Children rarely experience tumors in the face. Nevertheless, tissue damage caused by these tumors can modify facial growth and development causing physical, esthetic and psychological alterations. The histopathologiical origin of these lesions is variable, but their local behavior is frequently aggressive, oftentimes not matching their “benign” histological appearance. In order to reach accurate diagnosis it is important to be familiar with radiographic and clinical characteristics exhibited by all lesions, adequately take a biopsy, as well as count with histopathological operators with experience in the recognition of these tumors, since they ultimately are responsible for the treatment to be prescribed. Lesion resection is the treatment's objective, to restore facial esthetics and function, and, whenever possible, favor growth of any affected anatomical structures. This is not easy to achieve in government hospitals with limited resources. There is yet a lot to be achieved in the field of favoring bone growth and later rehabilitate patient's occlusal conditions. In the present article we present four cases of tumors in pediatric patients. Tumors were of different histopathological lineage and low frequency, but all were locally aggressive. These tumors were treated at the Hospital de Alta Especialidad 134, Mexican Institute of Social Security, Torreon, Coahuila, Mexico.
Los tumores de la región facial en niños son poco frecuentes pero el daño que ocasionan en los tejidos modifica el desarrollo y crecimiento de la cara, ocasionando alteraciones físicas, estéticas y psicológicas. El origen histopatológico de las lesiones es variable, pero la conducta local de las mismas suele ser agresiva, no correspondiendo en muchas ocasiones a su «benigna» apariencia histológica. Para llegar a un diagnóstico correcto es importante conocer características clínicas y de imagen que presenta cada lesión, realizar una adecuada toma de biopsia, además de contar con histopatólogos de experiencia en el reconocimiento de estos tumores, ya que de ello depende el correcto tratamiento a realizar. El objetivo del tratamiento es la resección de la lesión, restaurando función y estética facial y, de ser posible, favorecer el crecimiento de las estructuras anatómicas afectadas, siendo esto último difícil de llevar a cabo en hospitales del sector salud de presupuesto limitado, habiendo mucho por hacer en lo que se refiere a los tratamientos encaminados a favorecer el crecimiento óseo y posterior rehabilitación de las condiciones oclusales de los pacientes. En este artículo reportamos cuatro casos de tumores en pacientes pediátricos, de diferente estirpe histopatológica y de poca frecuencia, pero con la misma agresividad local, tratados en el Hospital de Alta Especialidad 134, del Instituto Mexicano del Seguro Social, Torreón, Coahuila, México.
Primary maxillofacial tumors in pediatric patients are very rare when compared to tumors present in adults. Nevertheless, tissue damage caused by these lesions is of greater impact, since, in children, they directly alter facial growth and development as well as psycho-social evolution.1 Generally, tumor lesions in children exhibit aggressive local behavior; initial diagnosis and ensuing treatment plan are difficult, since tumor malignity degree and histological lineage must be established. Treatment must be geared to lesion resection and immediate tissue reconstruction, in all possible cases restoring function and esthetics in one single procedure as well as favoring growth of affected structures.2 All the aforementioned procedures are possible when lesions are benign but are difficult to achieve when lesions are malignant, since they will require oncologic treatment and frequently will lead to the patient's demise. In all cases it is difficult to establish an initial diagnosis, since signs and symptoms as well as radiographic findings are sometimes similar or unspecific for each lesion. Histological origin or malignancy degree are prone to confusions, therefore, harvesting the biopsy is the most important element to achieve accurate diagnosis.3 It is recommended to count with experienced pathologists, well able to recognize tumors in the facial region, since accurate diagnosis will lead to an appropriate surgical behavior.
