The present article described a clinical case where it was assessed whether aggregation of enamel matrix derivative (EMD) to the procedure of coronary-advanced flap with sub-epithelial connective tissue graft (CAF + SCTG) would improve the amount of root coverage in Miller's class I and II gingival recessions when compared to the same isolated procedure in a patient suffering multiple gingival recessions, in a 6 month time-span. Twelve gingival recessions were included in the study: six treated with (CAF + SCTG + EMD) and six treated with (CAF + SCTG) in different quadrants. At beginning of procedure as well as six months later, the following clinical parameters were measured: gingival recession depth (RD), depth to probing (PD), clinical insertion level (CIL) and width of keratinized tissue (KT) in apex-coronary direction. A p < 0.05 was considered statistically significant. Results established that after a six month procedure CAF + SCTG + EMD and CAF + SCTG produced significant root coverage, respective averages were 2.83 ± 1.16mm (p = 0.001) and 2.50 ± 0.83mm (p = .002). All gingival recessions treated with EMD experienced 100% root coverage, sites treated with CAF + SCTG + EMD exhibited coverage of only 65.3%. When comparing results at six months, better results were observed with CAF + SCTG + EMD with respect to clinical insertion level (p = .02) and root coverage (p = .06). Nevertheless, neither the difference of clinical level insertion nor the gain in root coverage resulted significant. Additionally, no significant differences were observed between PD and KT. Conclusion: The present clinical case did not show additional benefits when EMD were aggregated to the CAF + SCTG in the coverage of multiple Miller's class I and class II gingival recessions.
Se presenta un caso clínico donde se evaluó si la agregación del derivado de la matriz del esmalte (DME) al procedimiento del colgajo de avance coronal con injerto de tejido conectivo subepitelial (CDC + ITCS) mejorarían la cantidad de cobertura radicular en recesiones gingivales clase I y II de Miller comparados con el mismo procedimiento solo, en un paciente con recesiones gingivales múltiples a seis meses. Se incluyeron 12 recesiones gingivales, seis tratadas con (CAC + ITCSE + DME) y seis con (CAC + ITCSE) en diferentes cuadrantes. Al inicio y a los seis meses se midieron los parámetros clínicos tal como profundidad de la recesión gingival (PR), profundidad al sondeo (PS), nivel de inserción clínica (NIC), y ancho de tejido queratinizado en dirección apico-coronal (TQ). Un valor p < 0.05 se consideró significativo. Los resultados mostraron que a los seis meses ambos procedimientos, CAC + ITCSE+ DME y CAC + ITCSE produjeron una significativa cobertura radicular en promedio 2.83 ± 1.16mm (p = 0.001) y 2.50 ± 0.83mm (p = .002), respectivamente. Todas las recesiones gingivales tratadas con el DME tuvieron el 100% de cobertura radicular y sólo el 65.3% de cobertura para los sitios tratados con CAC + ITCSE. Al comparar ambos procedimientos a los seis meses se observaron mejores resultados con CAC + ITCSE + DME en cuanto al nivel de inserción clínica (p = .02) y la cobertura radicular (p = .06); sin embargo, la diferencia del nivel de inserción clínico ni la ganancia en la cobertura radicular mostraron ser significativos. Por otro lado, no se observaron diferencias significativas en la PS y TQ. Conclusión: El presente caso clínico no mostró beneficio adicional cuando se agregó el DME al procedimiento de CAC + ITCSE para la cobertura de recesiones gingivales múltiples clase I y II de Miller.
Gingival recession is defined as exposition of a part of the tooth's root due to the displacement of the gingival margin.1 It is not considered a disease, but rather a defect which prompts the patient to complain about root hypersensitivity,2 poor esthetics3 and root caries.4 It is a trait frequently found in subjects with suitable or deficient oral hygiene,5 it can appear isolated or in several contiguous teeth.6
Self-induced trauma due to vigorous brushing is the main etiologic factor in patients with good oral hygiene, it generally appears in the oral surface in young subjects.5 In patients with inflammation induced by bacterial plaque, gingival recession mainly affects inter-proximal zones.6 Several factors might enhance the presence of gingival recession, such as high muscle insertion, frenum traction and iatrogenic factors related to restorative and periodontal procedures.7
Isolated gingival recession or multiple recessions can be treated with periodontal plastic surgery procedures aimed at placing soft tissue grafts to cover root surfaces, to thus restore acceptable esthetics and decrease root sensitivity.8,9
According to Miller's classification of gingival recessions,10 class I and II gingival recessions are more predictable to achieve root coverage, since in these recessions, inter-proximal tissues remain intact, blood supply for the survival of the graft will be provided from these locations. Success rate is unpredictable for Miller's class II and IV recessions, since there is a loss of inter-proximal tissues which will limit or prevent blood supply to the graft.
