1.020–15.885 | 0.91 | 0.194–4.260 | 0.909 | 0.857–0.964 |
| Type 2 diabetes | 1.337 | 0.445–4.021 | 2.73 | 1.311–5.719 | 1.554 | 0.299–8.082 |
CRF: chronic renal failure; N/A: none of the patients presented with lithiasis.
Bold: statistically significant odds ratio for surgical event with a confidence interval of 95%.
Regarding the associated clinical factors, the proportion of patients with urinary catheter in the study was 19.3%. Type 2 diabetes mellitus was found in 89 patients (10%). Other comorbidities, such as chronic renal failure, neoplasia, heart disease, and HIV, were found in 32.5% of the patients under study.
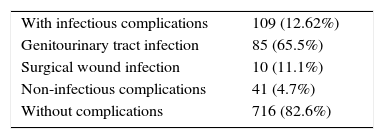
Of the surgical patients, 109 (12.6%) had postoperative complications, such as genitourinary tract infection in 85 (9.8%) and surgical wound infection in 24 (2.8%). Other non-infectious complications occurred in 4.7% of the patients intervened (Table 3).
A stratified analysis was performed for surgical event, the presence of diabetes mellitus, and age group, taking postoperative infection as an outcome. For the purpose of statistical analysis, we re-categorized the variable “postoperative complication,” where we considered all subjects with genitourinary tract and surgical wound infection as “present infection,” and the other values reported were considered as “absent infection.” A statistical significance of 95% was considered for the level of association between variables.
The result of the analysis for surgical event showed that the probability of infection in the postoperative period of TURP was three times higher when there was a history of previous antibiotic therapy. The association with the p-value of the chi-square test was p=0.032 for an alpha of 0.05. As for patients who underwent OA, those who presented with type 2 diabetes had 1.7 times higher risk of developing an infectious outcome in the postoperative period (p=0.06). Asymptomatic bacteriuria was associated with increased postoperative infection in the group of patients subjected to RP (p=<0.001). All patients undergoing radical prostatectomy had a diagnosis of malignancy.
When evaluating the association of variables for the age group, we found that the administration of antibiotics prior to complication caused a nine times higher probability of infectious complications in patients under 65 years of age (p=0.002); at the same time, we found a statistically significant association between diabetes mellitus and postoperative infectious outcome in patients younger than 65 years (p=0.07), as shown in Table 1.
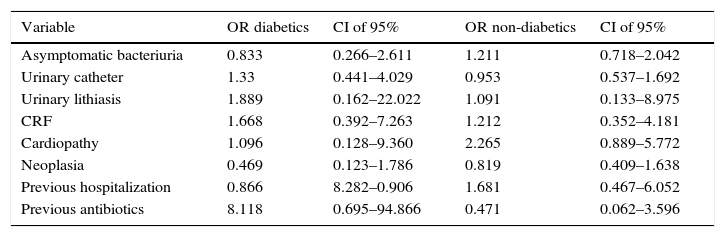
We adjusted the association for the presence of type 2 diabetes mellitus. We found that the presence of heart diseases, chronic renal failure, neoplasia, urinary catheter, AB, previous antibiotics, and previous hospitalization do not represent a statistically significant difference between diabetics and non-diabetics. Due to this, based on this analysis we can affirm that the development of postoperative infections in diabetic patients does not vary with respect to non-diabetic patients (Table 4).
Association for the presence of diabetes.
| Variable | OR diabetics | CI of 95% | OR non-diabetics | CI of 95% |
|---|---|---|---|---|
| Asymptomatic bacteriuria | 0.833 | 0.266–2.611 | 1.211 | 0.718–2.042 |
| Urinary catheter | 1.33 | 0.441–4.029 | 0.953 | 0.537–1.692 |
| Urinary lithiasis | 1.889 | 0.162–22.022 | 1.091 | 0.133–8.975 |
| CRF | 1.668 | 0.392–7.263 | 1.212 | 0.352–4.181 |
| Cardiopathy | 1.096 | 0.128–9.360 | 2.265 | 0.889–5.772 |
| Neoplasia | 0.469 | 0.123–1.786 | 0.819 | 0.409–1.638 |
| Previous hospitalization | 0.866 | 8.282–0.906 | 1.681 | 0.467–6.052 |
| Previous antibiotics | 8.118 | 0.695–94.866 | 0.471 | 0.062–3.596 |
CRF: chronic renal failure.