In children, primary tumor lesions are normally more aggressive and exhibit high levels of recurrence. This is due to the growth potential of developing cells, characteristic of these ages. Therefore wide resection with lesion-free margins are of utmost importance.4 Practically all basic tissues of the body can develop tumor lesions, nevertheless, the upper and lower jaw possess a unique characteristic, that is to say, they have teeth included. Therefore, lesions can be found in these structures which cannot be found in any other anatomical area of the body. These aforementioned lesions are generally known as odontogenic tumors5 Initial assessment of children afflicted with tumor lesions must per force include clinical history and physical exploration. All the following factors must be carefully taken into account: age, gender, familial genetic history, lesion onset, evolution and present state, present signs and symptoms, clinical data such as pain, paresthesia, paralysis, lesion discoloration, lesion bleeding, time of growth and degree of destruction or invasion to adjacent anatomical structures, mobility or fixation of the lesion, consistency, contents and size of tumor. All the aforementioned factors are meaningful diagnostic data. Other important signs and symptoms that might lead us to consider a possible malignant lesion are considerable weight loss, asthenia, adynamia, high temperature, or tegument pallor. It is important to take into account diagnostic auxiliary tools such as laboratory exams, X-rays computed or three-D tomograms, magnetic resonance or even ultrasound, all these tools are basic to guide diagnosis.6 Even though these studies are not conclusive to undertake a diagnosis, they will indicate with great precision whether the lesion has its origins in soft or hard tissues, its size, whether it contains solid, liquid or mixed material, whether or not it is encapsulated, as well as the amount of destruction to adjacent structures, relationship of tumor to relevant nerve, vascular or anatomical structures. Primary-origin tumors in children frequently exhibit rapid local growth, with local invasion and tissue destruction, which oftentimes do