Battered child syndrome is defined as all forms of violence, prejudice or physical and mental abuse, carelessness or neglect inflicted on the child while under the care of his parents, tutors or any other person exerting physical and/or intellectual superiority. In over 50% of all cases lesions are found in the head and neck area. For that reason, dentists, especially pediatric dentists, must be aware to recognize all sorts of battering or neglect based on a suitably-taken clinical history, and focused exploration when suspicion of battered child syndrome is established.
ObjectiveTo be knowledgeable with BCS intra- and extra-oral indicators which might allow the pediatric dentist to recognize signs and contribute in the diagnosis as part of a multi-disciplinary team in charge of providing care to this type of patients.
Clinical caseA two year, five month old male patient was brought to the National Pediatrics Institute afflicted with peri-orbital edema, multiple limb fractures and oral-facial indicators which suggested battered child syndrome diagnosis.
ConclusionTaking into consideration the frequency with which oral and facial structures are involved in battered child syndrome cases there is a medical, ethical and legal commitment for all dentists and specifically pediatric dentists, to intervene in prevention, detection, diagnosis and treatment of this medical and social problem.
El síndrome de niño maltratado se define como toda forma de violencia, perjuicio o abuso físico o mental, descuido o trato negligente, mientras el niño se encuentra bajo el cuidado de sus padres, de un tutor o de cualquier otra persona en función de su superioridad física y/o intelectual. En más del 50% de los casos las lesiones se presentan en cabeza, cara y cuello. Es por eso que el odontólogo y especialmente el odontopediatra deben estar preparados para reconocer alguna forma de maltrato o negligencia con base en una historia clínica adecuada y una exploración intencionada ante la sospecha de síndrome de niño maltratado.
ObjetivoConocer los indicadores intraorales y extraorales del SNM que le permitan al odontopediatra reconocer los signos y contribuir en el diagnóstico como parte de un equipo multidisciplinario encargado de la atención de estos pacientes.
Caso clínicoPaciente masculino de dos años cinco meses quien acude al Servicio de Urgencias del Instituto Nacional de Pediatría por presentar edema periorbitario, múltiples fracturas en extremidades e indicadores orofaciales que permitieron diagnosticar síndrome de niño maltratado.
ConclusiónConsiderando la frecuencia con que las estructuras orofaciales se ven involucradas en el síndrome de niño maltratado, existe un compromiso médico, ético y legal para que todos los dentistas y específicamente los odontopediatras intervengan en la prevención, detección, diagnóstico y tratamiento de este problema médico social.
The medical and social problem currently named «battered child syndrome» (BCS) is daily gathering more worldwide impact.
In view of this situation and its increasing effect on children's welfare, the World Health Organization (WHO) has considered it a worldwide public health problem.1 It is not easy to clearly define the concept of child abuse. Several national and international organizations have undertaken to define the concept. Nevertheless, based on concepts of the Clínica de Atención Integral al Niño Maltratado (CAINM-INP-UNAM) (Clinic for Battered Child Care), we can define BCS as «Any intentional aggression or omission within or without the home against a minor, before or after birth which might affect his biological-psychological-social integrity, undertaken by a person or institution exerting physical and/or intellectual superiority».2
There is presently sufficient information to state that child abuse has been present since the beginnings of time. It must be understood that this is a phenomenon as old as humanity, and not the distinct characteristic of a modern society. A clear example of this are the words of Aristóteles: «a son or a slave are property, and nothing undertaken with property can be considered unjust». In some civilizations, like in China, breeding was limited to three children, and in order to exert birth control, the fourth child was thrown to wild animals. In France, during the 19th century a habit was developed to hurt and deform children so as to inspire pity and beg for alms. In other parts of Europe, children afflicted with some sort of mental retardation or physical malformation were drowned, since it was believed they were the devil's instruments.3
In Mexico, some pre-Hispanic ethnic groups such as the Mazahuas, sacrificed children and adolescents so as to thank some deity for a given benefit. In some of the Mayan codes, there are specifications for punishments such as infliction of maguey thorns, hair burns when the child lied, long working days or keeping the head of the child in the fumes of dry chili when he was disobedient.4,5
Child abuse recognition dates from 1875, in New York City, when after an abuse case on a 9 year old girl, which shocked all society, the first worldwide law was enacted in order to prevent and chastise child abuse.3
In scientific literature, reports on child abuse identification begin when Caffey, in 1946, described the clinical picture of six children with subdural hematoma and multiple fractures in the long bones, it is interesting to note that three of these children presented oral and facial trauma.6,7 In Mexico, Riojas and Manzano detected the presence of child abuse through radiographic studies.8 It was only in 1981 when Dr Jaime Marcovitch really raised awareness not only of the physicians who treat children, but also the other medical professionals of related areas which are in contact with children.9
Pediatric dentistry, as part of the medical areas, might have had less participation in the problem of child abuse, partly due to lack of interest in the subject, but mainly due to lack of information.6,10 In countries considered first world countries such as USA or United Kingdom, there has always been the concern of describing and documenting child abuse findings in the field of dentistry.