Several surgical procedures have been undertaken to achieve root coverage of multiple gingival recessions, among them we can mention coronary-advanced flaps, 11,12 sub-epithelial connective tissue grafts13 connective tissue grafts with tunnel flap,14 all of which provide different rates of success and predictability.15 Nevertheless, the procedure involving a coronary-advanced flap combined with sub-epithelial connective tissue graft (CAF + SCTG), can be considered the gold standard, since this procedure exhibits greater root coverage predictability and greater color homogeneity with surrounding tissues.16
Recently, the use of enamel matrix derivative (EMD) has been applied as clinical treatment to promote periodontal tissues regeneration.17,18 It is a derivative from porcine embryonic enamel and is based on the high homology found between human and porcine enamel proteins, since they mimic the sequence of events involved in root cement formation, favoring thus new insertion of periodontal ligament.19,20 This regenerative concept has also been demonstrated when used in root coverage procedures.21
Topical EMD application in CAF procedures has exhibited suitable results with respect to root coverage, clinical insertion gain and increase of apex-coronal dimension of keratinized tissue.22,23 Nevertheless, other studies could not demonstrate clinical improvement when compared with solely coronal advanced flap.24,25 There are a few studies on EMD application along with CAF + SCTG, where contradictory results have equally been found. Better results have been reported in a controlled clinical study in Miller's class I and II26 recessions, as well as in another study conducted on Miller's27 class III recessions, whereas other studies have reported no benefit whatsoever.28,29
The purpose of the present clinical case was to study whether EMD application during coronal-advanced flap procedures with sub-epithelial connective tissue graft (CAF + SCTG) exerted an additional effect on root coverage of Miller's class I and II recessions in a patient afflicted with multiple gingival recessions.
CLINICAL CASE37 year old female attending the Implantology and Periodontics Clinic at the Graduate and Research School, National School of Dentistry, National University of Mexico (UNAM), due to multiple gingival recessions. She requested coverage of said recessions due to hypersensitivity and esthetic problems. Clinical history did not reveal any systemic condition. During pathological personal history recording, the patient revealed orthodontic treatment with bilateral mandibular orthognatic surgery three years before. Clinical exploration showed Miller's type I, II and III recessions in all quadrants and edge to edge occlusion (Figure 1). X-ray examination showed intact inter-proximal bone crests, periodontal examination revealed plaque-induced gingivitis. The patient exhibited a 22% plaque index and bleeding upon probing in 34% of all sites.
Initial photographs. (A) Right lateral side with multiple Miller's class I and II recessions. (B) The anterior area presented ridge to ridge occlusion and gingival recessions in lateral teeth and upper canines as well as in lower teeth. (C) Left lateral view with class I and II gingival recessions.
The patient was subjected to initial therapy which consisted on oral hygiene advice, calculi removal, tooth polishing, as well as inter-consultation with the Orthodontics Clinic at the same institution in order to correct dental malposition. Three weeks later another assessment was undertaken which revealed a plaque index under 10%.
Surgical treatment plan consisted on root coverage with coronal advanced flap with sub-epithelial connective tissue graft (CAF + SCTG) in the left upper and right lower quadrants and coronal advanced flap with sub-epithelial connective tissue graft along with application of enamel matrix derivative (CAF + SCTG + EMD) in the upper right and lower left quadrants.
The patient was advised on risks and procedures inherent to sub-epithelial connective tissue graft with and without use of EMD when undertaking root coverage. The patient signed an informed consent form before initiating therapy, and was treated in the time span ranging from August 2013 to May 2014.
Clinical measuresClinical measures used as success criteria for root coverage of gingival recession defects were: recession depth (RD) measured from the dentin-enamel junction to the gingival margin, probing depth (PD) measured from the gingival margin distance to the depth of the gingival sulcus, clinical insertion level (CIL) measured from the distance of the enamel cement junction to the sulcus depth and width of keratinized tissue (KT) measured from the distance of the muco-gingival line to the gingival margin. Location of muco-gingival line was determined visually. Clinical measures were observed immediately before as well as 6 months after surgery at the middle vestibular site of each treated tooth. To this effect, a millimeter Michigan periodontal probe (Hu-Friedy®, Chicago III. USA) was used. All measurements were recorded by one of the authors and were rounded to the lower millimeter. Photographs were taken at treatment initiation, during surgery and at follow-up appointments up to 6 months post-operatively.
