Cryptococcosis is a generally systemic and potentially lethal fungal infection. Although HIV infection is a predisposing condition, especially if the CD4+ lymphocyte count is less than 100cells/mm3, other forms of immunosuppression may be associated with this opportunistic fungal condition, such as prolonged steroid therapy or solid organ transplantation. Pulmonary presentation must be included in the differential diagnosis of pneumonia or pulmonary neoplasia in the immunosuppressed patient.
Case reportWe report a case of pulmonary cryptococcosis in a non-diagnosed HIV patient. In a 44 year-old male suffering from dyspnea and chest pain the image of a pulmonary nodule was observed in a radiological finding. In the histopathological study, intracellular structures suggestive of fungal conidia, and morphologically compatible with Cryptococcus, were observed. HIV serology and cryptococcal antigen detection in serum were requested, given the possibility of cryptococcosis. Cryptococcus neoformans var. grubii was isolated from the culture of the pulmonary biopsy. The patient was finally diagnosed with pulmonary cryptococcosis and HIV-1 infection. With a proper antifungal treatment the patient evolved satisfactorily.
ConclusionsThe best strategy to avoid opportunistic infections such as cryptococcosis in HIV-infected patients consists of an early diagnosis and a highly active antiretroviral treatment. In our case, the diagnosis of a pulmonary infection by C. neoformans var. grubii allowed a late diagnosis of HIV-1 infection.
La criptococosis es una infección fúngica generalmente sistémica y potencialmente letal. Aunque la infección por VIH es una condición predisponente, especialmente si el recuento de linfocitos CD4+ es inferior a 100células/mm3, otras formas de inmunosupresión, como la terapia prolongada con esteroides o el trasplante de órgano sólido, pueden asociarse a esta micosis oportunista. La forma pulmonar debe incluirse en el diagnóstico diferencial de neumonía o neoplasia pulmonar en el paciente inmunodeprimido.
Caso clínicoPresentamos un caso de criptococosis pulmonar en un paciente con VIH no diagnosticado. Varón de 44 años aquejado de disnea y dolor torácico en el que como hallazgo radiológico se observa un nódulo pulmonar. En el estudio histopatológico del mismo se observaron estructuras intracelulares sugestivas de conidias fúngicas, morfológicamente compatibles con Cryptococcus. Ante la sospecha de criptococosis se solicitó la serología de VIH y la detección en suero de antígeno criptocócico. Se aisló Cryptococcus neoformans variedad grubii de la siembra de la biopsia pulmonar. El paciente fue finalmente diagnosticado de criptococosis pulmonar e infección por VIH-1. Con el tratamiento antifúngico, el paciente evolucionó satisfactoriamente.
ConclusionesLa mejor estrategia para evitar infecciones oportunistas como la criptococosis en pacientes infectados por VIH consiste en un diagnóstico precoz y un tratamiento antirretroviral de gran actividad. En este caso, el diagnóstico de infección pulmonar por C. neoformans var. grubii permitió un diagnóstico tardío de infección por VIH-1.
Cryptococcosis is a generally systemic and potentially lethal fungal infection that can affect immunocompetent individuals, but it is more frequently diagnosed in immunosuppressed patients.15 Risk factors for acquiring cryptococcal infection are lymphoproliferative disorders, systemic lupus erythematosus, sarcoidosis, rheumatoid arthritis, corticosteroid therapy, diabetes, chronic lung disease, liver disease or chronic nephropathy, use of monoclonal antibodies or solid organ transplantation, among others.12,17 HIV infection predisposes this condition,8,10 especially if the CD4+ lymphocyte count is less than 100cells/mm3. Pulmonary cryptococcosis is clinically characterized by a febrile episode with dyspnea, cough, nocturnal sweating and progressive respiratory deterioration. Immunosuppression contributes to a hematogenous spread to the central nervous system18 and other locations, such as the skin. Although the most frequent and severe forms are cryptococcal meningitis and meningoencephalitis,14 the pulmonary cryptococcosis must be included in the differential diagnosis of pneumonia or pulmonary neoplasia in the immunosuppressed patient. The most common radiological pattern is multiple nodular involvement.5,13 In addition, lobar or segmental consolidation and thoracic adenopathies can be observed. The diagnosis and an early treatment of pulmonary cryptococcosis, as well as the knowledge of HIV condition, are essential for the control and prognosis of the infection.6
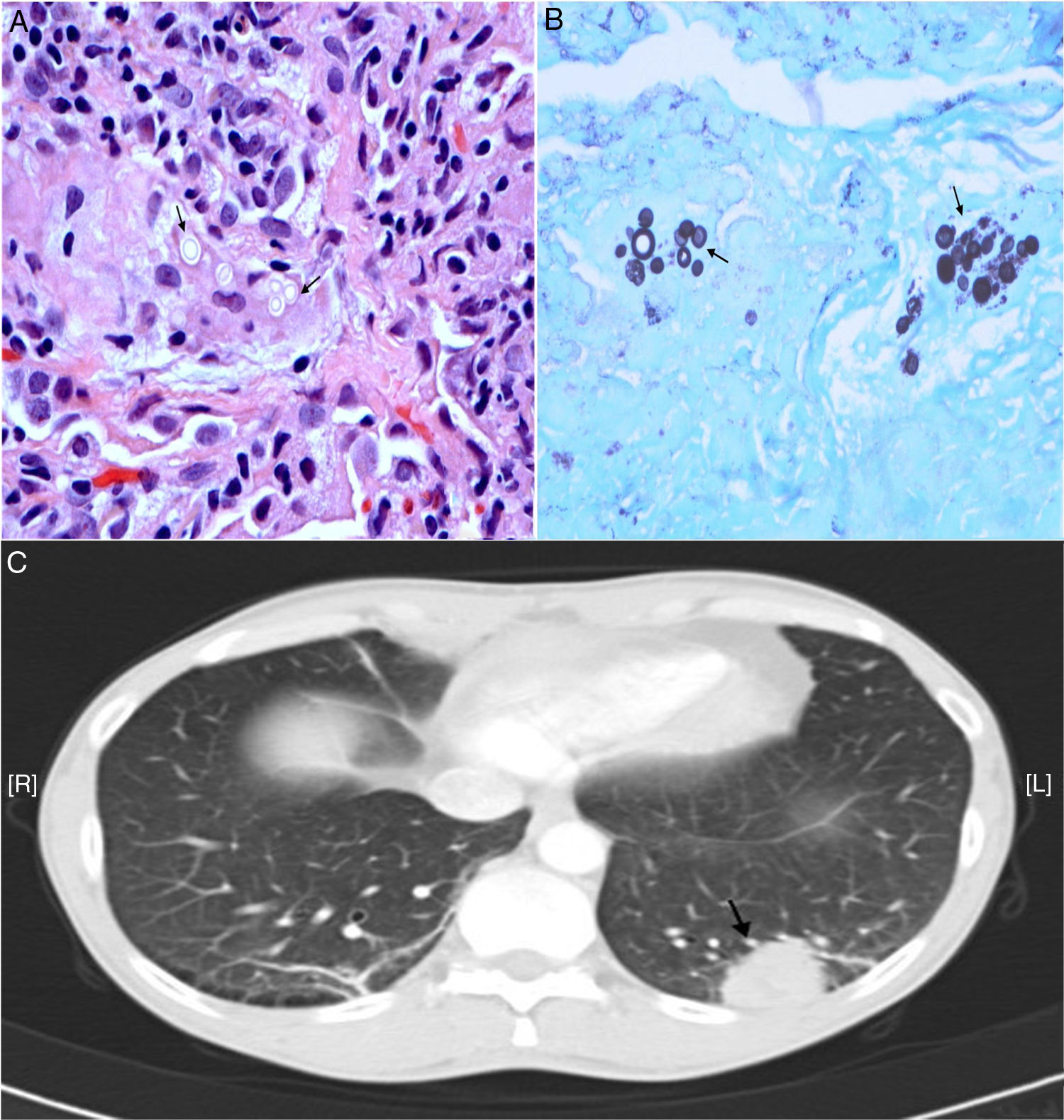
Case reportA 44 year-old male, in a situation of social exclusion, chronic tobacco smoker and with a personal history of spontaneous pneumothorax, bronchial asthma, and chronic cervical adenitis, was referred to our department. He complained of progressive dyspnea with chest pain, asthenia, anorexia and an unquantified weight loss. As a radiological finding after a chest X-ray and a computed tomography (CT) scan in December 2016, a 19mm pulmonary nodule was observed in the left lower lobe with an adjacent 6mm nodule in the same lobe and multiple bilateral axillary adenopathies of pathological size, with emphysematous changes of the centrilobular paraseptal type. The findings observed in the CT suggested a primary neoformative process, so the patient was referred to the Rapid Diagnosis Unit of Lung Cancer. Bronchodilator and analgesic treatments were started, and the Pneumology Department requested the following exams: tumor markers, positron emission tomography–computed tomography (PET–CT), bone scintigraphy, fiberoptic bronchoscopy and respiratory function tests (RFT). During this period the patient required admission to the Psychiatry Department being diagnosed of adaptive disorder with paranoid stress reaction; benzodiazepines and atypical antipsychotic were prescribed. Tumor marker tests were negative and bone metastases was discarded in the scintigraphy. RFT reflected a slight decrease in total lung capacity. PET–CT confirmed high metabolic activity of the lung nodule. In May 2017, fiberoptic bronchoscopy was performed, and samples of transbronchial biopsy and bronchial brushing of the left lower lobe and axillary adenopathy were collected and sent to the Pathology Department. Moreover, a lung biopsy sample was sent to the Microbiology Department for a microbiological study. In the histopathological study, focal chronic granulomatous inflammation with multinucleated giant cells was observed, with intracellular structures suggestive of fungal conidia, morphologically compatible with Crypytococcus (Fig. 1). Due to the possibility of cryptococcosis, HIV serology and detection in serum of cryptococcal antigen were performed. The lung biopsy was seeded on Sabouraud dextrose agar at 25 and 37°C, and the isolate obtained after 48–72h of incubation was identified as Cryptococcus neoformans var. grubii by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. In order to confirm the variety of the species identified, the strain was sent to the National Center of Microbiology, where the identification of the variety was confirmed, and the sensitivity to fluconazole was tested (MIC of 2mg/l). HIV screening by means of a fourth-generation enzyme immunoassay was positive, therefore being the patient infected by type HIV-1. The detection of cryptococcal serum antigen by latex agglutination (Crypto-La test, Fumouze®) was positive with a low titer of 1:2. Afterwards, the detection of the HIV-1 load in plasma was performed, with a result of 464,000copies/ml (5.67 log10); a lymphocyte subpopulation study was carried out, finding a CD4+ count of 235cells/mm3. The patient was finally diagnosed with HIV-1 infection and pulmonary cryptococcosis without clinical–radiological evidence of meningoencephalic involvement. In June 2017, he started a treatment with fluconazole (400mg/day, 10 weeks), with a favorable development. The patient was also prescribed a highly active antiretroviral therapy in July 2017, Triumeq® (dolutegravir/abacavir/lamivudina), and a month later the viral load of HIV-1 was 97copies/ml with a CD4+ count of 251cells/mm3. The cryptococcal antigen in serum became negative.
(A) Hematoxylin–eosin stain, ×400. Multinucleated giant cells with several intracellular rounded yeasts with peripheral light halo. (B) Grocott stain, ×400. Multinucleated giant cells with several rounded intracytoplasmic yeasts with positive staining of the wall. (C) Computed tomography. Pulmonary nodule in the left lower lobe.
The clinical manifestations of pulmonary mycosis are nonspecific,9 although the suspicion is simpler if the condition of immunosuppression is known. The differential diagnosis of any pulmonary nodule, especially in HIV-infected patients, should include pulmonary cryptococcosis.7,19 However, in the case presented here, the diagnostic algorithm was inverse as the immunosuppression of the patient was not known. The diagnosis of a pulmonary infection by C. neoformans allowed the diagnosis of the HIV-1 infection, which remained unknown until that moment. In this case, the treatment of mycosis depends not only on the use of antifungals, but also on reversing immunosuppression.3,6 At the time of the diagnosis, the patient presented a very low titer of cryptococcal serum antigen. Serum titers from 1:8 usually indicate an active disease.2 However, serum determination of cryptococcal antigen may be negative in exclusively pulmonary forms. Achieving a diagnosis and starting an early treatment are essential to avoid dissemination and the onset of more serious forms of cryptococcosis, such as cryptococcal meningitis or meningoencephalitis.16 In addition, the latent infection by C. neoformans in the pulmonary lymphatic tissue can be reactivated after a long period, as it occurs with tuberculosis. Another possible complication is the appearance of an inflammatory immune reconstitution syndrome following the start of antiretroviral therapy.4,11 This syndrome may be due to the recovery of the specific immune response. The best strategy to avoid opportunistic infections such as cryptococcosis in HIV-infected patients consists of an early diagnosis and a highly active antiretroviral treatment.1 Maintaining a CD4+ lymphocyte count of more than 200cells/mm3 is critical: most patients with HIV and cryptococcosis have CD4+ counts below 100cells/mm3. In Spain, it is estimated that 30% of the HIV-positive patients are unaware of the infection. Expanding the offer of the diagnostic test is essential to reduce the morbidity and mortality associated with a late diagnosis, 48% in 2017, according to data from the national information system on new HIV diagnoses. Currently, the national health system promotes the offer of a diagnostic test directly to patients with diseases indicative of a HIV infection. In this case, the presence of pulmonary nodules associated with a C. neoformans var. grubii infection allowed a late diagnosis of HIV-1 infection.
Conflict of interestThe authors declare that there is no any conflict of interest among them or with any financial organization regarding the material discussed in the present manuscript.
We thank the National Center of Microbiology for its collaboration.