Subsequently, by applying a multinomial logistic regression model, where we assumed as dependent variable the postoperative infectious outcome, and using as covariates age, the presence of diabetes, and surgical event, in relation to the other factors studied, we found a statistically significant association between the presence of type 2 diabetes and the surgical event with a value of p=0.021 and p=0.010, respectively.
DiscussionTo the best of our knowledge, this is the largest study that exists in a Colombian population in terms of predictors of an infectious outcome in patients subjected to prostate surgery. Our results evidence a prevalence of 21% of AB, which is comparable to the results obtained by the Saudi Center for Organ Transplantation7 and to the guidelines of the American Society of Infectious Diseases.3 In the population older than 70 years, the prevalence of AB is between 6 and 15% and in those with permanent urinary catheter is up to 100% of the cases.1,3
According to the review of Bjerklund et al.12 of the European Guidelines on Urological Infections, and the report by the Saudi Center for Kidney Transplantation, AB is a risk factor for developing an unfavorable postoperative outcome (p=0.037).7 In our study, we found that the population with AB had an increased risk of postoperative infection only in the subgroup of radical prostatectomy, with an OR of 21.58, IC of 95%, 3.949–120.274, p<0.001. However, the type of the isolated germ or the ability to produce extended-spectrum beta-lactamase had no statistically significant difference regarding the postoperative infectious outcome. Thus, this study evidenced that AB increases the risk of infection in the postoperative period of patients subjected to radical prostatectomy; however, no association with postoperative infection was found by adjusting for age and the presence of type 2 diabetes.
Patients with type 2 diabetes had a probability of a postoperative infectious outcome when evaluated in the subgroup of TURP and in patients younger than 65 years.1,3,9,13–15 Although it is true that in our stratified analysis we evidenced an increased risk of postoperative infection when adjusted for type 2 diabetes, we did not find a statistically significant association between the diabetic and non-diabetic groups. Therefore, we can conclude that type 2 diabetes in our study is not associated with differences in the development of postoperative infections.
According to the ORENUC classification of risk factors, proposed by the EAU Section of Infections in Urology, having a permanent urinary catheter is a Category C condition, which determines an increased risk of postoperative infection and unfavorable outcome for the patient.8,12 Within the population, 19% (167 patients) had a permanent urethrovesical catheter. The data evaluated in the present study did not evidence a statistically significant association for postoperative infection.
Taking as reference the different series found in the literature that point to the preoperative evaluation of preventable risk factors in urological surgery, it was found that the risk factors associated with the patient, such as advanced age, immunosuppression states, the use of permanent catheter, previous active infection, and previous hospitalization, are the most determinant in terms of postoperative complications.3,5,7–9
Other comorbidities, such as the presence of neoplasia, chronic renal insufficiency, and heart disease, were not representative in terms of the postoperative infectious outcome. Although it could be appreciated that patients with chronic renal failure had a higher incidence of postoperative infections. Immunosuppression states, taking HIV as an index pathology, were prevalent in only three patients in the sample. As it is a not very representative sample within our study population, it was not possible to establish a significant correlation with a postoperative infectious outcome.
Further studies are required to determine whether the evaluation of variables as statistically non-significant was due to their low prevalence in the study population.
This study has some limitations. Its character and retrospective design limits the quality of data obtained in the clinical records. On the other hand, the rate of infectious complications and AB was low, which is in line with the findings in other cohorts in the literature. Some of the variables of the study were not very prevalent, which could explain the absence of association with the outcome in some of them. Finally, this study included patients with benign and malignant prostate disease; malignancy was included as a variable without finding any statistically significant association with the outcome.
ConclusionsBased on the statistical analysis of our population we can conclude, with a statistical significance of 95%, that the presence of type 2 diabetes mellitus did not represent statistically significant difference in the development of postoperative infections after prostate surgery. However, we can infer with the same significance that in patients under 65 years of age subjected to TURP and in patients undergoing OA, it represents a 2.5 and 1.7 times higher probability of presenting postoperative infections, respectively. Pre-complication antibiotics in patients under 65 years of age submitted to TURP was also statistically associated with the infectious outcome.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article
FinancingNone.
Conflict of interestsNone.