Primary breast lymphoma (PBL) represents a rare form of breast malignancy, with diffuse large B-cell lymphoma (DLBCL) emerging as the predominant histological subtype. Despite advancements, treatment strategies remain contentious.
ObjectiveThis study aims to succinctly outline the clinicopathological and immunohistochemical characteristics of PBL while appraising available therapeutic modalities.
MethodsRetrospectively, 22 PBL cases from 2003 to 2021 were culled from pathological records at the Salah Azaiez Institute. Immunohistochemistry was employed to discern DLBCL subtypes.
ResultsMedian age stood at 58, with a predominance of 16 female patients over 6 males, notably with over 50% of women being post-menopausal. Clinical manifestation primarily involved a unilateral right-sided breast mass, with concurrent lymph node involvement detected in 10 cases at diagnosis. Radiological data were available for 6 cases, revealing DLBCL as the prevailing pathological subtype in 16 cases (73%). Non-germinal center B-cell type was notably discerned in 9 out of 16 PB-DLBC cases. Treatment modalities encompassed surgery in 5 patients, chemotherapy in 7, and radiotherapy in 3 cases. Among treated individuals, 7 experienced recurrences, 5 of them had DLBCL.
ConclusionDespite its rarity, PBL warrants careful consideration due to its notably aggressive nature, mandating a clear distinction from breast carcinoma owing to differential therapeutic approaches and prognoses. Hence, an accurate diagnosis grounded in thorough pathological and immunohistochemical examination is imperative for tailoring optimal treatment strategies, thereby potentially enhancing outcomes.
El linfoma primario de la mama (LPM) representa una forma rara de neoplasia de la mama, siendo el linfoma difuso de células B grandes (DLBCL) el subtipo histológico predominante. A pesar de los avances, las estrategias terapéuticas siguen siendo controvertidas.
ObjetivoEl objetivo de este estudio fue destacar sucintamente las características clinicopatológicas e inmunohistoquímicas del LPM, así como evaluar las modalidades terapéuticas disponibles.
MétodosSe seleccionaron retrospectivamente 22 casos de LPM, de 2003 a 2021, de los registros patológicos del Instituto Salah Azaiez. Se utilizó inmunohistoquímica para discernir los subtipos de DLBCL.
ResultadosLa edad media fue de 58 años, con predominancia de 16 mujeres sobre 6 varones, siendo más del 50% de las mujeres notablemente postmenopáusicas. La manifestación clínica se compuso principalmente de una masa unilateral en el lado derecho de la mama, detectándose afectación ganglionar concurrente en 10 casos durante el diagnóstico. Se dispuso de datos radiológicos en 6 casos, que revelaron DLBCL como subtipo patológico prevalente en 16 casos (73%). Se detectó el tipo de células B de los centros no germinales en 9 de los 16 casos de PB-DLBC. Las modalidades terapéuticas incluyeron cirugía en 5 pacientes, quimioterapia en 7, y radioterapia en 3 casos. Entre los individuos tratados, 7 experimentaron recidivas, y 5 de ellos manifestaron DLBCL.
ConclusiónA pesar de ser infrecuente, el LPM merece una consideración detenida debido a su naturaleza notablemente agresiva, siendo imperativa su distinción clara del carcinoma de mama, debido a los enfoques y pronósticos terapéuticos diferenciales. Por ello, es imperativo un diagnóstico preciso basado en el examen patológico e inmunohistoquímico exhaustivo para diseñar las estrategias terapéuticas óptimas, y así mejorar potencialmente los resultados.
Primary breast lymphoma (PBL) is a rare condition, accounting for less than 0.5% of all breast malignancies and for 2% of extra nodal lymphomas.1,2 It is defined as a malignant lymphoma primarily within the breast without the prior history of lymphoma, with or without regional lymph node involvement.
PBL predominantly affect post-menopausal women, with a peak of incidence in the sixth decade of life.3 However, it can occur in younger, pregnant, or lactating women.