In our country, Monter, de la Teja et al conducted a study on 52 children diagnosed with BSC at the Stomatology Service of the National Institute of Pediatrics (Instituto Nacional de Pediatría). In that study they found that 54% exhibited indicators in the head, face and neck.11 Based on the aforementioned, and considering the frequency of oral and facial structures involved in BCS cases, there is a medical, ethical and legal commitment for all dentists, especially pediatric dentists to intervene in the prevention, detection, diagnosis and treatment of this medical and social problem.6,10,12
Presently it can be determined that a child can be the victim of one or several forms of abuse. Among them we can count sexual and psychological abuse, neglect and physical mistreatment in all possible varieties.13–15
The mouth and all adjacent structures are frequently locations more prone to suffer damage in BCS patients. This is specially due to its psychological meaning, the child speaks, cries and eats through the mouth. Thus, violence is used to silence the child, resulting in clinical indicators of abuse and mistreatment.6,12,16–19
Child mistreatment and neglect cannot be diagnosed when the clinical operator is unaware of the signs and symptoms related to that conduct. Pediatric dentists play an important role raising suspicions on child mistreatment since they could become aware of clinical indicators which might be visible and/or invisible.10,20,21
The American Dental Association, from 1999 onwards, has been stressing the dentists’ ethical responsibility to report any suspicion of abuse or neglect, and it forces them to recognize signs of these entities. Thus, specialists dealing with children must bear the task of acquiring an exhaustive clinical history aimed at finding clinical indicators in those cases when battered child syndrome is suspected.10,22 In our country, there is the Norma Oficial Mexicana (Official Mexican Norm) NOM-190-SSA1-1999. Provision of health services. Criteria for medical care of interfamilial violence. This norm compels all health services providers within the public and private sectors which form the National Health System (Sistema Nacional de Salud) to establish criteria to recognize abuse, provide medical care, promote activities of awareness, updating and training so as to train personnel in charge of providing health services and orientation to users who might be involved in interfamilial violence situations.23
Interrogation as an initial aspect of clinical history, must be focused on becoming aware of abuse's invisible aspects; it is of the utmost importance to enquire about pre-natal and peri-natal background, so as to ascertain whether the child was planned, received timely care for childhood conditions, whether there is familial background of alcoholism or drug addiction, access to basic living facilities, subtly inquiring about familial or spousal dysfunction data, or parental sudden loss of employment, among other factors.15,24,25
Quite frequently, the person responsible of the aggression is the one who first arrives looking for help, either to avoid suspicion or compelled by a sense of guilt. That person can become aggressive during interrogation, or confess that he/she caused some of the injuries but not all of them. Sometimes, the child informs he hit himself, but frequently he tells the story he was ordered to tell, driven either by fear or loyalty to his parents. Therefore, great care must be exerted when analyzing assertions of parents and children.12,26 It has been observed that, when the child is questioned, the parent, in anticipation, provides responses, interrupting thus the communication flow the pediatric dentist is trying to establish with the child.
Clinical inspection is a very important aspect, since pediatric dentists and personnel working alongside them must be perfectly trained to achieve visual impression of children from the moment they enter the office.22,27 Some of these young patients are fearful, they constantly observe their surroundings looking for signs of danger, they do not smile spontaneously and generally, do not establish visual contact. All the following factors must be taken into careful account: lack of hygiene, alterations in gait, small body size with respect to chronological age; typical signs of malnutrition such as forward posture of the shoulders, protuberant abdomen, fragile, thin hair, and pallor of integuments. While examining the child it is possible to observe whether he exhibits difficulties to climb onto the dental chair, or expresses pain when being physically lifted.28–30
Physical exploration must be carefully undertaken; it must be divided into extra-oral and intra-oral analyses. The first analysis initiates in the skull, observation must be made about whether there are hematoma, exostoses, depressions, fractures, areas of alopecia, detachment of the ear lobe, conjunctival hemorrhage, present lacerations and old or healing scars. Lymph nodes and face structures must be palpated, an analysis of the temporomandibular joint must be undertaken so as to find whether there are opening limitations, pain or deviations, and relate all the results with some preceding traumatic background.17–19,24,30
Once the face and head analysis is completed, when there is suspicion of child abuse, it is mandatory to examine other areas such as arms, back, thorax and legs, so as to assess presence of hematoma, scars, burns or any other indicator which might indicate BCS. Ideally, this assessment should be conducted with an assistant present.29,30
Intra-oral examination must be conducted in an orderly manner: soft tissues must be first examined, with emphasis on their integrity, ecchymoses, hematoma, lacerations in the tongue frenulum caused by forced feeding with bottle or cutlery, lacerations in the palate, burns in the mucosa caused by extremely hot food or caustic substances, or inappropriate shape of the tongue.17 After this, assessment of hard tissues (teeth and jaws) might reveal fractures of root and crown, discoloration in some teeth which might indicate former trauma, high incidence of caries, loss of teeth lacking reasonable explanation, asymmetries and fractures of upper or lower jaw, bearing in mind that facial fractures are not very frequent before a child is five years old.6,18,19,30–34
When considering comportment, there must be awareness of the types of behavior exhibited by battered children such as defiance, aggression or depression. When these children manifest their feelings they do so violently, nevertheless, the patient might show himself unpredictable, shy, fearful, with low self-esteem, antisocial, and even in some cases indulging in oral habits such as finger-sucking, bruxism and nail biting.29
No one can decide by himself whether he is facing a case of child abuse. In this sense, only the joint effort of a multi-disciplinary team can detect, treat and intervene; they will provide these children with better assessment and care tailored for each individual case. Based on the aforementioned, the National Pediatrics Institute and the National Autonomous University of Mexico created a Battered Child Comprehensive Care Clinic CAINM (Clínica de Atención Integral al Niño Maltratado). It was created in 1980 by a group of specialists whose inter-disciplinary care was tailored to diagnose, watch over and treat cases of violence against boys, girls and adolescents. Within this multi-disciplinarian team, pediatric dentists play a fundamental role when dealing with suspicion and diagnosis of this condition, since most BCS indicators are located in the areas pertaining to their expertise.
