RN4CAST-Chile builds upon two decades of global nursing outcomes research and the successful implementation of the RN4CAST study in 30 countries around the world to replicate this research for the first time in South America. Over 70 scientific papers in leading nursing and interdisciplinary journals have resulted just from the RN4CAST-EU study, making it the most productive study ever funded by the European Commission (www.rn4cast.eu). The results of this program of research have been influential in changing clinical practice, managerial policies, and governmental policies in many countries. Based upon the establishment of a link between lower patient to nurse ratios and better patient outcomes, a number of jurisdictions and countries have adopted safe nurse staffing standards including California in the U.S., Victoria and Queensland in Australia, Ireland, and Wales. Documentation that a nurse workforce qualified at least at the bachelor's level is associated with better patient outcomes including lower hospital mortality has been the catalyst for U.S. hospitals working toward a target date of 2020 to achieve at least a 80% bachelor's educated nurse workforce. The European Parliament for the first time approved a bachelor's pathway for nurse education. Additionally research from RN4CAST and its predecessor studies has been influential in creating the evidence base in support of redesigning clinical work environments to provide greater involvement of clinicians in institutional policy decisions and better managerial support to reduce operational errors in clinical settings that detract from nurses, doctors, and others providing safe clinical care. Chile will soon have comparable data to inform evidence-based decisions that hold promise for improving the outcomes of its health services.
A landmark study by the U.S. Institute of Medicine published in 1999 called the world's attention to the high incidence of patient harm associated with the delivery of medical care (1). It estimated that medical errors in the U.S. were among the top five leading causes of death. The World Alliance for Patient Safety was formed shortly thereafter by the World Health Organization to encourage global responses to the reduction of patient harm that was thought to be a leading cause of disease burden globally (2). A program of international research by the Center for Health Outcomes and Policy Research at the University of Pennsylvania, USA, was undertaken to determine whether variation in hospital registered nurse (RN) staffing across hospitals contributed to poor patient outcomes (3). This program of research has been implemented in 30 countries to date in various parts of the world including the latest replication a national sample of hospitals in Chile.