Although rare, cases of PBL in men have been documented.4 Clinically, the most common presentation is an asymptomatic unilateral mass of the breast. Bilateral involvement, while uncommon, is affecting mostly younger women, and is characterized by a more aggressive course.3,5 Radiologically, PBL may present with incidental findings on mammography in 10%–20% of cases. Typically, mammography reveals a high-density, well-circumscribed mass without spiculation or calcifications.6 The distinction from an invasive breast cancer can be challenging and final diagnosis is made either on core or excision biopsy. The predominant histopathological type is diffuse large B-cell lymphoma (DLBCL). However, any type of lymphoma can occur as PBL, with a site-specific histological subtype which is breast implant-associated anaplastic large cell lymphoma. Because of the rarity of PBL, there is no standard therapy regimens. Treatment modalities depend on the specific type of lymphoma and include surgery, radiotherapy (RT), chemotherapy (CT), and immunotherapy (IT). Survival rates vary largely in published series and seem to be improved with modern treatments such as Rituximab.7 However, treatment outcomes factors are still not well identified due to limited data.
This study aims to evaluate the clinicopathological and immunohistochemical characteristics of PBL within a Tunisian population.
Material and methodsPathological reports of Salah Azaiez institute's database were at first screened using key words: “Lymphoma” and “Breast”. 27 pathological reports of patients diagnosed and treated between 2003 and 2021 were included. Reports of lymphoma were then screened in order to select primary and secondary breast lymphomas. Diagnosis of PBL was established according to the criteria described by Wiseman and Liao and modified by Hugh et al. including: both mammary tissue and lymphomatous infiltrate present in close association in an adequate specimen and no evidence of widespread lymphoma or preceding extramammary lymphoma except for simultaneously appearing ipsilateral axillary lymph nodes.8 For DLBCL diagnostic cases, we performed an immunohistochemistry analysis to precise the germinal center or non germinal center DLBCL, according to the system of Hans et al.9 DLBCL cases of CD10(+) or CD10(−), BCL6 (+) MUM1(−) were defined as germinal center B-cell (GCL) type, whereas cases with CD10(−) MUM1(+), regardless of Bcl-6 expression were subclassified as non-GCL or activated B-cell (ABC) type.
Patients with systemic disease with breast involvement were excluded. The clinical data: age, gender, site, tumor size, nodal involvement, imaging and biology findings, treatment modalities, and outcomes were extracted from medical charts and the biopsy request forms when available. The histological type was defined according to the World Health Organization classification. We used the Ann Arbor's system for staging the patients when data were available. Due to the lack of consensus regarding cases with bifocal breast involvement, patients with bilateral disease were considered stage IV.
Ethical considerationsSpecific guidelines of our institution do not require ethical approval for a retrospective study as there is no active or additional interventions performed to the patients. Besides, it lacks of direct participant involvement.
Patient consentVerbal consent for eventual publication is always obtained from all patients followed in our institution as long as patients' data are anonymized to protect patients' confidentiality.
ResultsAmong the 27 pathology reports detailing breast involvement by lymphoma, 22 cases were identified as PBL. Of these cases, 16 (73%) affected women and 6 affected men. Notably, among women, 10 out of 16 (62%) were post-menopausal. The median age at diagnosis was 58 years, ranging from 17 to 83 years. The most common clinical presentation observed was a unilateral palpable breast mass in 21 cases (95%), with only one case exhibiting bilateral involvement diagnosed as DCBCL. Right-sided localization was predominant, noted in nearly half of the cases (55%). Lymphatic node involvement was associated with the diagnosis in 10 cases (45%), with palpable axillary lymph nodes detected in 8 cases and supraclavicular nodes found in 4 cases. The median tumor size measured 40 mm. Regarding radiological characteristics, findings were available for 6 cases. Mammography revealed nodules characterized as round, hyperdense, and poorly defined masses without calcifications. Ultrasonography findings performed in 5 cases, predominantly described masses as hyperechoic structure in 4 cases, ill-defined, and heterogeneous, with one case presenting as a well-circumscribed and hypoechoic mass. Posterior acoustic shadowing was observed in 3 cases, posterior enhancement in 1, and no marked posterior effect was disclosed in 1.
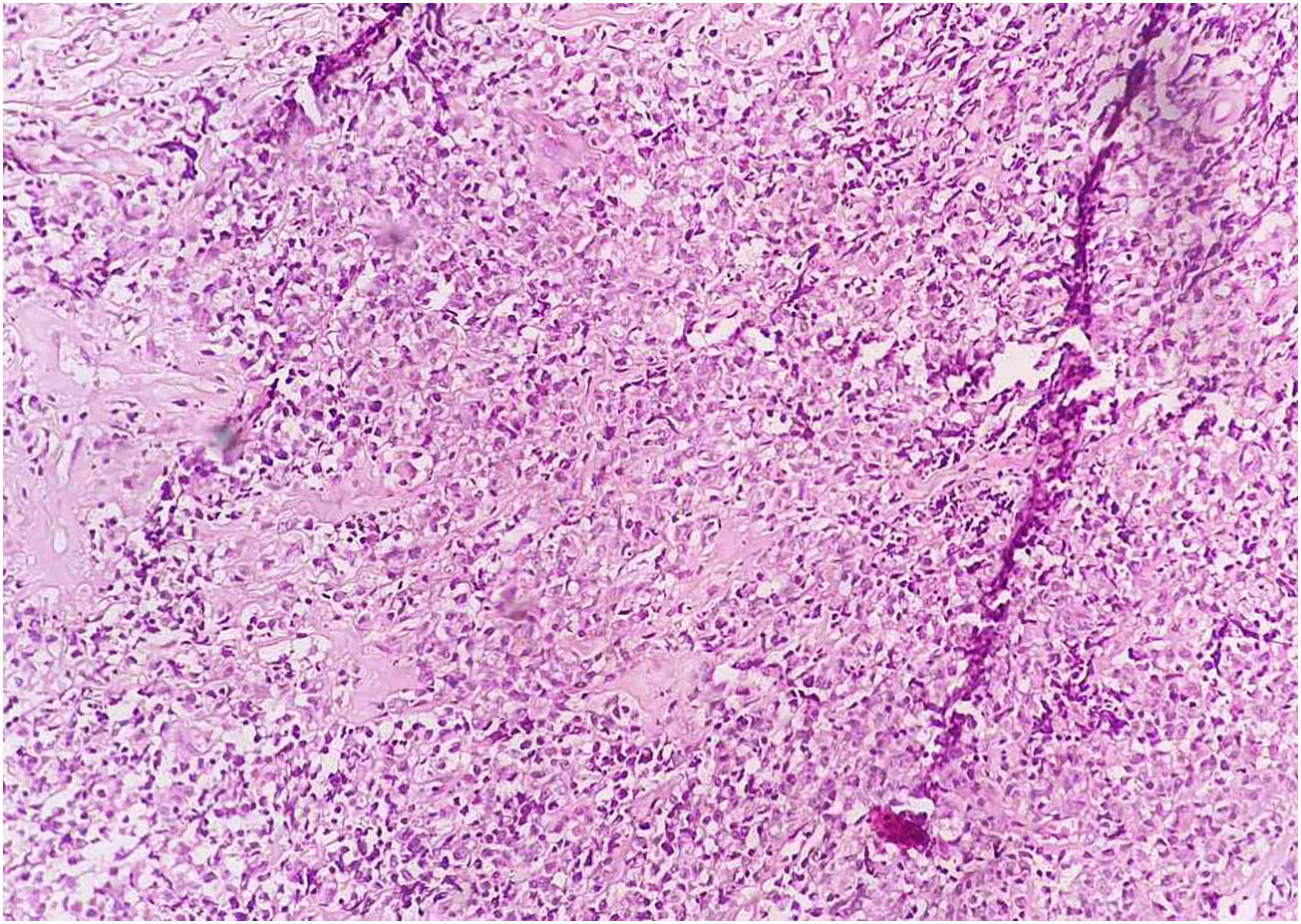
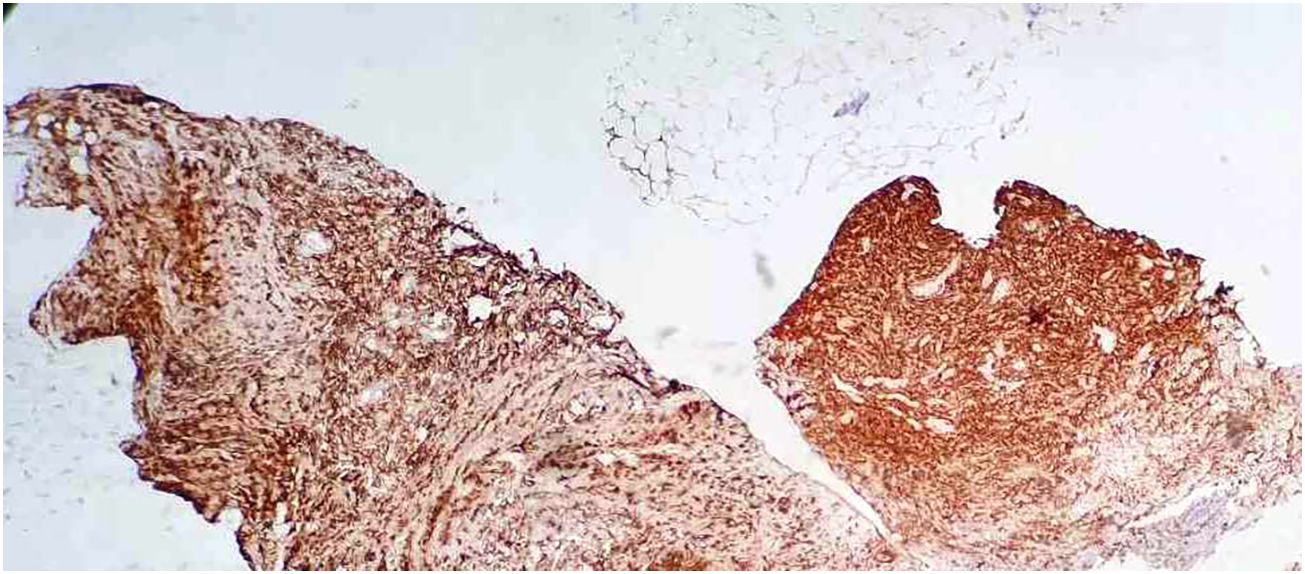
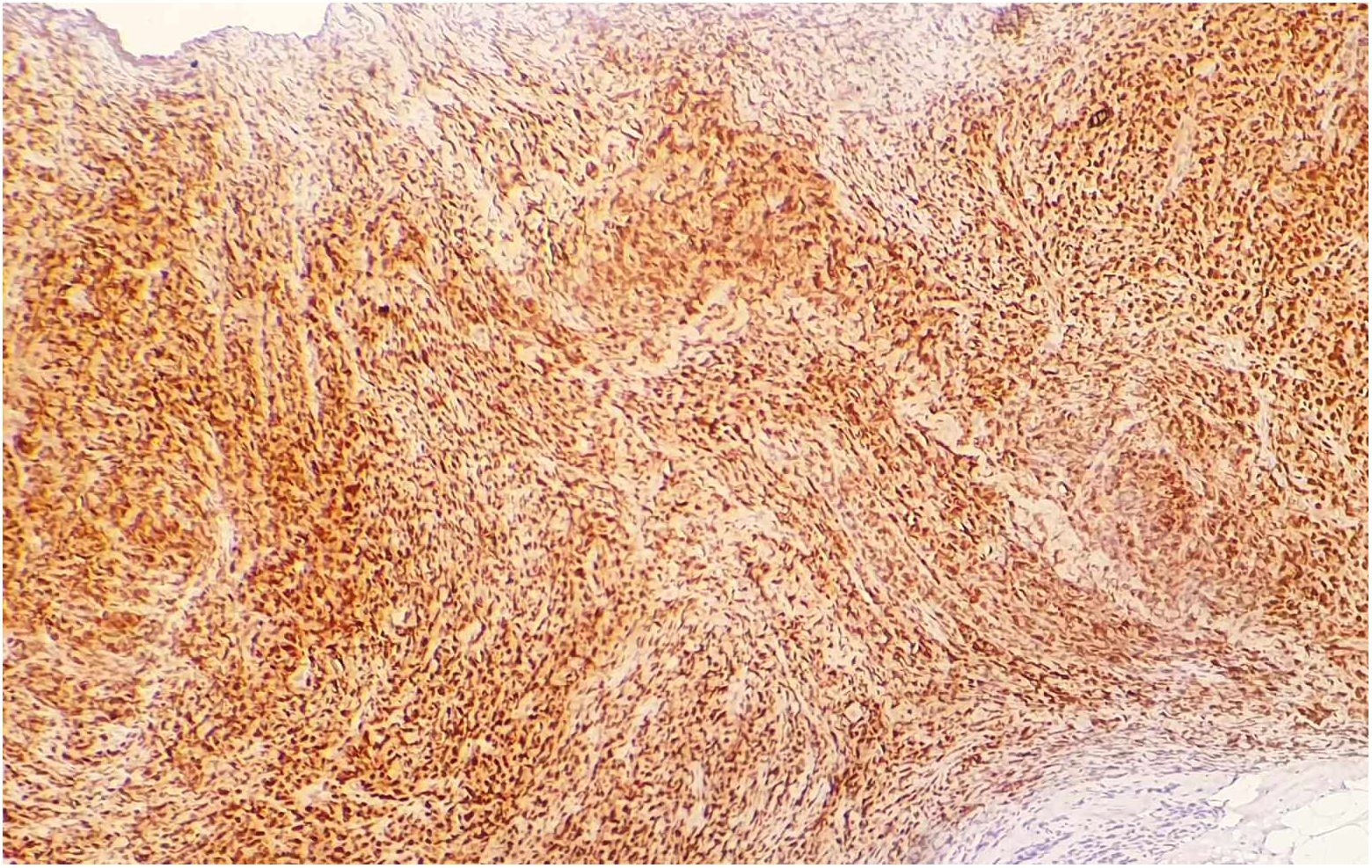
The histopathological types observed in decreasing order were as follows: DLBCL (Figs. 1, 2), detected in 16 cases (73%); T lymphoma NOS in 2 cases (9%); small B-cell lymphoma in 2 cases (9%); lymphoblastic lymphoma in 1 case; and follicular lymphoma in 1 case. Immunohistochemistry analysis conducted for DLBCL cases revealed positivity for CD10 in 9 cases, BCL6 expression in 9 cases, and MUM1 expression in 12 cases (Fig. 3). Among the 16 DLBCL cases, 7 were classified as GCL type and 9 as non-GCL type. Treatment regimens comprised surgery in 5 cases, first-line CT in 7 cases (with 4 cases receiving neoadjuvant treatment), and RT in 3 cases. The chemotherapeutic protocols mainly consisted of cyclophosphamide, doxorubicin (Adriamycin), vincristine (Oncovin), and prednisolone (CHOP) in 6 cases, with 1 case receiving CHOP-bleomycin.
Data concerning therapeutic management were missing in 14 cases, although contact was established with 6 of them. Among these, 2 patients had deceased, while 4 were alive and receiving treatment at another medical center. The median follow-up duration was 8 months. Among the treated patients, 7 experienced recurrences at 2 and 7 months. Of these, 5 had DLBCL, with 2 cases classified as germinal center and 3 as non-germinal center.
DiscussionIn this study, we aimed to delineate the clinicopathological aspects of PBL and investigate the significance of determining the centro-germinative origin of DLBCL within these malignant lymphoproliferative diseases. We analyzed 27 pathology reports of breast lymphoma and identified 22 cases as PBL. It is important to note that secondary breast lymphoma is generally more common than PBL in clinical practice.10 However, our institute serves as a national reference center for breast pathology, and only well-documented cases of PBL are admitted for study with a female predominance. The predominant clinical presentation was a unilateral palpable breast mass in 21 cases (95%), which also was often described in the literature.8,10 A right predominance laterality was classically reported,10–12 which was the same fact in our series (55%) Bilaterality is uncommon in PBL and seems to be a characterization of secondary breast lymphoma,9 and was also noticed in our series with 1 case exhibiting bilateral involvement. Lymph node involvement was observed in 45% of cases, with palpable axillary lymph nodes in 8 cases and supraclavicular nodes in 4 cases. The median tumor size was 40 mm. This was nearly the same finding reported in other series.10 Imaging studies are crucial PBL diagnosis. Radiologically, tumors appeared as round hyperdense masses without calcifications on mammography, and as hyperechoic, ill-defined, heterogeneous masses on ultrasonography. Calcifications and spiculated margins was not observed, this was common in the literature.10–13
Histopathological analysis revealed DLBCL as the most prevalent type (73% of cases), followed by T-cell lymphoma NOS (9%), small B-cell lymphoma (9%), lymphoblastic lymphoma (4%), and follicular lymphoma (4%). Immunohistochemical analysis for DLBCL cases showed positivity for CD10 in 9 cases, BCL6 expression in 9 cases, and MUM1 expression in 12 cases. Among DLBCL cases, 7 were categorized as GCL type and 9 as non-GC type.
Therapeutic protocols predominantly comprised the CHOP regimen (cyclophosphamide, doxorubicin, vincristine, prednisolone), administered in 6 cases, with 1 case receiving CHOP-bleomycin. The median follow-up duration was 8 months, during which 7 treated patients experienced recurrences, with 5 of these cases being DLBCL (2 GCL and 3 non-GCL).
PBL is an uncommon condition that accounts for only 2% of extra nodal lymphomas. The diagnostic criteria for PBL as proposed by Wiseman and Liao in 1972 is challenged and other diagnostic criteria are now added such as ipsilateral supraclavicular lymph nodes.6
Clinically, our results were consistent with previous published data. Most of our patients were post-menopausal women with few cases affecting men, in accordance with prior studies. The median age of patients with PBL ranges from 60 to 65 years. PBL lacks specific clinical presentation in most cases: it presents typically as a painless unilateral mass of the breast with a right-sided predominance and very rare cases of bilateral involvement.10 The median tumor size is 4 cm. Previous studies reported a predominance of stage IE and IIE stage disease.2 Mammography often shows a solitary hyperdense mass, with commonly circumscribed margins. Uncommon mammographic findings have been reported including skin thickening or calcifications.12 Breast ultrasound findings are non-specific and vary from a limited to indistinct hypoechoic round mass or with mixed echogenicity. Posterior acoustic enhancement or shadowing are reported.10
Therefore, imaging features for PBL are not specific without clinical context. PBL diagnosis is confirmed by histological and immunohistochemical examination. Although, fine-needle aspiration is sensitive, the core biopsy is the gold-standard.11,12
B-cell phenotype is more commonly found in PBL, comparing to the T-cell type, with DLBCL as the leading histological subtype.13
As previously reported, in our series, we found DLBCL to be the most common type of PBL, which is consistent with the literature.
Follicular and mucosa-associated lymphoid tissue “MALT” lymphoma are common too and T-cell lymphomas are rare.14
As DLBCL presents the main pathological type of PBL and an aggressive behavior, it was subclassified conferring to the cell of origin into two subgroups: GCL-like and ABC-like or non-GCL.15
These phenotypes were categorized using the Hans immunohistochemical algorithm9 based on the expression of CD10, BCL6, and MUM1 with a threshold of positivity considered to be greater than or equal to 30%: GCL phenotype was defined to be positive for CD10 and BCL6 and non-GC or ABC phenotype was CD10 negative and MUM1 positive. The latter was reported to be more common in PBL.15
In our study, in accordance with the literature, we found that the non-GCL type exhibited a slight majority.
Furthermore, existent literature has demonstrated that this phenotypic distinction has therapeutic and prognostic value since it is associated to a different response to CT and targeted agents with the non-GCL phenotype being correlated to a worse prognosis.15,17 In our study, owing to the reduce number, we could not perform statistical analysis. In our study, recurrences seemed to be more associated with non-GCL than GCL (3 vs 2) but could not be affirmative.
PBL is a hematological malignancy with a significantly different pathogenesis and progression from breast carcinoma, thus their therapeutic management diverge greatly.13
There is no consensus yet regarding the treatment of PBL. According to authors, for PBL, and contrarily to breast carcinoma, surgical resection was not considered as a first option and would not be as advantageous as systemic therapy for lymphomatous tumors. It has been even demonstrated that treating PBL surgically was correlated to a worse outcome and prognosis.13,18
In the present study, 5 PBL patients underwent surgery for initially alleged breast carcinoma, among which 3 have received adjuvant CT according to our available therapeutic management data.
The therapeutic approch for PBL have changed over the past decades. While surgical intervention was the treatment option for PBL, CT is recognized as a more efficient treatment for PBL with the cornerstone of it is a CHOP-based regimen.16,17
Immunochemotherapy combining rituximab (R-CHOP) was stated to generate better outcomes in terms of remission rate, disease-free survival, and overall survival (OS) of PB-DLBCL patients comparing to CHOP CT alone.18 Nevertheless, other small-scale researches reported that no significant difference has been established in survival rate whether rituximab is combined or not to systemic therapy (CHOP).19
RT may be an alternative treatment approach. Although RT can improve local control and progression-free survival of PBL, the OS benefit is inconclusive.16 As for consolidation RT, even its efficiency is still controversial, numerous data exhibited that it may improve survival and decrease local recurrence rate when administered after CT.13,17,20
The limitation of our study is that it is a small-scale retrospective one due to the scarcity of the presented entity with the missing data from patients lost to follow-up, which may weaken the impact of our findings. Nonetheless, it remains of a great implication for clinical guidance.
ConclusionIn summary, despite its rarity, clinicians keep in mind the possibility of PBL in front of a breast lump. PBL is a rare entity with overlapping clinical presentation and imaging findings yet divergent management with that of breast carcinoma. However, accurate diagnosis based on pathological and immunohistochemical examination is crucial to onset the appropriate therapy. The most frequent histological type is DLBCL. More study are needed to determine the clinical impact of an immunohistochemical characterization as non-GCL or GCL.
FundingThe authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval/informed consentInformed consent was obtained from all individual participants included in the study.