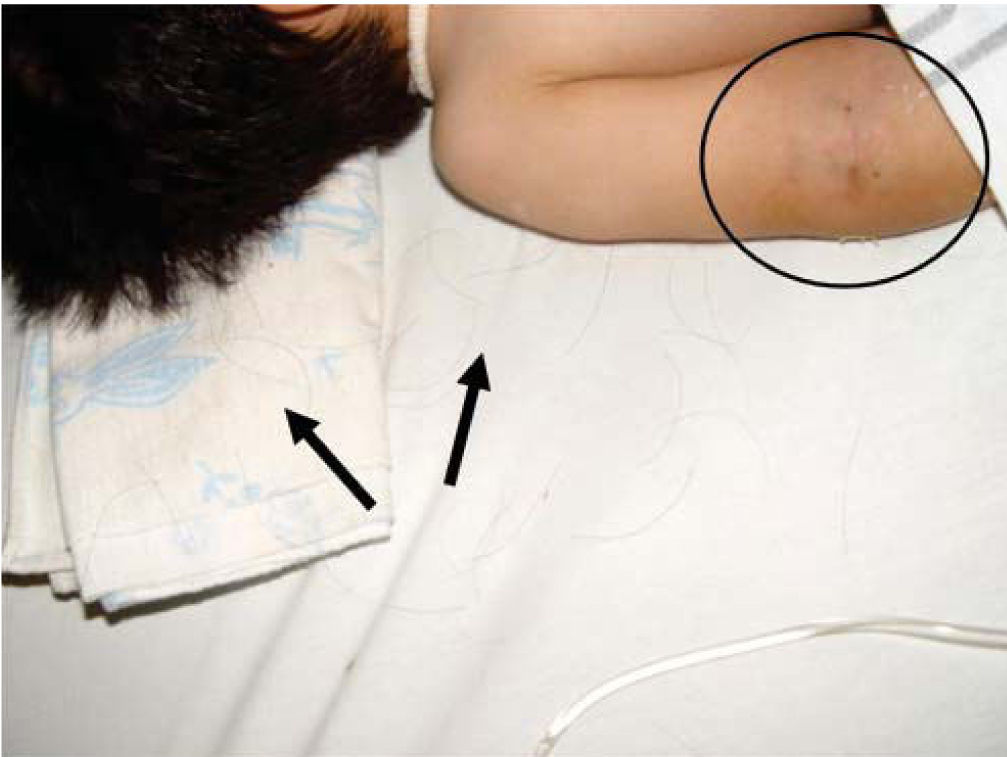
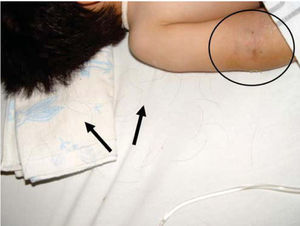
CASE REPORTA two year, five month old patient was brought to the Emergency Services of the National Pediatrics Institute due to the presence of edema in the eyelids, volume increase in the limbs, and decreased limb mobility. Upon admission he was diagnosed with untreated chronic ocular infection and multiple lesions in upper and lower limbs described as follows: left elbow dislocation, fracture of the left radius, double helical fracture of the left tibia, and fracture of the left fifth rib (Figures 1 and 2).
Due to the presence of multiple fractures and to the fact that the mother was unable to logically and objectively explain their provenance, it was decided to consult with the Battered Child Comprehensive Care Clinic (CAINMP-INP-UNAM) to assess whether it was a battered child syndrome case (BCS).
Within the medical team which forms the CAINM, the stomatological service of the same institution was consulted so as to find oral and facial indicators which might support a BCS diagnosis.
Clinical examinationWithin the clinical exploration procedure and as part of the established protocol for approaching patients suspected of being victims of child abuse, the mother was interrogated so as to find out relevant data which might gather indicators to confirm diagnosis.
During interrogation, the mother revealed she was a member of an incomplete family, since she was separated from her partner. She lived and worked in a loaned room in a photographic studio, her schooling was basic and her financial status was of mere subsistence. When asked about the provenance of her child's lesions, the mother denied having hit or hurt him, she continuously expressed ideas that the lesions’ origins were due to «magical witchcraft». She resorted to requiring medical assistance one month after he child's condition, prompted by a witch doctor whom she had visited in order to solve her son's problem.
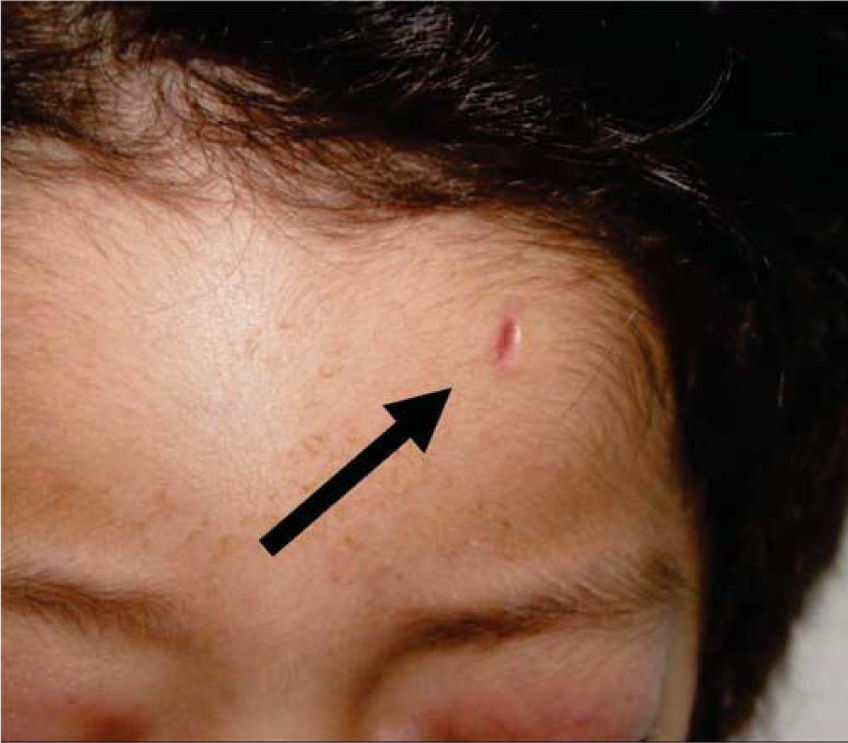
Physical exploration revealed a child in physiological sleep, in supine position, with all four limbs fixated with plaster splints (Figure 3), multiple lesions at different healing stages, such as traces of blows and lacerations in the skin of the right arm (Figure 4). A peri-orbital edema was observed in the head as well as probably traumatic alopecia areas, a scar at the left section of the forehead, the rest of hair was very fragile, which might be related to malnutrition (Figures 5 to 7).
When conducting intraoral exploration, the child expressed pain when requested to open his mouth. Opening was limited, maximum opening only reached 17mm, there was a slight deviation to the right side, therefore, exploration was only carried out with an external lamp, this revealed a full primary dentition, free of caries and localized gingivitis in the anterior area (Figure 8).
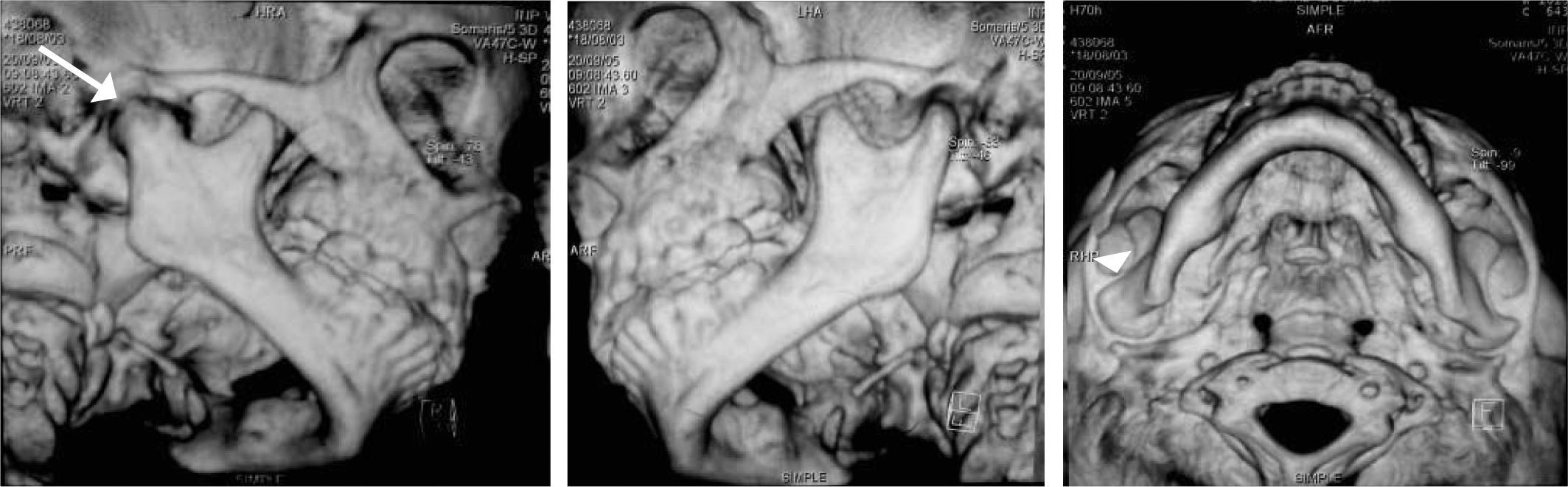
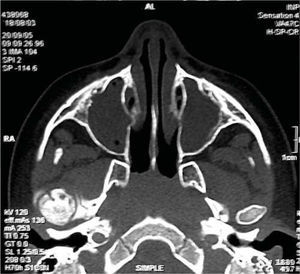
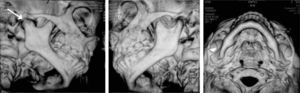
Based on the aforementioned, temporomandibular joint articulation damage was suspected. A computerized axial tomography of the face bulk was requested with axial and coronary cuts as well as TMJ 3-D reconstructions. Tests revealed loss or normal morphology in the right TMJ with decrease of articular space. On the left side normal condyle and coronoid apophyses could be seen, as well as normal morphology and preserved articular space (Figures 9 to 11).
With data obtained from the clinical examination and imaging studies the presence of oral and facial indicators corresponding to battered child syndrome could be confirmed, in its variety of neglect and physical abuse. Moreover a diagnosis of right unilateral bone intra-articular temporomandibular ankylosis secondary to facial trauma was emitted.
Once the diagnosis was established, comprehensive and multi-disciplinary care of the patient was undertaken according to the following prioritization:
- 1.
Treatment of limb fractures undertaken at the orthopedics service.