The purpose of this paper is to summarize the key findings from this program of research, often referred to as RN4CAST after the 15 country European Union funded study of the impact of nursing on hospital outcomes in Europe. We also describe the study that is now underway in Chile, known as RN4CAST-Chile. The study in Chile is expected to produce important and actionable findings, that if implemented, hold promise for improving the culture of patient safety in hospitals and resulting in better patient outcomes.
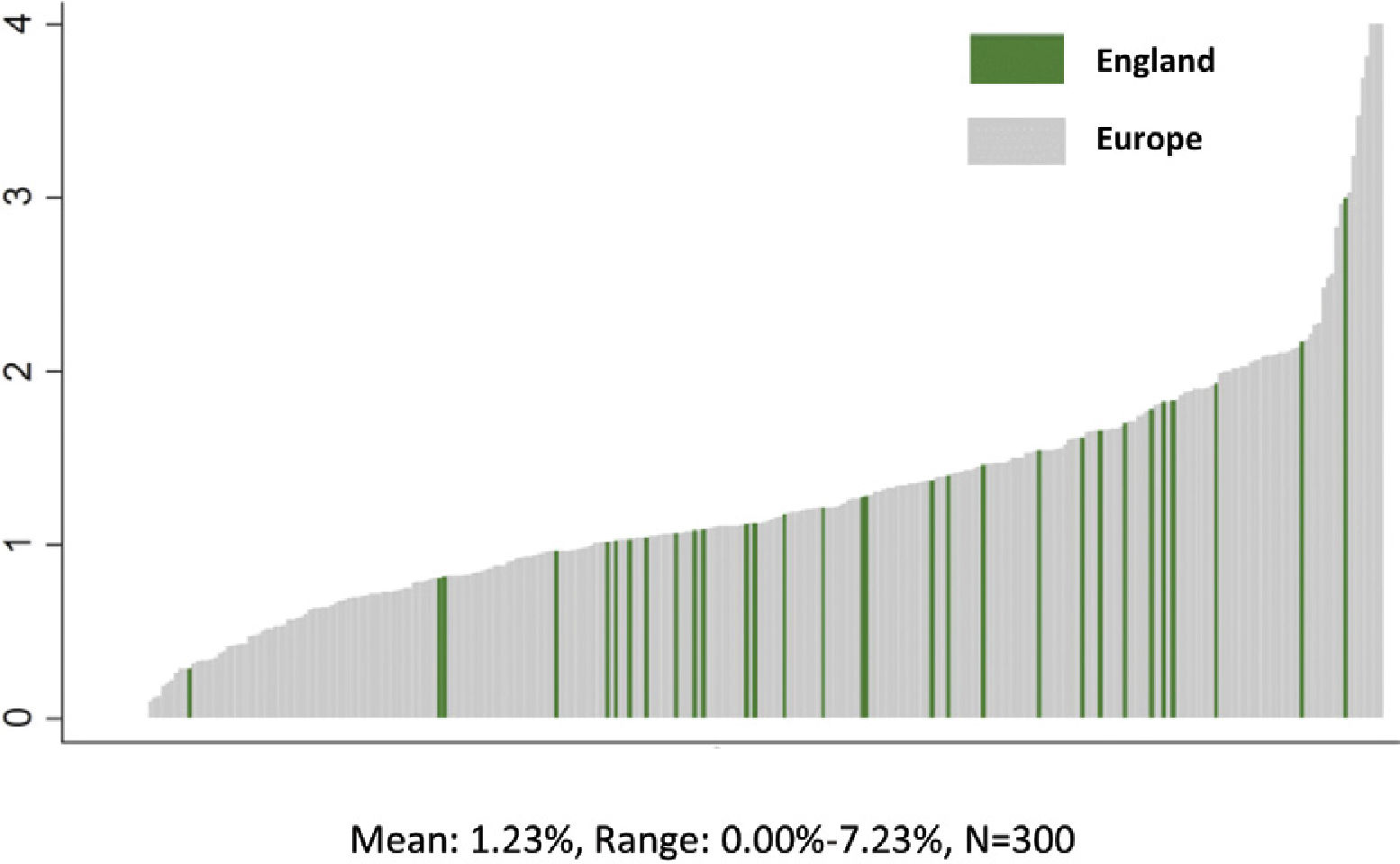
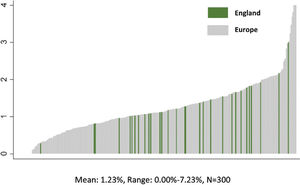
PATIENT OUTCOMES VARY BY HOSPITALResearch shows that within the same country that patient outcomes vary substantially by hospital, after taking into account that some hospitals care for sicker patients than others. The popular magazine Consumer Reports, for example, recently published an analysis of death rates in U.S. hospitals for elderly patients admitted for treatment of common acute medical conditions—pneumonia, heart failure, acute myocardial infarction—and surgery (4). Death rates for patients with these conditions were twice as high at some hospitals than for others. We found the same significant differences in death rates following common surgical procedures across 300 representative hospitals in nine European countries (5). Indeed, the differences in mortality across hospitals within country were larger than the mean differences across countries. Figure 1 illustrates this relationship by highlighting that the mortality rates for the 46 participating hospitals in England, which has a centralized national health system, vary as much as the 300 hospitals in 9 different European countries.
NURSE STAFFING LEVELS AND HOSPITAL MORTALITYThroughout this paper when we use the term “nurse”, we are referring to fully qualified professional nurse, or registered nurse (RN). We also found considerable variation in patient-to-nurse ratios across hospitals within every country we have studied. In England, for example, the average patient-to-nurse ratios for all hospitals was 8.6 but varied 5.6 patients-per-nurse to 11.5 patients-per-nurse (6). We have found similarly wide variation in patient-to-nurse ratios across hospitals in every country we have studied.
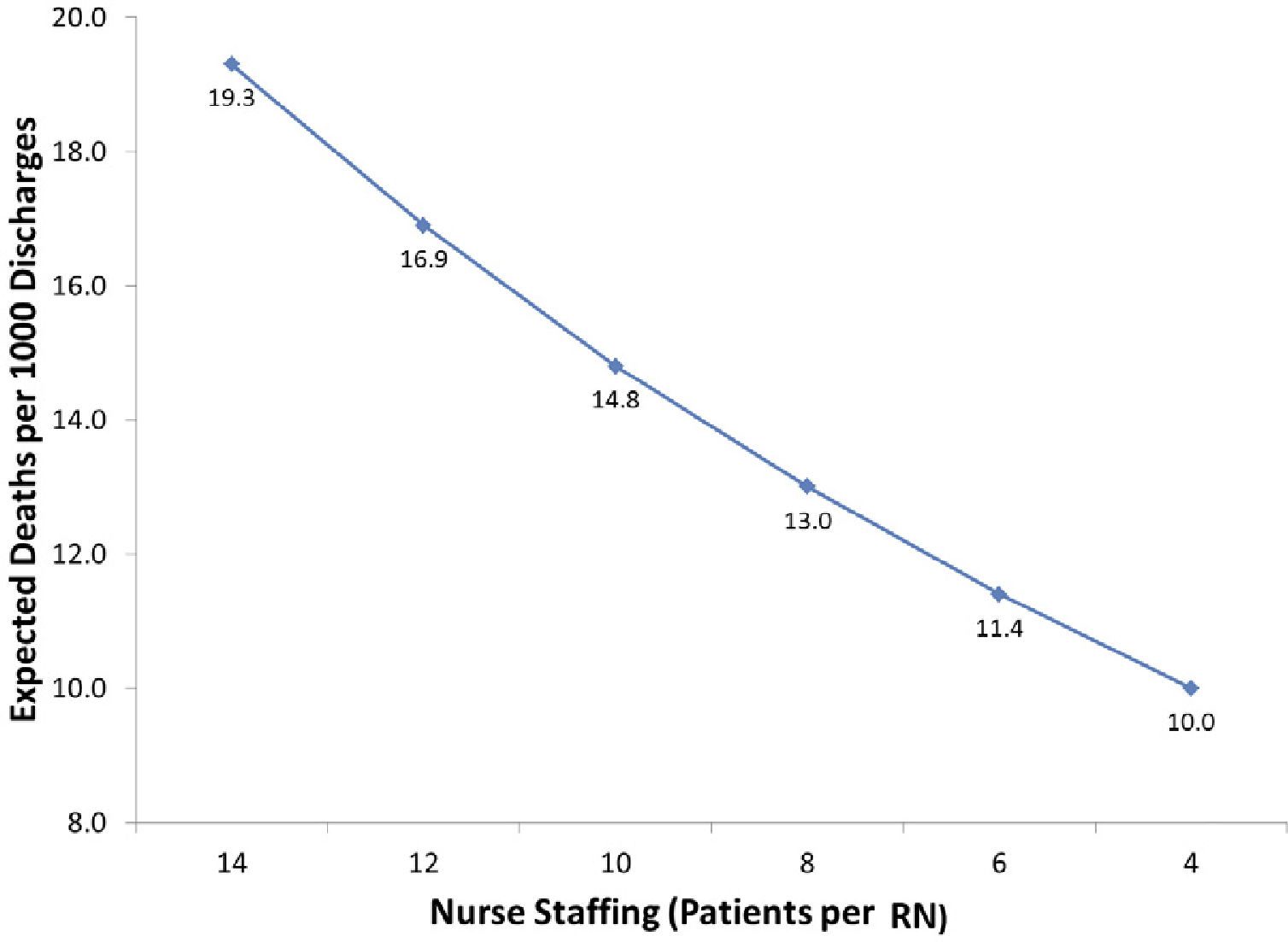
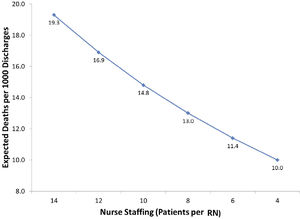
Two systematic reviews have concluded that there is strong evidence of a significant association between better nurse staffing and lower mortality (7,8). We have found across all the countries we have studied, including the U.S., Canada, England, Belgium, South Korea, and nine countries in Europe, significant associations between lower patient-to-nurse ratios and lower risk-adjusted mortality (5, 9-14). Each one patient added to a nurse's workload is associated with a 7 percent increase in risk-adjusted mortality following general surgery. Figure 2 presents in visual form the relationship between patient to nurse staffing and expected deaths per 1000 discharges from the RN4CAST-EU study of 300 hospitals in 9 European countries.
THE BUSINESS CASE FOR IMPROVED NURSE STAFFINGNational policymakers and hospital executives often view hospital nurse staffing as an expense to be minimized as much as possible. The significant variation across hospitals within countries in patient-to-nurse workloads likely results from different managerial decisions about allocation of limited resources. Evidence is beginning to accumulate about the value of investing in improved nurse staffing. This line of research documents that investing in more nurse positions offsets expenditures in other patient care categories often enough to pay for increased labor costs. Most adverse patient outcomes occurring in hospitals substantially increase the overall per patient cost of care by resulting in additional surgical procedures, more diagnostic testing, more use of expensive drugs and supplies, more days of intensive care, and longer lengths of stay in addition to pain and suffering for patients (15). We offer below some examples from the RN4CAST international nursing outcomes research demonstrating that having too few nurses may cost more when all the costs of patient care are considered.
In a recent publication in JAMA Surgery from RN4CAST-US, we used patient matching techniques to create 25000 patient pairs that were the same in terms of surgical procedure, co-morbid conditions such as hypertension, age, sex, and other surgical risk factors (16). We divided hospitals into groups depending upon the extent of nursing resources, controlling for high technology and other hospital characteristics, and compared the outcomes and costs for the matched patients in well nurse resourced hospitals versus poorly nurse resourced hospitals. Patients in well nurse resourced hospitals were significantly less likely to die at every patient risk level and their total care costs were the same or less in the high nurse resourced hospitals than in the low nurse resourced hospitals. Higher nurse resourced hospitals, with higher labor costs, were able to achieve better patient outcomes at the same or lower costs than hospitals with worse patient outcomes because the higher nurse resourced hospitals admitted 40 percent fewer patients to expensive intensive care units; also length of stay was shorter in well nurse resourced hospitals. In summary, the higher labor costs in hospitals with more nurses were offset by reduced intensive care use and shorter length of stay. This is a good example of the business case for hospitals employing more professional nurses.
In a different paper, we documented that the rate of expensive hospital-acquired infections (HAIs) varied significantly across hospitals in the same country (17). Hospitals with the best nurse staffing had 30 percent fewer hospital acquired infections than hospitals with poor nurse staffing after taking into account patient risk factors and characteristics of hospitals such as size, technology, and teaching status. The cost-savings from prevention of HAIs offset, at least in part, higher labor costs associated with the employment of more nurses.
Another large and potentially preventable cost of hospital care is hospital readmissions within 30 days of discharge. In RN4CAST, we have examined the association of hospital nurse staffing and readmission rates. Our results show that every one additional patient added to nurses’ workloads is associated with between a 6-9 percent increase in readmissions for patients with pneumonia, heart failure, and acute myocardial infarction (18); 8 percent increase in readmissions after hip and knee replacement (19); 3 percent increase in readmissions after general surgery (20); and 11 percent increase in readmissions for hospitalized children (21), unnecessarily adding to cost of care. About half of nurses report on their last shift being unable because of lack of time to complete discharge planning and patient teaching. Thus, research showing the link between better nurse staffing and lower readmission rates is an example of how investments in human capital, namely in hiring more nurses, potentially pays for itself by avoiding the high costs of readmissions.
A final example of research pertinent to the business case for improved investments in professional nurse staffing pertains to the composition of bedside caregivers by qualifications. A common but unfounded assumption is that less qualified and lower paid staff can be substituted for professional nurses without adversely affecting patient outcomes or cost of care. A growing research literature presents evidence to the contrary. Needleman (22) in a study of nursing skill mix in U.S. hospitals, showed that holding constant the total number of hours of care, replacing lower qualified licensed practical nurses, that are the equivalent of technical nursing staff in Chile, with fully qualified professional nurses would save money and lives. Technical level nursing staff were paid 30 percent less than professional nurses but had a more limited scope of practice, and had to be supervised by professional nurses thus eroding the value of their lower salaries. Additionally, the greater the proportion of technical nurses, the worse the outcomes for patients, including expensive adverse outcomes like infections and falls with injuries (23). Taking into account all of these factors, the Needleman study confirmed that it cost hospitals more to have fewer fully qualified nurses. We confirmed similar findings and a strong business case in favor of a higher proportion of professional nurses in the composition of the bedside care workforce in the RN4CAST-Europe study of 243 hospitals in 6 European countries (24). We found that every 10 percent increase in the proportion of professional nurses among all nursing care personnel at the bedside was associated with 11 percent lower odds of mortality after general surgery and 10 percent lower odds of poor hospital ratings from patients. Costly adverse patient outcomes including pressure ulcers, falls with injuries, and urinary tract infections occurred significantly less frequently in hospitals with a higher proportion of professional nurses. In summary, an increasing number of studies shows that total costs of care are often higher in hospitals that employ too few professional nurses.
RN4CAST-CHILEThe Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing is partnering with Chilean colleagues at schools of nursing at four universities to replicate RN4CAST in Chile: Universidad de los Andes, Pontificia Universidad Católica de Chile, Universidad de La Serena, and Universidad de Concepción. Chile is the first country in South America to participate in the international RN4CAST study that has to date been implemented in 30 countries in different parts of the world. The Chilean nurse-led research consortium is committed to undertaking a program of research that helps strengthen health services and policy research in nursing in Chile, and provides rigorous evidence that can inform practice, management, and policy decision-making to promote health care that is effective, affordable, and satisfactory to the public.
RN4CAST-Chile uses previously validated instruments and measures from RN4CAST-US and RN4CAST-EU (25). Data are collected from four sources: 1) Surveys from a sample of registered nurses (RNs) recruited directly from 43 public and private general acute hospitals participating in the recently implemented patient GRD system using the validated RN4CAST nurse survey instrument; 2) GRD patient discharge data obtained through the Ministry of Health; 3) survey of hospitalized patients in the study hospitals using the Hospital Consumer Assessment of Healthcare Provider and Systems (HCAHPS) patient experience/satisfaction surveys validated in Spanish (26); and 4) data on characteristics of hospitals including size, public-private ownership, teaching status, technology availability, rural-urban location. Ethics approvals have been obtained to access de-identified patient data for each study hospital. Ethics committee approvals are being obtained directly from each participating hospital. Results will be published in the aggregate only and individual hospitals will not be identified.
The resulting Chilean data will be analyzed to determine the effects of registered nurse (RN) staffing and the nurse practice environment on patient and nurse outcomes. We will examine variation in nursing resources across hospitals in Chile and their relationship to patient outcomes to develop specific recommendations for improving patient outcomes in Chile and getting more value for investments in health care. We will provide international comparisons of Chilean results from RN4CAST studies in other countries to offer further insights into strategies that could improve quality of hospital care and patient outcomes in Chile.
SPECIFIC AIMTo determine the association of nurse staffing, nurse skill mix and the nurse work environment with patient outcomes. The outcomes to be studied include risk-adjusted mortality, failure to rescue, patient satisfaction, readmissions, length of stay, nurse satisfaction and burnout, and other outcomes as feasible to measure from GRD data.
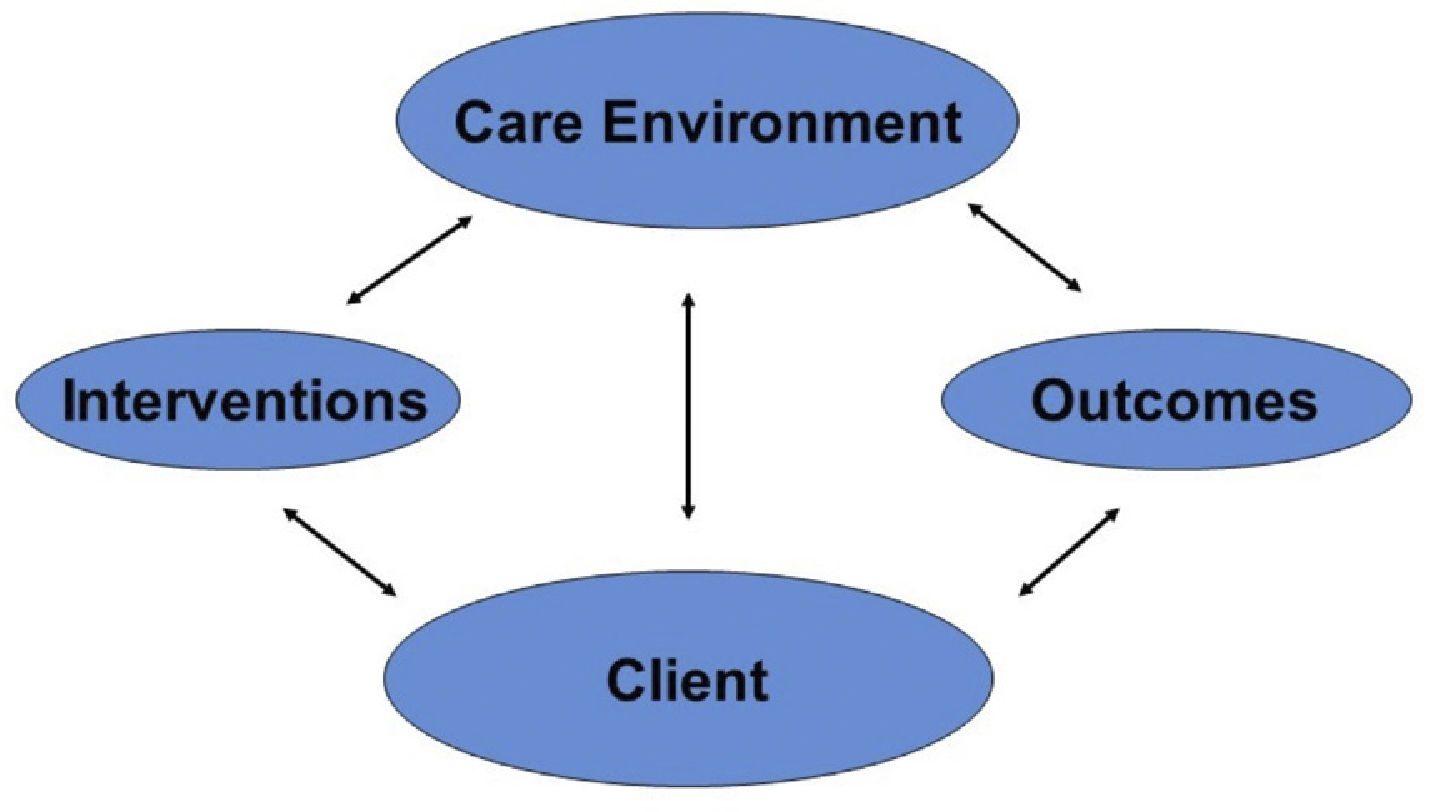
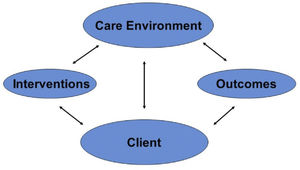
CONCEPTUAL FRAMEWORKThe overarching conceptual framework that guides the study is the Quality Health Outcomes Model (QHOM) (27). This model is an elaboration and extension of Donabedian's (28) essentially linear conception of quality that structure affects processes, which in turn affects outcomes. The Quality Health Outcomes Model posits that the effects of interventions are mediated by client and system characteristics; no independent direct effect on outcomes is assume, as depicted in Figure 3. Relationships specified by the QHOM are consistent with observations that there are far more nursing and medical interventions that have been shown to be successful under controlled conditions to improve patient outcomes but do not have their intended effects once introduced into usual practice conditions. Our 25 years of research has amassed substantial evidence that modifiable “system” features such as patient to nurse staffing ratios, nursing workforce skill mix, the composition of the RN workforce by educational qualifications, and the quality of the work environment mediate the outcomes of interventions such as in-hospital resuscitation (29); infection prevention (17); and the rescue of patients experiencing complications in the hospital (12).
METHODResearch DesignThe same research protocol and measures used in RN4CAST are used for the Chile data collection. These methods and measures have been extensively validated in published research papers (30, 31). A nationally representative sample of hospitals, public and private, participating in the GRD patient data system are expected to participate in the study. In each participating hospital, all nurses in adult medical and surgical units will be asked to participate in the survey. Additionally 100 patients will be recruited from the same medical and surgical units in each participating hospital to complete the patient experience survey. Patients must be cognitively and physically able to complete the survey and have been hospitalized for 3 days or longer.
Measures: The nurse survey includes the internationally validated Practice Environment Scale of the Nursing Work Index to measure the quality of the nurse work environment (32). The Maslach Burnout Inventory is used to measure nurse burnout (33). Nurses report a range of information about their workloads, the number and kinds of other direct care staff that we have used in multiple high impact scientific journals to measure patient-to-RN ratios. Patient to RN ratios are determined from RN surveys of how many RNs and patients there are on each nurse's last shift worked. For each medical and surgical unit, excluding ICUs, we average the responses together of how many RNs and patients are on each unit. We divide the number of patients by the number of RNs. Results from each unit are aggregated to create a hospital level average. The validated HCAHPS survey is used to measure patient experience and satisfaction with hospital care (26).
Patients: The GRD patient data system in Chile closely resembles the U.S. DRG system. We propose in this study, as in much of our international research, to focus on outcomes of patients undergoing general surgery, orthopedic surgery, and uncomplicated vascular surgical procedures, and the major causes of medical hospitalizations including acute myocardial infarction, heart failure, pneumonia, and GI bleeding. We focus on these GRDs because patient risk adjustment procedures are well developed and data are available to better distinguish complications that occur in the hospital from comorbidities present on admission. We will obtain individual level data for every patient over a one-year period that coincides with the surveys of nurses and patients.
ANALYSISAggregating the data to the hospital-level, we will use the cross-sectional dataset look at several staffing and work environment measures (ratios, skill mix, work environment), patient outcomes (mortality and failure to rescue, readmission, length of stay, non-mortality adverse outcomes, risk adjustment, hospital quality of care indicators, patient satisfaction) and hospital outcomes (burnout, job dissatisfaction, intent to leave, hospital financial indicators). We will compare several of these descriptive statistics and bivariate correlational matrices will be constructed to examine individual relationships between predictor and outcomes variables. Independent variables that are correlated with the dependent variable at p < .05 will be analyzed in a multivariate regression model. Second, bivariate regression models will be constructed to test the relationships between predictor variables. Nurse survey data are used to derive hospital-level nursing measures (staffing, skill mix, nurse education, and the nurse work environment). We will then combine these measures in a hospital-level dataset with the other hospital characteristics (bed size, teaching status, technology, location, and ownership). Then we merge these hospital-level measures with the individual-level patient data to enable the multi-level analyses of patient outcomes (including mortality, failure to rescue, patient satisfaction, and readmissions).
Depending on the measures used in the different analyses, we will use disaggregated analytic techniques (in which individual patient-level data are used, similar hospital-level values are assigned to each patient in the same hospital, and generalized estimating equations are employed), aggregated analytic techniques (in which patient outcomes are aggregated to the hospital level by averaging, and ordinary least squares models are used), and by using hierarchical linear models (HLM), in which both levels are explicitly retained and modeled separately. We will rely heavily on HLM models which, since our observations are nested, often do a better job of disentangling individual and group effects on the outcomes of interest (39, 40). The important points are that when outcome characteristics pertain to patients or nurses, the outcome variables are measured at the individual level. Our main predictor variables are measured at the aggregate level, primarily as averages of individual responses. For example, when patient mortality is regressed on the nursing work environment, we have outcome data for the individual patient (whether they died or not) as well as patient-specific data on severity at time of admission. Evaluations of the nursing work environment are obtained from individual nurses, but in our design, there is no connection between particular nurses and particular patients. So the nursing work environment is a property of the hospital, based on the mean scores of sampled nurses. An aggregate-level predictor cannot explain variation within a group, so in this sense the patient outcomes are similarly averages within hospitals. However, by adjusting for severity at the individual (patient) level, we can ensure that variation between hospitals explained by nursing factors is net of variation between hospitals better attributed to differences in patient populations.
Funding: Funding for RN4CAST-Chile was provided by the University of Pennsylvania from its Global Fund, the Center for Health Outcomes and Policy Research in the School of Nursing, and the Population Research Center. Additional funding was provided by Sigma Theta Tau International. The funding was provided to facilitate the overall conduct of a scientific study.