Cowden Syndrome belongs to a group of disorders that are associated with germline mutations in the tumor suppressor gene, phosphatase and tensin homolog (PTEN). The prevalence has been estimated to be 1 in 200,000–250,000. However, this prevalence may be underestimated due to many factors. Better understand Cowden Syndrome among our local population to provide genetic counseling and appropriate screening for different types of neoplasms associated to Cowden Syndrome.
Material and methodsCase series analysis based on data maintained by the Breast Cancer and Hereditary Cancer Departments of the AC Camargo Cancer Center, a large specialized hospital in Brazil.
ResultsFive cases are presented according to their diagnostic criteria, cancer rates, and outcomes for Cowden Syndrome.
ConclusionThese cases highlight the need for a multi-institutional evaluation of Cowden Syndrome cases in order to better comprehend its prevalence in Brazil. To improve the outcome of patients with CS, a greater understanding of this syndrome is needed, as well as recognition of the value of periodic screening.
El síndrome de Cowden (SC) pertenece a un grupo de trastornos asociados a las mutaciones germinales en el gen supresor del tumor, homólogo de fosfatasa y tensina (PTEN). La prevalencia ha sido estimada en uno por cada 200.000-250.000 sujetos. Sin embargo, esta prevalencia puede subestimarse debido a muchos factores. Nuestro objetivo es hacer que nuestra población local comprenda mejor el SC para proporcionar asesoramiento genético, así como un cribado adecuado para los diferentes tipos de neoplasias asociadas a dicho síndrome.
Material y métodosAnálisis de una serie de casos basado en los datos mantenidos por los Departamentos de Cáncer de Mama y Cáncer Hereditario del Centro para el Cáncer AC Camargo, un gran hospital especializado de Brasil.
ResultadosSe presentan 5 casos con arreglo a sus criterios diagnósticos, tasas de cáncer y resultados para el SC.
ConclusiónEstos casos subrayan la necesidad de realizar una evaluación multi-institucional de los casos del SC, a fin de comprender mejor su prevalencia en Brasil. Para mejorar el resultado de los pacientes con SC se necesita una mayor comprensión del mismo, así como el reconocimiento del valor del cribado periódico.
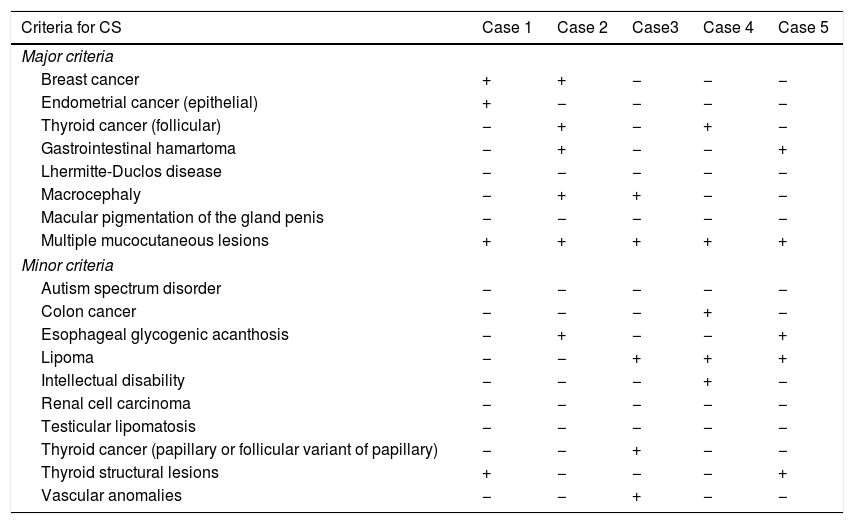
Cowden Syndrome (CS) is an autosomal dominant syndrome associated with germline mutations in the tumor suppressor gene PTEN.1 A set of clinical criteria to aid its diagnosis was not established until 1995 by the International Cowden Consortium (ICC). To date, these criteria continue to evolve and the most recent diagnostic guidelines were published by the National Cancer Comprehensive Network (NCCN)®.1,2 According to NCCN® Guidelines, diagnostic of CS encompass pathogenic/likely pathogenic variant PTEN mutation and/or clinical criteria: three or more major criteria (one must include macrocephaly, Lhermitte-Duclos Disease (LDD) or gastrointestinal hamartomas) or two major and three minor criteria.2 NCCN® clinical criteria are described in Table 1.
Fulfillment of NCCN® diagnostic criteria in our patient cases.
| Criteria for CS | Case 1 | Case 2 | Case3 | Case 4 | Case 5 |
|---|---|---|---|---|---|
| Major criteria | |||||
| Breast cancer | + | + | − | − | − |
| Endometrial cancer (epithelial) | + | − | − | − | − |
| Thyroid cancer (follicular) | − | + | − | + | − |
| Gastrointestinal hamartoma | − | + | − | − | + |
| Lhermitte-Duclos disease | − | − | − | − | − |
| Macrocephaly | − | + | + | − | − |
| Macular pigmentation of the gland penis | − | − | − | − | − |
| Multiple mucocutaneous lesions | + | + | + | + | + |
| Minor criteria | |||||
| Autism spectrum disorder | − | − | − | − | − |
| Colon cancer | − | − | − | + | − |
| Esophageal glycogenic acanthosis | − | + | − | − | + |
| Lipoma | − | − | + | + | + |
| Intellectual disability | − | − | − | + | − |
| Renal cell carcinoma | − | − | − | − | − |
| Testicular lipomatosis | − | − | − | − | − |
| Thyroid cancer (papillary or follicular variant of papillary) | − | − | + | − | − |
| Thyroid structural lesions | + | − | − | − | + |
| Vascular anomalies | − | − | + | − | − |
(+) Yes; (−) No.
The prevalence of CS has been estimated to be 1 in 200,000–250,000 but it may be underestimated due to overlap between the common benign features of CS and the presence of these features in the general population.3 CS is a multi-systemic disease that is associated with a higher risk of developing multiple tumors, such as breast cancer, thyroid cancer, endometrial cancer, colorectal cancer, renal carcinoma, and melanoma.4–6 Moreover, the lifetime risk of presenting breast cancer in association with CS has generally been reported to vary from 25–50%,3 while the cumulative risk of developing breast cancer by age 70 has been reported to be as high as 85.2%.6 The latter is comparable to the risk associated with patients carrying germline mutations in BRCA1 and BRCA2.1
In order to provide genetic counseling and appropriate screening for different types of neoplasms that have an increased incidence in association with CS, it is important to identify affected patients. We present five cases of CS which were identified in Brazilian population according to their diagnostic criteria, cancer rates, and outcomes for CS.
Clinical caseRetrospective study of medical records of AC Camargo Cancer Center (ACCCC, Brazil). Five patients were included: 2 patients met NCCN® clinical criteria for CS and 3 patients had PTEN mutation besides NCCN® clinical criteria. This case series study was approved by the Ethics and Research Committee of the ACCCC in 2018. All patients involved received genetic counseling before and after undergoing genetic testing.
Three patients carried PTEN mutations associated with their health condition: c.388C>T (p.Arg130Ter), c.697C>T (p.Arg233Ter), and c.425G>C (p.Arg142Pro). The first two mutations are pathogenic, while the latter mutation is classified as a variant of uncertain significance (VUS) and was previously reported other patient with PTEN related disorder.4
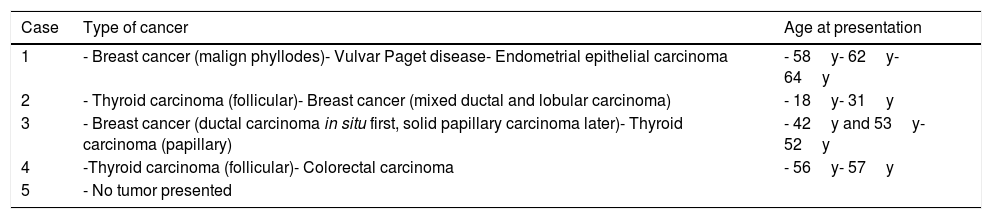
All five patients with a diagnosis of CS had a family history of neoplasms, specially breast and colorectal carcinoma. Four patients had multiple cancers. NCCN® clinical criteria for these five cases are reported in Table 1 and the cancers detected in the four patients are shown in Table 2.
Frequencies of neoplasms and age at presentation.
| Case | Type of cancer | Age at presentation |
|---|---|---|
| 1 | - Breast cancer (malign phyllodes)- Vulvar Paget disease- Endometrial epithelial carcinoma | - 58y- 62y- 64y |
| 2 | - Thyroid carcinoma (follicular)- Breast cancer (mixed ductal and lobular carcinoma) | - 18y- 31y |
| 3 | - Breast cancer (ductal carcinoma in situ first, solid papillary carcinoma later)- Thyroid carcinoma (papillary) | - 42y and 53y- 52y |
| 4 | -Thyroid carcinoma (follicular)- Colorectal carcinoma | - 56y- 57y |
| 5 | - No tumor presented |
Cancer surveillance was offered with mammogram, breast ultrasound and breast magnetic resonance imaging for the female patients. One of them underwent bilateral nipple-sparing mastectomy. All patients underwent thyroidectomy due to the presence of thyroid carcinoma or a goiter. Annual transvaginal ultrasound was offered to one patient who did not undergo a hysterectomy. Colonoscopy, abdomen ultrasound or tomography scan was offered to the entire cohort for colorectal and renal cell cancer screening and an annual dermatologic screening. Three patients underwent an upper digestive endoscopy to follow gastrointestinal polyps or esophageal glycogenic acanthosis.
Regarding patient outcome, all patients are alive, four of them have no signs of neoplasm and one patient developed metastatic follicular thyroid cancer in their skullcap bone.
DiscussionThe true prevalence of CS remains unknown, possibly since multiple clinical manifestations which characterize CS are also common in the general population. Also, most of the studies conducted for CS had small cohorts, making it difficult to estimate the real incidence of this syndrome. In our literature search, no local cohorts of CS have been characterized in the Brazilian population. In recent study conducted by Tan et al.,7 pathogenic germline PTEN mutations were found in approximately 25% of individuals with CS.
CS is a multi-system disease that includes both benign features and an increased risk of malignancies.3–6 Benign manifestations of CS include: multiple gastrointestinal polyps (93%; 44% as hamartomas), dermatologic features (98%), macrocephaly (93%), benign breast (74%) and thyroid (71%) lesions and vascular malformations (18–35%).1,4,8 In this case series, all patients presented with mucocutaneous lesions, gastrointestinal polyps (40% as hamartomas) and goiter (40%). Benign thyroid features incidence may be underestimated among our five cases because three presented with thyroid cancer (Table 1). CS also has components of autism spectrum disorders, mental retardation (IQ ≤75), and LDD.7,9
Regarding the elevated risk of various cancers, the single largest patient series included 21 patients and was reported by Starink8 in 1986. This paper was published prior to establishment of the Consortium diagnostic criteria in 1995. Consequently, some patients reported by Starnik may not have been accurately diagnosed with CS according to updated clinical criteria.3
Four main studies analyzed large cohorts of CS patients and determined cumulative lifetime risks (CLR) and standardized incidence rates (SIRs) of cancer.4,10 Breast cancer is the most prevalent tumor in patients with CS (SIR 25.4–45% and CLR 67.3–85.2%), followed by thyroid carcinoma (SIR 12–51.1% and CLR 21–38%).4,10 In this study, two patients developed breast cancer (the earliest at age 42y) and two presented thyroid cancer (the earliest at 18y) as their first manifestations of the syndrome. An earlier onset for these cancers was observed compared to the general population. Furthermore, the increased risk of breast cancer with CS also encompasses a risk of bilateral breast cancer which has been reported in 25–48% of CS cases.4,5,8,10 In this study, 33% of patients developed bilateral breast cancer that manifested at ages of 42 years and 53 years.
A PTEN-related endometrial cancer risk starts at age 25 and it increases to 30% by age 60.4,10 In this study, one patient (20%) presented endometrial carcinoma and another patient submitted to total hysterectomy due to atypical endometrial hyperplasia. Other malignancies related to CS includes colorectal cancer, renal cell cancer, and melanoma. The age at which risk of these tumors becomes a concern is at 50 years.4,10 In this case series, one patient had colorectal cancer at 57 years of age.
CS should be suspected in individuals fulfilling any one major criteria, or any two minor criteria, of the updated guidelines of the NCCN®.2 These patients should be referred for genetic counseling to consider PTEN-testing. Treatments for benign and malignant manifestations of CS are the same as those applied to their sporadic counterparts. The importance of diagnosing CS is that it indicates appropriate screenings for such neoplasms.
Confidentiality of dataThe authors declare that they have followed the protocols of their Institution regarding the publication of patient data.
Conflict of interestsThe authors declare that they have no conflict of interest.
We thank AC Camargo Cancer Center research department for all the support during the writing of this manuscript.