- 2.
Hospital admittance to treat infectious process of both eyes. Treatment was conducted by the infection control service consisting of a double antibiotic scheme (clindamycin and ceftazidime every 8hours).
It is important to note that patient hospitalization was undertaken for three reasons: a) provide immediate medical care, b) separate the child from the probable aggressor, preventing thus further abuse, c) allow Social Services the time to conduct pertinent research so as to be able to support legal elements of the case.
- 3.
No improvement was observed after drug administration, the ophthalmological service was consulted, and a decision was reached to perform a bilateral enucleation of both eyeballs.
- 4.
Once the patient recovered he was sent to stomatological services to correct ankylosis of right TMJ. Care protocol adhered to by the stomatological service was observed.
The objectives of said protocol were to achieve an ideal maximum oral opening as well as attain satisfactory articulation mobility and function and obtain facial symmetry with harmonious occlusion. This was achieved in the two following phases:
- 1.
Surgical procedure to liberate ankylosis: a simple arthroplasty was undertaken without any need to place a costochondral graft.
- 2.
Functional therapy immediately after arthroplasty.
Patient's surgical treatment was undertaken with a simple arthroplasty with pre-auricular approach (treatment described by Dr Dunn). Existing partial ankylosis was eliminated, allowing thus a 28mm oral opening moments after surgery was completed.
Functional therapyImmediate physiotherapyOnce postoperative pain abated, the patient, with the help of a relative, was asked to conduct opening and closing movements with pliers or a Molt type mouth opener, for 20minutes four or five times a day, in order to cause tension on ligaments and muscles surrounding the articular capsule.
Sugar-free chewing gum was used between exercises. The aforementioned procedures were executed in order to prevent oral opening decrease as well as re-ankylosis.
Mediate physiotherapyMediate physiotherapy was initiated once the acute surgery period was completed. Mental Health Services were consulted to provide psychological care and psychological support due to present abuse circumstances and above all, to motivate the child and his relatives to undertake physical rehabilitation. No oral rehabilitation treatment was required since there was absence of caries. Nevertheless, the responsible adult with custody of the patient (paternal grandmother) was instructed on hygiene preventive care, since mediate rehabilitation consisted in manufacturing and placing a Woodside Bite Spring functional device (Figure 12) during 20minutes, four times a day to stimulate mouth opening and closing favoring thus mandibular rotation and TMJ translation.35
DISCUSSIONBattered child syndrome is considered in our country a public health concern; pediatric dentists are a key element in the diagnosis of this entity. In 1946, Caffey described six cases with multiple fractures; three cases or oral and facial trauma, and two with skin abrasions. Loredo et al,11 in a study involving 29 cases, reported scalp alteration in 79%, forehead 52% and lower jaw 48%. These data corresponded with findings in our present patient. Becker et al (1978) conducted a review of 260 battered child cases of children who had been admitted to the Boston Children's Hospital Medical Center. In that study they found 16% patients with signs of abuse at the head and neck, and 49% of them specifically presented oral and facial trauma.36 In our case, oral and facial indicators were evident as well as the patient's medical requirements which prompted his admittance to a third level hospital to immediately treat neglect and physical abuse sequels.
With respect to the socio-economic characteristics of battered children, Loredo Absala mentioned that, within all the factors that favor BCS phenomenon, financial instability, lack of indispensable basic facilities and familial disintegration are paramount.37 All the aforementioned circumstances were found in the present case, confirming thus the need, to undertake a purposeful interrogation in those cases where child abuse is suspected.
One of the main manifestations of BCS is trauma to the teeth. Malcez described 25 cases and found dental trauma in 32% of them, oral lacerations in 14% and jaw fractures in 11%.6 No dental trauma was observed in our case; there was nonetheless damage in the right TMJ. Taking into account the multiple fractures found in the limbs it can well be considered that deviation and opening limitation experienced by our patient might be a sequel of a previous facial trauma.
Unfortunately, lesions which are the product of physical abuse and neglect can be irreversible, and can even be fatal. Data gathered in the USA point out that fatality averages vary from 48% due to physical abuse and 37% for neglect. In Mexico CAINM reported only 17 fatalities in 17 years.37 In our patient, sequels found after the physical abuse he was subjected to were bilateral enucleation of the eyes as a consequence of the mother's neglect to treat chronic infection as well as oral opening limitation as a consequence of ankylosis of the right temporomandibular articulation.
In our country there have been no reports on TMJ ankylosis as a sequel of physical abuse in patients diagnosed with battered child syndrome. Most cases are focused on ankylosis treatment, and make no reference to physical abuse.
With respect to temporomandibular ankylosis post-surgical functional therapy, Kimura38 reported 52 cases surgically treated for TMJ ankylosis in three IMSS (Mexican Institute for Social Security) hospitals; he concurred with the use of physiotherapy and functional devices (appliances) to avoid reankylosis.37 Kaban,39 Behnia40 and other authors recommend vigorous physiotherapy and devices to activate oral opening. Munro41 and Morey42 mention that early physiotherapy is essential and can be initiated immediately after surgery. They considered that when early physiotherapy is initiated and the space between the base of the skull and the lower jaw is between 1.5 and 3cm, it could be possible to avoid placing condylar reconstruction materials. In our case, it was possible to perform a simple arthroplasty, without having to place grafts in order to reconstruct the condyle; immediate post-surgical physiotherapy was conducted and elicited favorable results.
CONCLUSIONSAwareness of child abuse requires knowledge of visible and invisible extra-oral and intra-oral indicators which might contribute to diagnose BCS.
In the field of pediatric dentistry, a focused and comprehensive clinical history must be taken, which might allow the dentist to become familiar with the child's environment. A thorough extra-oral examination must be conducted so as to identify alopecia areas, hematoma, scars at different healing stages as well as limitation in the function of limbs and/or articulations.
Likewise, the temporomandibular joint must be assessed, as part of the stomatognathic system, with the aim of identifying opening and closure alterations which might indicate a probable fracture or ankylosis at the joint.
Second year Resident, Pediatric Stomatology Specialty.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam