It is known that pain is the most disturbing symptom-syndrome in patients in any context of medical therapy, so the comprehensive critical care (biological–psychological–social–spiritual) approach should be adequately addressed in the patient–family–healthcare team triad when structuring major therapeutic care. Health status, as well as admission to the High Dependency Unit and/or Intensive Care Unit represents an event often accompanied by dependency, uncertainty, fear, multiple losses, vulnerability, suffering and near-death experiences. Patients in intensive care often experience multiple and recurrent acute stressors, where their response and ability to cope depend on a variety of neuropsychological, cognitive, emotional, and social functions and the support that is given to them in these areas.
Se sabe que el dolor es el síntoma-síndrome más preocupante en los pacientes en cualquier contexto de terapéutica médica, por lo que en medicina crítica el abordaje integral (biológico–psicológico–social–espiritual) debe ser adecuadamente abordado en la tríada paciente-familia-equipo de salud (ES) al ser los principales estructurantes de la atención terapéutica. El estado de salud, así como el ingreso a la Unidad de Terapia Intermedia (UTI) y/o a la Unidad Cuidados Intensivos (UCI) representa un evento acompañado frecuentemente de dependencia, incertidumbre, temor, múltiples pérdidas, vulnerabilidad, sufrimiento y experiencias cercanas a la muerte. Los pacientes en cuidados intensivos experimentan a menudo múltiples y recurrentes factores de estrés agudo, donde la respuesta y afrontamiento depende de una variedad de funciones neurofisiológicas, cognitivas, emocionales, sociales y el apoyo que se les brinde en estos aspectos.
The concept of a critically ill patient is not clear since it is often used a synonym for urgent or emergency patients. Urgent patients are defined as patients who have problems of diverse aetiology and varying severity that create awareness of an immediate need for care in the subject or their close friends or relatives. Its course is usually slow and not necessarily life-threatening, but care should not be delayed by more than 6h. Emergency patients are all subjects in whom their life or the function of an organ is in danger. In this case a lack of healthcare will likely lead to death within minutes and it is essential to apply first aid. In these patients, the concept of the golden hour is promoted as the first hour after an event in which mortality is elevated due to the high onset frequency of complications.
Therefore, to prevent confusion, we will define patients as critically ill when, regardless of their baseline status as urgent or emergency patients, multiple organ failure or the failure of sequential vital signs begins with an imminent danger of death creating a persistent state of severity that requires continuous monitoring and treatment.1
This definition includes, but is not limited to, patients found in intensive care and/or high dependency units since there are critically ill patients with practically no possibility of recovery and who because of triage priorities are located outside these units.
The International Association for the Study of Pain (IASP) defines “pain” as an “unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”.2 This “symptom” is important to always keep in mind since pain can become an illness if it is not adequately treated on time.3 As it is a frequent and unpleasant symptom in critically ill patients it is considered a risk factor for several psychological and physiological complications, some of which are potentially fatal.
Nearly five million patients are admitted to the ICU each year. More than 70% of the patients in ICUs have pain, of which 63% have moderate to severe pain. It is also known that only half of the patients with sedation receive analgesics and 21% of those who have muscle relaxants do not receive analgesics. Forty percent of cases with acute respiratory failure, multiple organ failure, and sepsis who end up dying reported pain in the last 3 days of their life.4
Pain is one of the most common symptoms in patients in critical condition and it is experienced by every patient in a unique way. Procedures that cause pain, such as movement and tracheal aspiration, are common and trigger acute pain.5 Furthermore, many of these patients have a history of chronic pain, which complicates their course and treatment.6
According to the international guidelines from the IASP, medical, surgical, and trauma patients in the ICU routinely present pain at rest, during care routines, and during procedures. In addition, pain in adult patients after heart surgery is common and poorly treated.7
Given the importance of an adequate approach to and treatment for pain, the interdependent actors in the comprehensive care plan for critically ill patients, both the family and the healthcare team, must be considered with the goal of achieving a good outcome in the psychosocial domain that, according to Garland,8 is measured based on long-term function and the perception of quality of life among survivors, patient- and family-satisfaction, agreement between desired and actual end-of-life decisions, and the pertinence of the provided medical interventions.
In the healthcare team, all the staff involved to participate in psychosocial and spiritual care. Therefore it is important to understand the processes that take place in the context of critically ill patients, how to assess emotional, cognitive, and behavioural symptoms, as well as how to apply diagnostic and intervention methods based on the scientific literature.
The complete situation for critically ill patients is enormously complex. The health condition, as well as admission to the High Dependency Unit (HDU) and/or the Intensive Care Unit (ICU) represent a high-impact event where patients frequently confront a technologically driven environment, high noise levels, painful procedures, fear, loss of autonomy, vulnerability, suffering, and near-death experiences.9 Therefore, patients in intensive care often experience multiple and recurrent acute stressors where their response and ability to cope depend on a variety of cognitive and neurophysiological functions,10 as well as the degree of emotional and social support they receive.11
In this context, patients can be reduced to their illness, identified by room number, promoting a feeling of isolation, loneliness, loss of control, and uselessness. For these reasons, it is important that patients feel as if they have a name and are treated like a person with inherent dignity and worth.
Pathophysiology of painPain is definided as a dynamic process, where the central brain centres responsible for cognition and emotion influence the transmission of nociceptive signals from the specific receptor sites of pain in the brain whith the influence of immunological and endocrine mechanisms that are modified by stress during the pain process. These proposals suggest taking any emotionally stressful situation into account.12
The pathophysiology of pain is complex, but in general it starts with the release of inflammatory mediators after tissue injury. The mediators stimulate the nociceptors, which transmit pain impulses to the dorsal horn in the spinal cord. The pain impulses reach the somatosensory cortex, where the site and meaning of the pain are produced.13
The physiological response to pain is nearly universally adverse, causing a potentially fatal unstable haemodynamic state,14 endocrine abnormalities that cause an increase in the release of catabolic hormones such as cortisol and glucagon as well as a decrease in anabolic hormones. This causes anxiety, which increases the needs for O2 and triggers a stress response, activating the sympathetic nervous system which translates to tachycardia, an increase in myocardial oxygen consumption, and an increase in catabolism. This contributes to pulmonary dysfunction by protecting the muscles around the area of pain, causing generalised muscle rigidity or spasms that restrict movement of the chest wall and diaphragm.15
The increase in circulating catecholamines can cause artery vasoconstriction, worsen tissue perfusion, and reduce the partial oxygen pressure in tissue.16
Other responses caused by pain include catabolic hypermetabolism that causes hyperglycaemia, lipolysis, and muscle breakdown to provide protein substrates,17 suppression of natural killer cell activity18—a critical function in the immune system—decrease in the number of cytotoxic T cells, and a reduction in neutrophil phagocytic activity.19
Acute pain can be the major risk factor for developing delirium and persistent pain is often neuropathic.20 Moreover, if it remains unalleviated it tends to be ubiquitous and non-benign, with both short- and long-term consequences.
Changes in cardiac output, blood flow, blood and tissue pH, and hypoalbuminaemia are the most important factors regulating changes in the response to the administered analgesics and sedatives.
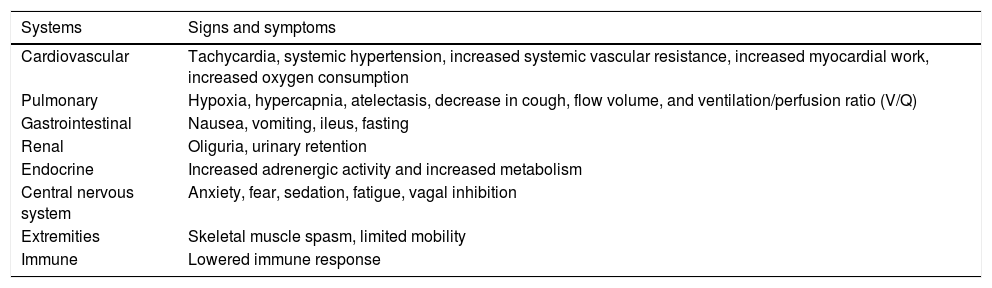
The most common physiological changes are discussed in Table 1.
Pathophysiological consequences of acute pain.
| Systems | Signs and symptoms |
|---|---|
| Cardiovascular | Tachycardia, systemic hypertension, increased systemic vascular resistance, increased myocardial work, increased oxygen consumption |
| Pulmonary | Hypoxia, hypercapnia, atelectasis, decrease in cough, flow volume, and ventilation/perfusion ratio (V/Q) |
| Gastrointestinal | Nausea, vomiting, ileus, fasting |
| Renal | Oliguria, urinary retention |
| Endocrine | Increased adrenergic activity and increased metabolism |
| Central nervous system | Anxiety, fear, sedation, fatigue, vagal inhibition |
| Extremities | Skeletal muscle spasm, limited mobility |
| Immune | Lowered immune response |
If pain is not effectively detected or alleviated, the patient's recovery can be delayed by presenting physiological, psychological, and behavioural alterations.21 Moreover, it hinders patients from properly collaborating their rehabilitation (movement or respiratory physiotherapy), which can lead to complications that extend their hospital stay and increase health costs.22
PsychopathologyPsychological stress factors show similar neuro-hormone and secretagogue patterns to those described with physiological stress factors.23 Stress and negative emotions in critically ill patients can present immediately, in the short- to mid-term, as well as in the long-term, impacting their psychological and physical well-being.24 This has been related with delays in physical recovery, prolonged hospital stays, and being a factor that influences delirium-related psychotic symptoms.25
The main mental alterations that can present in critically ill patients are those related to: stress, depression, anxiety, trauma, delirium, and other neuropsychiatric alterations, all of which will influence their perception of pain and significantly alter their experience.
Depression and anxiety are associated with cognitive errors that influence their ability to make decisions and negatively affect their prognosis. The response to the excessive amount of anxiety can present as agoraphobia, panic attacks, and hospital phobia, to mention a few.
Delirium is an important neuropsychiatric syndrome since it can be confused with the above-mentioned alterations. Svenningsen considers it an “underestimated condition, especially in critically ill patients”, and its presence increases the risk of mortality by 10% in the first year after discharge. There is also a correlation between the duration of delirium in the ICU and cognitive deterioration. A wide range of factors contribute to its development: anaemia hypoalbuminaemia, blood transfusions, genetic predisposition, systemic inflammation, high or fluctuating glucose levels, drugs, dementia, physical restrictions, age, and severe disease.26
Post-traumatic stress disorder refers to a specific set of symptoms that persist for more than 1 month after exposure to a stress factor and is characterised by frequent, vivid flashbacks, avoidance of stimuli associated with the flashback, hyperexcitation, and deteriorated social performance.27 It can become highly disabling, preventing the patients from returning to their normal lives since they avoid doing activities that trigger exacerbations in their symptoms and can directly influence adherence to the therapeutic treatment.28 The risk for post-traumatic stress disorder has been associated with prior psychopathology, high doses of benzodiazepine, and memories of fighting and/or psychotic experiences during the ICU stay.29
CausesThe subjective experience of pain varies from one person to another and includes several dimensions: sensory, emotional, cognitive, physiological, spiritual, and behavioural30; and so it is in turn influenced by other factors such as: age, sex, experiences prior to pain, beliefs, culture, etc.
By searching for the leading causes of pain in patients in critical condition, the Thunder Project II, whose objective was to study the patients’ pain responses when six nociceptive procedures were performed (turning, wound drain removal, endotracheal suctioning, femoral line removal, central line insertion, and wound dressing change)31 concluded that what causes the worst pain is turning, therefore the need to administer additional analgesia before the procedure is indicated.
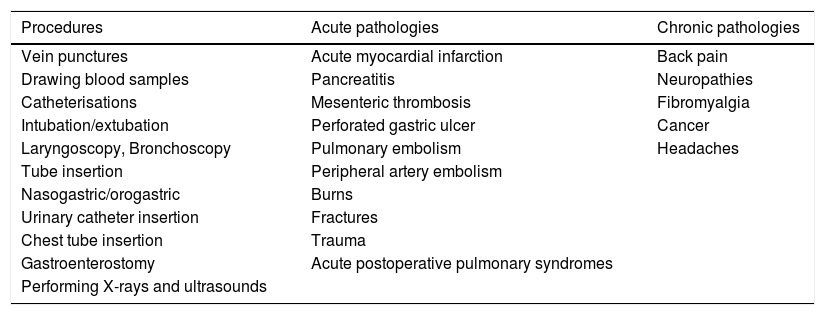
The procedures that cause the most pain are indicated in Table 2.
Common causes of pain in the ICU.
| Procedures | Acute pathologies | Chronic pathologies |
|---|---|---|
| Vein punctures | Acute myocardial infarction | Back pain |
| Drawing blood samples | Pancreatitis | Neuropathies |
| Catheterisations | Mesenteric thrombosis | Fibromyalgia |
| Intubation/extubation | Perforated gastric ulcer | Cancer |
| Laryngoscopy, Bronchoscopy | Pulmonary embolism | Headaches |
| Tube insertion | Peripheral artery embolism | |
| Nasogastric/orogastric | Burns | |
| Urinary catheter insertion | Fractures | |
| Chest tube insertion | Trauma | |
| Gastroenterostomy | Acute postoperative pulmonary syndromes | |
| Performing X-rays and ultrasounds |
Critically ill patients commonly present cognitive alterations as sequelae associated with factors of the illness itself and contextual, sociodemographic, and pharmacologic factors. In the study by Hopkins et al. (in Jones), a group of adult patients recovering from acute respiratory distress syndrome was followed for 2 years after discharge from the ICU, of which 47% were demonstrated to continue to have cognitive deterioration. Deterioration in memory and attention mainly involve the executive function areas. The executive functions are a collection of brain processes responsible for planning, cognitive flexibility, abstract thought, rule acquisition, initiating appropriate actions, suppressing inappropriate actions, and selecting relevant sensory information. This can decrease understanding of their illness, although they often recover on their own, the time can vary from one person to another, so it is important to continue monitoring them and provide the necessary information.29
One issue that is generally neglected in patients are their spiritual needs. The WHO (1990) affirms that “spirituality refers to those aspects of human life relating to experiences that transcend sensory phenomena”. It is often understood as being concerned with meaning and purpose, and for those nearing the end of life, is commonly associated with the need for forgiveness, reconciliation and affirmation of worth.” Spirituality can be expressed in any context (religious or non-religious).
The spiritual dimension is idiosyncratic of the human condition and is also universal in nature. Every person is a spiritual being who has inside themselves the ability to yearn to integrate their being with a larger reality than themselves, and at the same time, yearn for the possibility of finding the path to that integration, a path for that unique and unrepeatable person, since the spiritual dimension does not appear in the abstract, but rather is lived in specific people.
These needs can be expressed explicitly or implicitly. The manifestation and intensity vary according to the person's progress and circumstances. In addition, it is continually changing over the course of their life and they are not perceived or expressed in the same way at each stage.
The discussion about the conceptualisation of this dimension and the limits of its study remains open. Benito et al. mention some important axes for exploring spiritual needs: Search–Yearning–Aspiration–Meaning–Connection–Transcendence–Ethical values.32
The family and the healthcare team in the context of critically ill patientsDiagnosing a person as critically ill and admitting that person to a specialised unit involves a physical and psychological barrier in the family–patient relationship dynamic at a time of life crisis. The isolation of patients far from their family has repercussions for both sides, which indirectly and negatively influences the family system. From that moment, the family members run the same risk as the critically ill patient of developing affective, emotional, spiritual, and physical alterations.33 The most common emotions in family members are anxiety, fear, sadness, frustration, guilt, powerlessness, and irritability.
Plaszewska-Zywko and Gazda stress that the family members of ICU patients experience high intensity negative emotions. They report that most of the emotions are reduced by the second or third day of admission compared with the first,34 but it depends on several factors such as age, gender, severity of the patient's condition, and the family relationship. Spouses and relatively young family members have a higher incidence of symptoms of anxiety and depression, and family members of unconscious patients who are responsible for making decisions about several processes and interventions have an increased risk of distress.35 The family members of patients on mechanical ventilation have expressed “feeling connected” with their loved one, experiencing suffering with the ICU patient,36 which is called an empathic bond.
Anderson et al.37 found that 35% of family members presented symptoms of post-traumatic stress disorder related with the experience of having a loved one in the ICU 6 months after the event occurred, and 46% of those who lost a family member presented complicated grief after 6 months.38
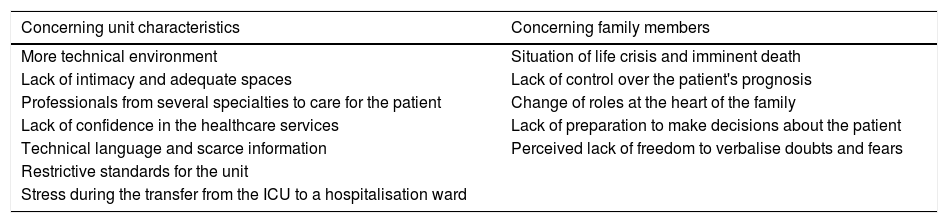
Some of the main sources of stress in the family members of critically ill patients are presented in Table 3.
Stress-causing factors in family members.
| Concerning unit characteristics | Concerning family members |
|---|---|
| More technical environment | Situation of life crisis and imminent death |
| Lack of intimacy and adequate spaces | Lack of control over the patient's prognosis |
| Professionals from several specialties to care for the patient | Change of roles at the heart of the family |
| Lack of confidence in the healthcare services | Lack of preparation to make decisions about the patient |
| Technical language and scarce information | Perceived lack of freedom to verbalise doubts and fears |
| Restrictive standards for the unit | |
| Stress during the transfer from the ICU to a hospitalisation ward |
The healthcare team can come to show unpleasant emotions that will be demonstrated in the form of burnout syndrome and/or other alterations by attaching themselves to the management of patients with a poor prognosis, work overload, and dealing with the emotions of patients and families, which affects communication, efficacy, and efficiency in their service.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestsThe authors declare that they have no conflict of interests.