Included teeth were four canines and six premolars (upper and lower) giving a total of 12 gingival recessions. Seven gingival recessions were Miller's class I and five were Miller's class II. Six gingival recessions were treated with CAF + SCTG and six with CAF + SCTG + EMD.
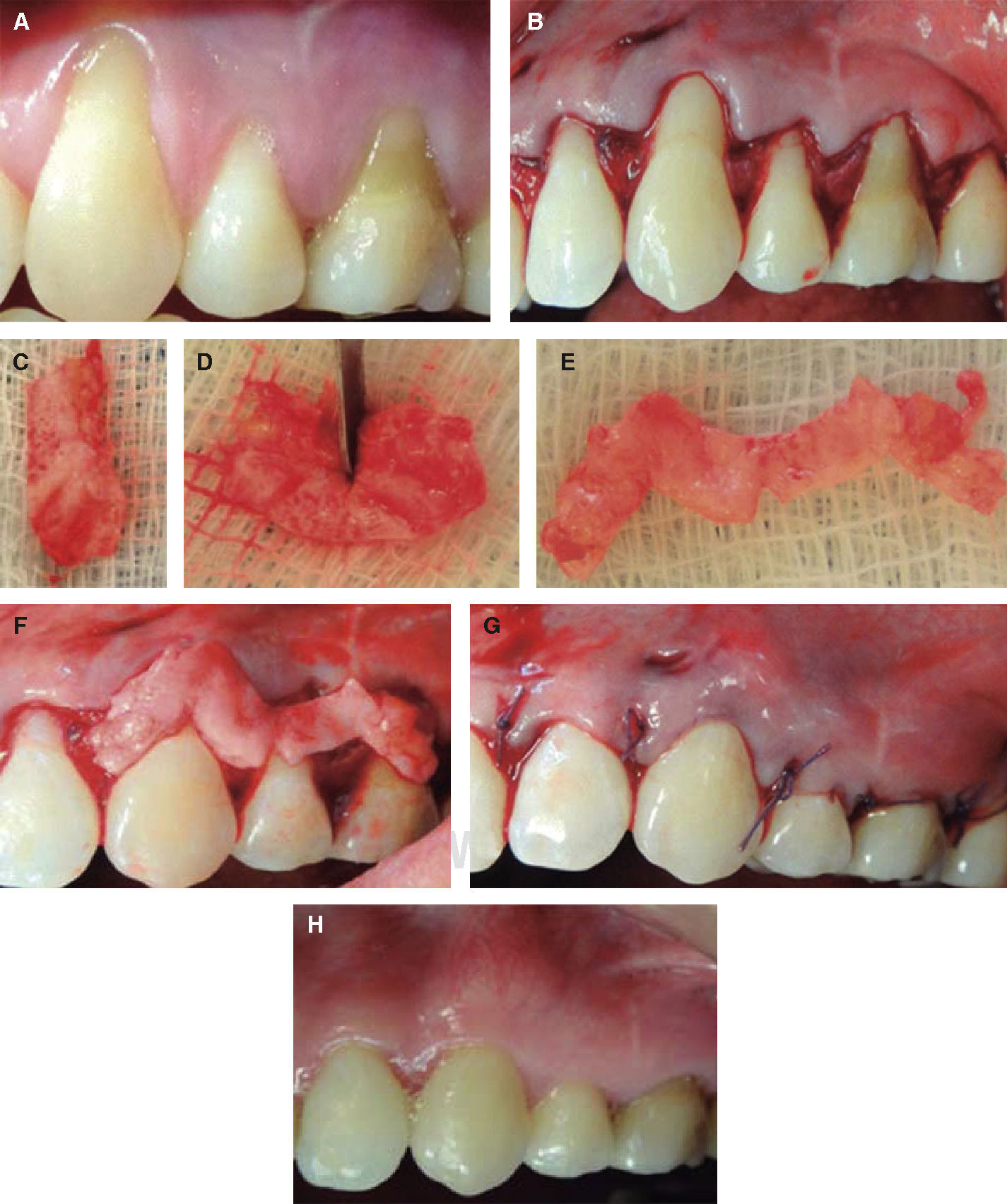
Surgical procedure with CAF + SCTG in upper left and lower right quadrants
After local anesthesia with 2% lidocaine with 1:100,000 epinephrine, root surfaces were scraped and smoothed with Gracey curettes (Hu-Friedy®, Chicago Illinois, USA) in order to remove calculi and plaque deposits, leaving smooth surfaces and removing any protuberance. For surgery the Zucchelli G and De Sanctis M12 bilaminar technique for multiple recessions was used.
Oblique incisions were performed in the interproximal papillae, followed by intra-sulcus incisions around the gingival recessions. A flap of partial-total-partial thickness was lifted in coronal-apical direction. Oblique incisions created surgical papillae which were de-epithelialized. The flap was freed from underlying periostium so as to be able to be freely displaced in a coronal direction towards the level of the cementenamel junction.
The sub-epithelial connective tissue flap was obtained from the palate area, performing the trapdoor incision described by Langer.13 Treatment was initiated with infiltrative blocking with 2% lidocaine anesthetic with epinephrine 1:100,000 at the level of premolars and mesial aspect of first molar. A horizontal incision was performed at approximately 5mm from the gingival margin in apical direction. Two vertical incisions were undertaken at both sides of this horizontal incision. A partial thickness flap was raised thus obtaining sub-epithelial connective tissue. The area was sutured with cross-wise sutures, using absorbable 4-0 suture (PGA® Atramat, Internacional Farmacéutica, Mexico City Mexico).
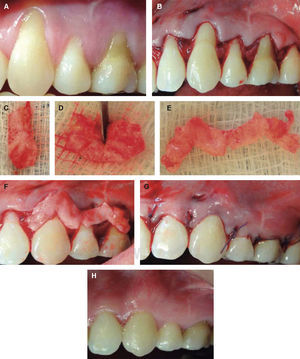
The graft was partially sectioned so as to achieve greater extension and was then placed and adapted to exposed root surfaces. It was fixated to the receptor site with single isolated sutures. After this, the flap was placed in position and sutured at 2mm in a coronal direction from the enamel-cement junction, fully covering the graft. To this effect, 4-0 absorbable sutures were used with horizontal suspensory sutures in all inter-proximal papillae (Figures 2 and 3).
Surgical procedure with CAF + SCTG in left upper quadrant. (A) Gingival recessions before surgery.(B) Oblique incisions beginning from the largest recession. (C), (D) and (E) Graft cut in order to obtain greater extension. (F) Graft placement and adaptation. (G) Sutured, coronally displaced flap. (H) Postoperative results six months after treatment completion.
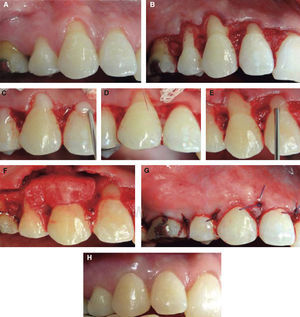
CAF + SCTG in lower right quadrant. (A) Gingival recessions before surgery. (B) Oblique incisions and de-epithelialization of interproximal papillae. (C) Partial-totalpartial thickness fl ap lifting. (D) Flap released from underlying periostium.(E) Palate graft harvesting. (F).Graft placement on root surfaces.(G) Sutured displaced flap. (H) Postoperative results six months after treatment completion.
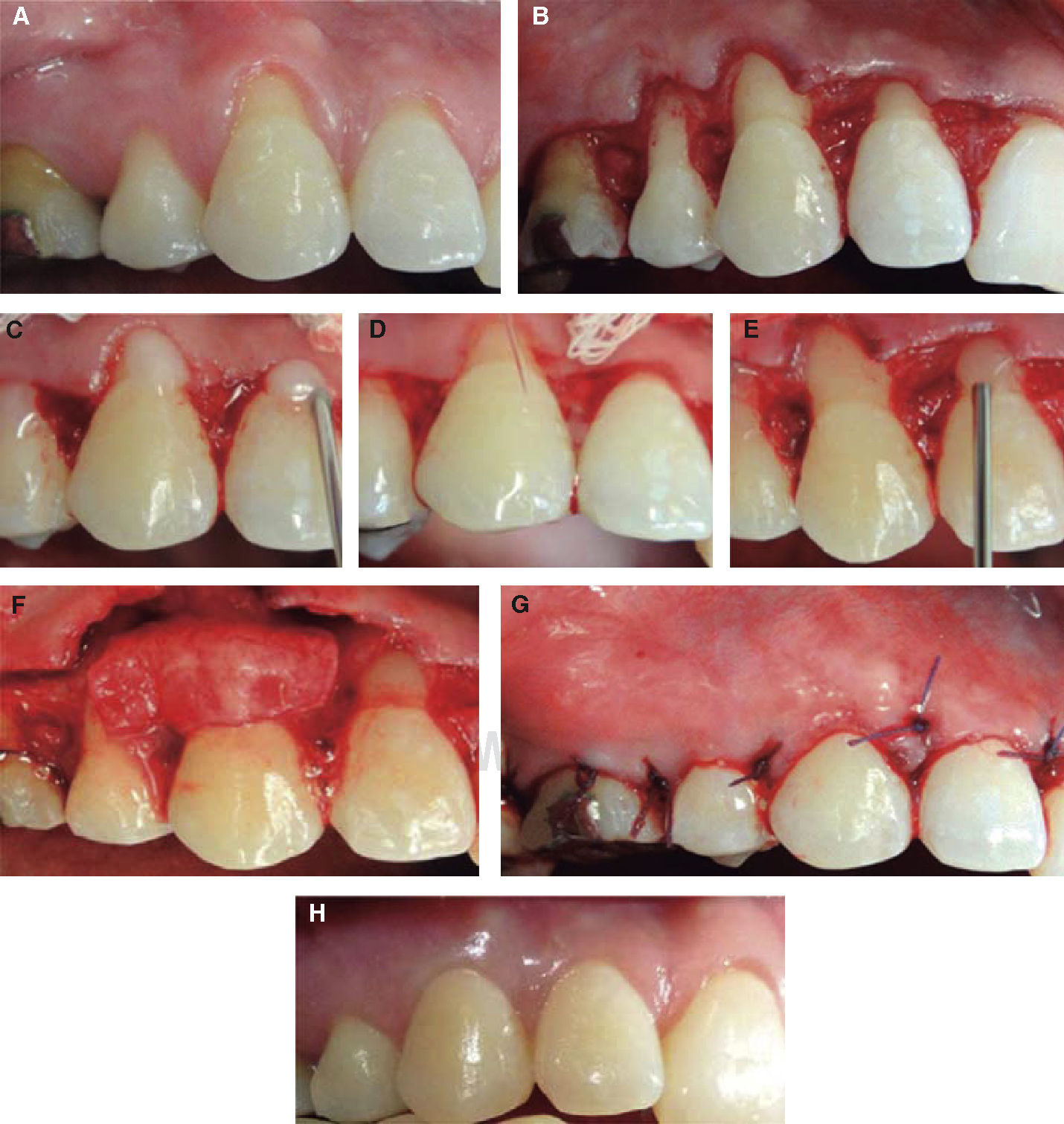
CAF + SCTG + EMD surgical procedure in upper right and lower left quadrants
Sites were treated as previously described with the exception of EMD gel (Emdogain® Straumann, Switzerland) placement, following manufacturer's instructions.
Before placing SCTG, root surfaces were primed for 2minutes with 24% PrefGel® of EDTA (ethylenediaminetetraacetic acid) (Straumann Basel Switzerland). After this time, rinsing abundantly with pressured sterile saline physiological solution, they were lightly dried with sterile gauze. EMD was applied (Emdogain®) on exposed root surfaces, starting at the base of the recession and covering the whole root surface. Immediately after this, the graft was placed on the gel at the level of the cement-enamel junction, and it was stabilized with absorbable 4-0 suture (PGA® Atramat, Internacional Farmacéutica, D.F., Mexico). The flap was coronally displaced l and sutured, using the same 4-0 absorbable suture with horizontal suspensory points at all inter-proximal papillae (Figures 4 and 5).
CAF + SCTG + EMD in upper right quadrant. (A) Gingival recessions before surgery. (B) Flap lifting underneath oblique incisions. (C) Placement of PrefGel on root surfaces. (D) Abundant irrigation with physiological solution to remove PrefGel. (E) Application of EMD on root surfaces. (F) Graft placed immediately after EMD application on root surfaces. (G) Flap sutured above the enamel-cement junction. (H) Healing at six months.
Following surgeries, 600mg ibuprofen (Siegfried Rhein® D.F., Mexico) was prescribed to the patient, every 8hours for four days. The patient was instructed to forego oral hygiene practices on treated zones, as well as use of 0.12% chlorhexidine oral rinse (Siegfried Rhein® D.F., Mexico) twice a day for two weeks. The patient was instructed not to brush the affected area and to avoid trauma and food impaction in the operated area for duration of two weeks. Sutures were removed after 15 days and the patient was instructed to resume brushing and use of dental floss. The patient was examined once a week for six weeks, and after that, every 2 months until 6 months had elapsed. At all appointments, the patient received reinforcement of oral hygiene instructions and was subjected to professional cleansing.
STATISTICAL ANALYSISClinical results were assessed at the beginning of treatment and 6 months after treatment completion. Standard deviation mean was estimated for all four measurements, and these values were compared between both groups at basal measurement and at six months. In all groups, differences in before-after measurements were compared. T student test was used for independent samples, as well as for paired samples as hypothesis proof. p < 0.05 values were considered statistically significant. Results were analyzed through SPSS Software (version 17.0).
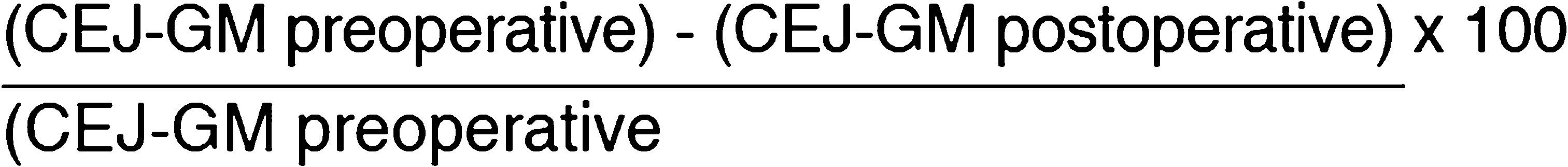
Root coverage percentage was estimated after 6 months according to the following formula:
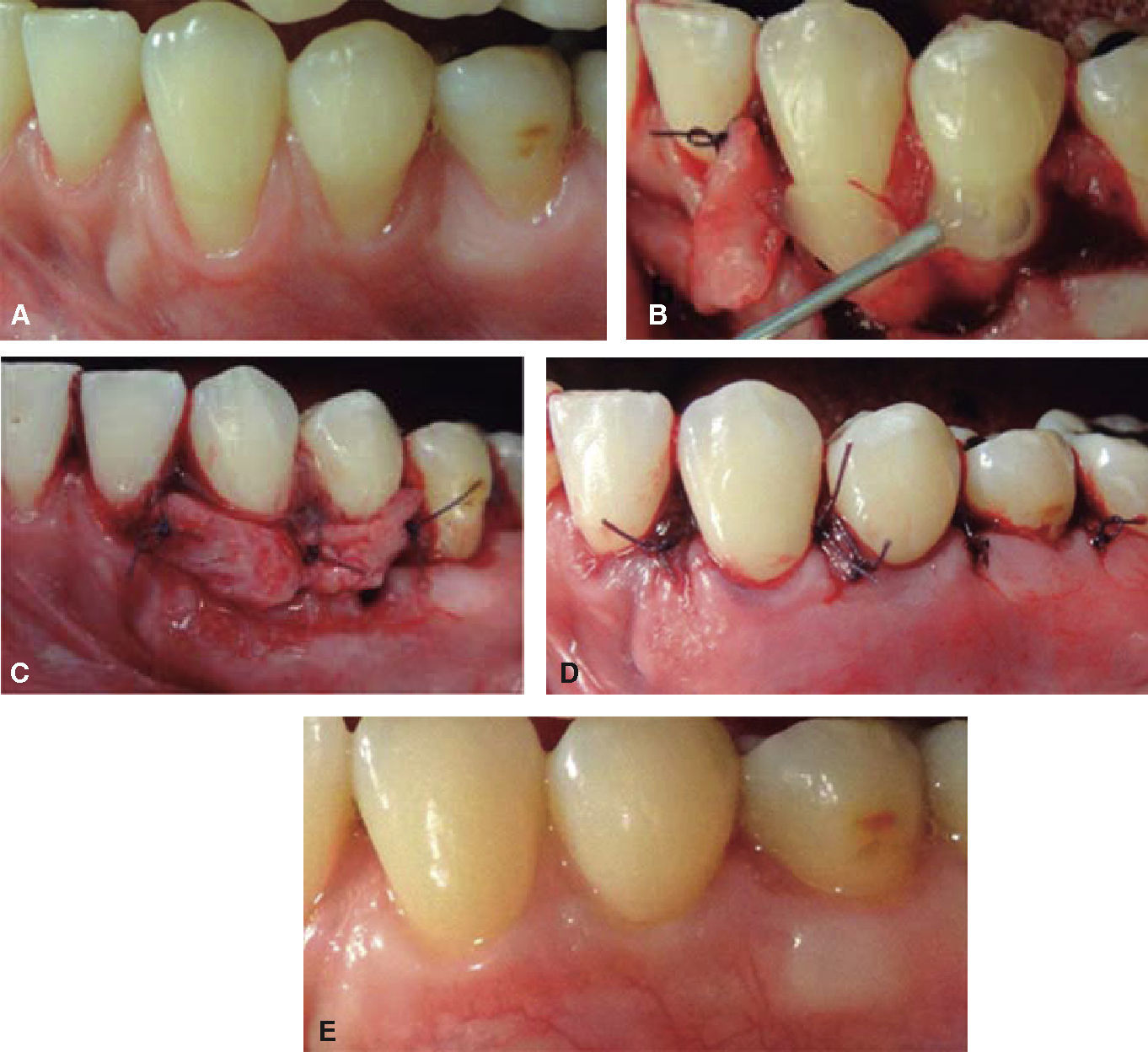
RESULTSAfter six months, all gingival recessions clinically presented soft tissue coverage whose color suitably matched surrounding tissues. None of the surgical procedures caused post-operative complications (Figures 2 to 5).
In all groups, means of measurements were compared at beginning of treatment as well as 6 months after treatment. It was found that both procedures, CAF + SCTG + EMD and CAF + SCTG caused significant root coverage, at an average of 2.83 ± 1.16mm and 2.50 ± 0.83mm respectively. This is to say that the root coverage increase (in millimeters) when comparing measurement at beginning of treatment and six months after completion was statistically significant in both methods. (p = .001 and p = .002).
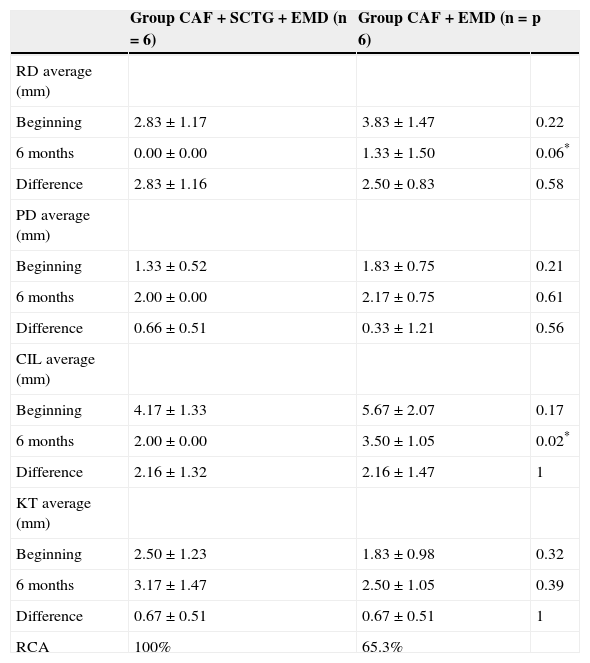
Averages of initial clinical measurements of gingival recession depth (RD), probing depth (PD), clinical insertion level (CIL) and keratinized tissue (KT) among teeth of both treatment groups were similar, since no statistically significant differences were found between both groups (p > .05) (Table I).
Base measurements and measurements at six months and difference between base and six month measurements according to treatment group.
| Group CAF + SCTG + EMD (n = 6) | Group CAF + EMD (n = 6) | p | |
|---|---|---|---|
| RD average (mm) | |||
| Beginning | 2.83 ± 1.17 | 3.83 ± 1.47 | 0.22 |
| 6 months | 0.00 ± 0.00 | 1.33 ± 1.50 | 0.06* |
| Difference | 2.83 ± 1.16 | 2.50 ± 0.83 | 0.58 |
| PD average (mm) | |||
| Beginning | 1.33 ± 0.52 | 1.83 ± 0.75 | 0.21 |
| 6 months | 2.00 ± 0.00 | 2.17 ± 0.75 | 0.61 |
| Difference | 0.66 ± 0.51 | 0.33 ± 1.21 | 0.56 |
| CIL average (mm) | |||
| Beginning | 4.17 ± 1.33 | 5.67 ± 2.07 | 0.17 |
| 6 months | 2.00 ± 0.00 | 3.50 ± 1.05 | 0.02* |
| Difference | 2.16 ± 1.32 | 2.16 ± 1.47 | 1 |
| KT average (mm) | |||
| Beginning | 2.50 ± 1.23 | 1.83 ± 0.98 | 0.32 |
| 6 months | 3.17 ± 1.47 | 2.50 ± 1.05 | 0.39 |
| Difference | 0.67 ± 0.51 | 0.67 ± 0.51 | 1 |
| RCA | 100% | 65.3% |
CAF + SCTG + EMD= coronally advanced flap and sub-epithelial connective tissue graft with enamel matrix derivative, CAF + SCTG = coronally advanced flap and sub-epithelial connective tissue graft, RD = gingival recession depth, PD = probing depth, CIL = clinical insertion level, KT = keratinized tissue, RCA = root coverage average, CRC = complete root coverage.
T Student test for independent and paired samples.
Six months after treatment, a new clinical evaluation was undertaken in order to identify which one of both treatments had achieved better clinical results. It was observed that gingival recessions treated with CAF + SCTG + EMD exhibited average gingival recession depth (RD) of 0.00mm, this is to say 100% coverage was achieved, whereas recessions treated with CAF + SCTG exhibited an average of 1.33 ± 1.50 GR, and achieved 65.3% coverage, these differences were not statistically significant (p = 0.06). Nevertheless, when average clinical insertion level (CIL) was compared, it was found that the group with CAF + SCTG + EMD showed lower insertion average (2.00 ± 0.00) than the CAF + SCTG group (3.50 ± 1.05mm). These differences were statistically significant (p = 0.02) (Table I)
Probing depth averages did not exhibit differences between both groups after 6 months, since the CAF+ SCTG + EMD group exhibited 2.00 ± 0.00mm and the CAF + SCTG group showed 2.17 ± 0.75mm (p = 0.61). No statistically significant differences were found for keratinized tissue between groups, which respectively exhibited 3.17 ± 1.47mm and 2.50 ± 1.05mm (p = 0.39).
Likewise, no statistically significant differences were found when comparing differences among before-after probing depth, clinical insertion level and keratinized tissue measurements in the two groups (p > 0.05).
It was not possible to establish comparisons among class I and II gingival recessions, since their number was not similar in both groups.
DISCUSSIONThe main objectives of surgical procedures for root coverage are the complete coverage and restoration of normal gingival anatomy, achieving thus eradication of root hypersensitivity and restoration of esthetics.
Several techniques have been developed to achieve this goal; predictability has improved as a result of modifications undertaken through the years. It has been shown that the coronally-advanced flap without liberating incisions created by Zucchelli G and De Sanctis M12 conferred abundant blood supply to the sub-epithelial connective tissue graft, improving thus the probabilities to achieve full root coverage in Miller's class I and II gingival recessions.
The thin gingival phenotype present in this patient as well as keratinized tissue absence in apical location with respect to gingival recessions justified the CAF + SCTG procedure, since this procedure is indicated in these biotypes and in canine and premolar areas, with the aim of increasing marginal tissue thickness, avoiding contraction and favoring root coverage stability through time.30
In recent years, periodontal plastic surgery has focused not only on soft tissue coverage, but also on periodontal tissue coverage with the use of EMD; it has shown it can induce growth factor production, which in turn promotes migration of osteoblasts and periodontal ligament cells favoring thus periodontal regeneration in periodontal defects31,32 as well as in gingival recession defects.21,33
The present clinical case compared multiple gingival recessions coverage using the technique of coronally advanced flap with connective tissue graft (CAF + SCTG) with and without application of matrix enamel derivative (EMD). Results revealed that both procedures were effective to reduce gingival recession depth since both techniques produced a high percentage of root coverage (100% in CAF + SCTG + EMD and 65.3% in the group CAF + SCTG).
The group CAF + SCTG + EMD statistically showed better results in the increase of clinical insertion after 6 months, when compared with the CAF + SCTG group. Likewise, it exhibited greater gain of root coverage, which furthermore was found at the limit of significance level (p = 0.06). Nevertheless, when comparing differences, none of both measurements resulted statistically significant. These results concur with those of Rasperini et al26 who established greater rate of root coverage in the CAF + SCTG + EMD group (90%) than that of the CAF + SCTG group (80%), but this did not represent a significant statistical relevance. Other studies have not found additional clinical benefits of including EMD in CAF+SCTG29,34,35 and suggest that, from a clinical point of view, its application is not necessary. Nevertheless, use of EMD could enhance early healing of periodontal tissues as well as new insertion of connective tissue towards the root surface.21 These benefits can only be histologically confirmed.
This study did not prove additional KT gain when EMD was used combined with CAF + SCTG. Similarly, Aroca et al36 study did not report noticeable KT increase after CAF + SCTG + EMD treatment. Nevertheless, other studies24,37 have shown KT gain when EMD was applied with coronal-advanced flap for root coverage. This might suggest presence of an altered expression of keratinocytes stimulated by enamel matrix derivative.
The patient was satisfied with the excellent esthetic results obtained, which were characterized by full root coverage in most gingival recessions and color similarity to surrounding tissues. Nevertheless, one of the disadvantages of this technique was the lengthy treatment time, since complete healing of palate is required in order to once more obtain sub-epithelial connective tissue graft.
CONCLUSIONResults of the present clinical case did not show that EMD use provided additional effect to achieve root coverage, or CIL decrease when a coronally advanced flap and sub-epithelial connective tissue graft were applied as treatment for root coverage in multiple Miller's class I and II recessions; neither did the other two clinical measurements reveal statistically significant differences. Nevertheless, it must be borne in mind that the small size of the sample could have prevented observation of greater differences in both treatments.
Graduate and Research School, National School of Dentistry, National University of Mexico (UNAM).