not match their benign histological appearance. In spite of this rapid and destructive behavior, lesions in children are normally benign, nevertheless, treatment must be based on their biological and clinical behavior which is normally aggressive.7 Early detection of these lesions would be of the utmost importance to avoid severe complications derived from radical surgical treatments.
MATERIALS AND METHODSFour cases of pediatric patients were reviewed in the present article. These patients exhibited locally aggressive primary tumors; tumors were of different histological lineage and malignancy degree. In view of exhibited aggressiveness, tumor surgical treatment was based on biological and clinical behavior rather than on tumor histopathology Patients were treated at the Unidad de Alta Especialidad Num. 134 (Highly Specialized Unit) (UMAE) of the Mexican Institute of Social Security (IMSS), Torreon, Coahuila, Mexico.
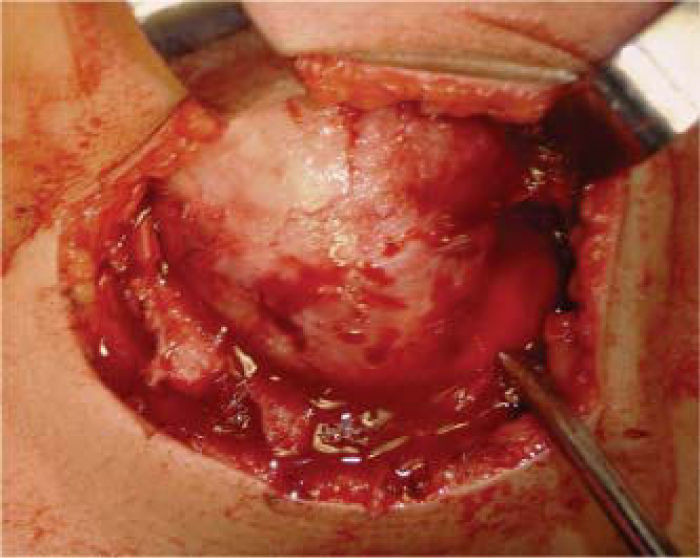
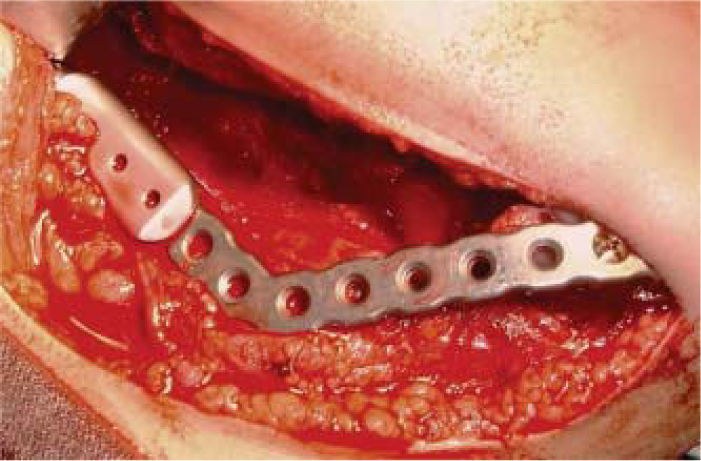
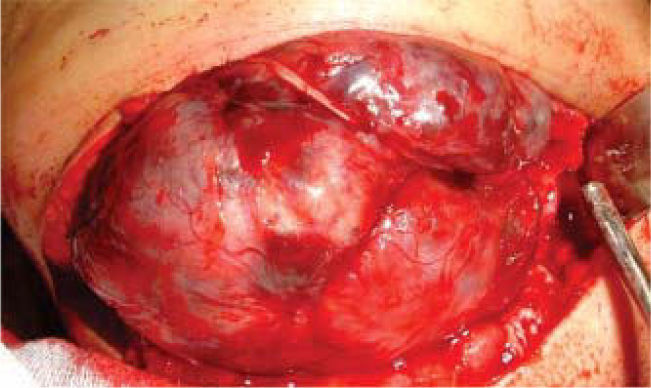
Case 1Six year old female patient exhibiting volume increase at the right side of the mandible. Lesion was of a four month evolution. Lesion was of rapid growth and elicited mild pain (Figure 1). Intraorally, expansion of mandibular cortical bone at molar level could be observed. Three-D tomogram confirmed widespread bone destruction (Figure 2). Patient's general health had not been compromised with absence of general signs and symptoms. Laboratory results were within normal parameters. Incisional biopsy report revealed benign mandibular osteoblastoma. In view of lesion's widespread destruction and aggressive local behavior, a right hemi-mandibulectomy was performed (Figure 3). A mandibular reconstruction prosthesis with condyle was placed on the surgical bed (Figure 4). Post operative control showed suitable oral opening, with undamaged main nerve structures, motor and sensory nerves preserved their continuity (Figure 5).
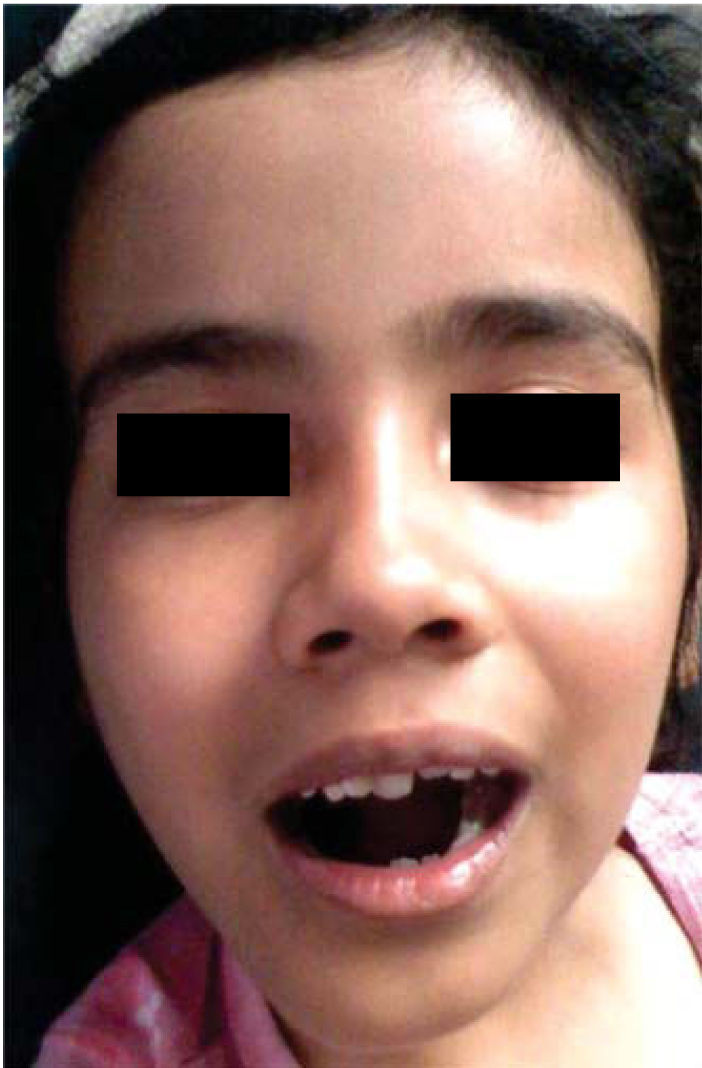
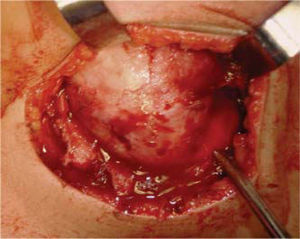
Case 2Eight year old female patient who attended the clinic with increase in left hemi-mandibular volume. Lesion was of a 5 month evolution with fast, painful growth (Figure 6). Intra-orally, expansion of vestibular cortical bone was observed, with tooth displacement (Figure 7). X-rays revealed a lesion destroying part of the body and ramus on the left side of the mandible, nevertheless, condyle and coronoid apophyses were preserved (Figure 8). The patient did not exhibit any other relevant data; laboratory exams yielded normal parameters. Result of incision biopsy was mandibular plexiform ameloblastoma. Block excision was undertaken in view of the lesion's local aggressive behavior (Figure 9). A reconstruction prosthesis was placed with preservation of condyle and coronoid apophyses (Figure 10). No complications were observed during post-operative period; motor and nerve structures were preserved. The patient exhibited suitable oral opening and appropriate facial appearance (Figure 11).
A 13 year old female patient sought consultation due to a lesion in the right mandibular alveolar process. The lesion was of a three month evolution, painful and of rapid growth, with mild paresthesia in the right lower lip. The lesion exhibited a granular and bloody appearance, with sessile base (Figure 12), X-rays revealed a diffuse, radio-lucid area, at the level of right lower premolars. No other relevant pathological data were observed. Biopsy outcome yielded result of mandibular ameloblastic fibroma. A block resection of the lesion was undertaken with lower ridge preservation (Figure 13).
Case 4Radio-lucid lesion in the ramus and upper body of the right side of the mandible involving condyle and coronary apophyses (Figure 14) in a nine year old male patient. He complained of mild pain in lower right molars, no other relevant data were noted. Biopsy yielded results of mandibular ameloblastoma. Lesion extension dictated performance of right hemimandibulectomy with placement of reconstruction prosthesis including a condyle. X rays taken two years after surgery revealed spontaneous hemi-mandibular bone regeneration, with bone adopting the shape of the mandibular ramus and following the contour of the titanium metallic plate shows physical appearance two years after surgery (Figures 15 and 16).
In certain primary tumors found in children, lesion's histopathological results oftentimes do not match the tumor's aggressive biological behavior. Therefore, treatment must be determined through tumor location, extension and biological behavior.8 Histopathologically, benign lesions oftentimes exhibit locally aggressive behavior, and lesions with benign clinical appearance are usually malignant. Our first case was a mandibular osteoblastoma. Osteoblastomas are infrequent primary bone lesions located in the maxillofacial area. These lesions are most frequently found in long bones and spine, approximately 15% can be found in facial bones,9 most commonly in the mandibular bone.10 Patients are commonly asymptomatic or they can experience pain in the lesion area which does not subside with salicylate use. These lesions can appear at a wide age range, nevertheless they are most frequent in young patients in the 20-40 year old range. Some recent articles refer lesion prediction for the female gender.11 Many pathologists find it difficult to differentiate osteblastoma from other similar pathological entities such as osteoid osteoma, cementoblastoma, juvenile ossifying fibroma and osteosarcoma: this is due to the fact that they present some similar histological characteristics. Jones et al12 proposed that any lesion located in the maxillofacial skeleton and composed of osteoblasts with osteoid formation and trabecular bone in a well vascularized connective tissue stroma must be called osteoblastoma. Some osteoblastoma have a tendency to recur, malignant transformation from osteoblastoma to osteosarcoma have additionally been reported.13 Cases two and four illustrate ameloblatoma in an 8 year old girl and a 9 year old boy respectively. Ameloblastomas, are odontogenic-origin neoplasias derived from embryonic remnants of the enamel which persist in the upper jaw. Triggering factors for the onset of these tumors are yet unknown, they are histopathologically benign neoplasia, nevertheless exhibiting aggressive recurrent behavior without a circumscribing capsule. They appear mainly in the upper jaw, especially in the molar zone and ascending ramus. They usually exhibit asymptomatic beginnings, they grow and expand bony plates causing lesions to adjacent teeth and bony tissue loss.14 This lesion is more common in adults, and is rarely found in children under 10 years of age.15 Case three reports a mandibular ameloblastic fibroma in a 13 year old female patient. Ameloblastic fibroma is a rare, mixed, benign odontogenic tumor representing 1.5 to 4.5% of all odontogenic tumors.16 In most cases this lesion occurs in the posterior region of the mandible mainly in the molar and premolar areas. Average onset age is between 14 and 15 years. These tumors are normally asymptomatic at the beginning, exhibiting a slow volume increase. Radiographically, they appear as multior uni-locular radio-lucid areas, presenting sclerotic margins. Treatment of the aforementioned lesions can vary from radical excision to block resection, segment resection or enucleation and curettage.17
In these lesions, treatment of choice should be extensive resections, and whenever possible, early reconstruction of the damaged area,18 trying, whenever possible, to preserve nerve, sensory and motor structures. In three out of the four presented cases lower dental nerve continuity was preserved, and in one of them spontaneous mandibular bone formation could be observed,following the contour of the reconstructive titanium plate; titanium is a material that somewhat favors this type of reactions and is therefore recommended for this type of procedures instead of using chrome-cobalt plate. Severe loss of mandibular bone tissue was observed in cases 1 and 2. Patients’ relatives did not accept harvesting and placing of iliac crest graft to reconstruct damaged area. In this sense, it would be relevant to note that this decision was made in view of the impossibility of patients to continue with rehabilitation after bone graft procedure; this rehabilitation would involve implant placement in the area of the graft, therefore, partial reconstruction was decided upon. Most government hospitals in Mexico lack implant placement services, therefore, in these cases, reconstruction can only be partial. It is difficult for patients to avail themselves to these possibilities due to the high cost they represent when treated in private practice. There is much to be still furthered in the rehabilitation, not only physical but also physiological, of these patients. With respect to physical rehabilitation, availability to new advances such as bone regeneration with morpho-genetic protein-type bone inductors should be considered in order to avoid morbidity caused by all tumor harvesting and placing procedures.19 After surgical treatment is completed, the need for psycho-social therapy must be considered, since for the patient, to lose part of their anatomy, the face being the most affected, causes significant psychological damage.
CONCLUSIONSIn general terms, it can be said that benign and malignant tumor lesions in children are not very frequent, they exhibit greater frequency in adult population. For the aforementioned reason, when these lesions appear in children, they represent cases of greater scientific interest as well as an important challenge to establish diagnosis and treatment plan. Since these are aggressive lesions, surgical treatment is frequently radical, with all its inherent consequences; for this reason, in these cases, establishment of accurate diagnosis is clearly required before undertaking any treatment. To be able to emit said diagnosis, all clinical and radiographic characteristics of the tumor must be ascertained; experienced pathologists with wide experience in the maxillofacial area are equally required. Clinical behavior of these tumors can be variable and frequently does not match histological pattern.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam