Sporotrichosis has been occurring as outbreaks in Brazil, reaching epidemic levels in some regions. Zoonotic transmission is the main route to acquire Sporothrix.
Case reportWe describe a case of disseminated sporotrichosis caused by Sporothrix brasiliensis in an HIV/AIDS patient, with the presentation of immune reconstitution inflammatory syndrome (IRIS).
ConclusionsThis case reinforces that sporotrichosis should always be suspected in patients with IRIS from endemic regions, even in patients without the typical cutaneous lesions of this mycosis.
La esporotricosis suele aparecer en Brasil en forma de brotes y alcanza tasas epidémicas en algunas regiones. La ruta principal de transmisión es la zoonótica.
Caso clínicoDescribimos un caso de esporotricosis diseminada causado por Sporothrix brasiliensis en una paciente con VIH/sida que presentó un síndrome inflamatorio de reconstitución inmune (SIRI).
ConclusionesEste caso demuestra que en regiones endémicas de esporotricosis esta micosis siempre debe ser sospechada en casos de SIRI, incluso en pacientes sin las lesiones cutáneas típicas de esta enfermedad.
Hyperendemic and epidemic levels of zoonotic sporotrichosis are presently described in different states of Brazil.7 In these regions, severe forms of this disease are often described, especially associated with HIV/AIDS patients.2,4 Sporotrichosis associated with the immune reconstitution inflammatory syndrome (IRIS) was described so far only in Rio de Janeiro (RJ).9 Southern Rio Grande do Sul (RS) has the second highest prevalence of this mycosis, and most of these cases are found in Rio Grande city (RG), which has the highest prevalence of HIV/AIDS among Brazilian cities with more than 100,000 inhabitants.3,10 This study reports a case of disseminated sporotrichosis in an HIV/AIDS patient, with a suggestive presentation of IRIS. In addition, we performed a literature review of similar cases.
A 38 year-old woman, living in RG (RS, Brazil), with an HIV infection diagnosed in 2008 and with low adherence to active antiretroviral treatment (ART), was admitted to the University Hospital of RG (HU-FURG/EBSERH) in March 2019. She complained of cough of four weeks’ duration. Her HIV viral load was 53,565 RNA copies (log=4.72) and CD4 T-cell count was 62cells/mm3 (6%). Chest computed tomography (CT) showed faint “frosted glass” opacities, and a sputum sample was collected to diagnose the apparent pulmonary infection. All microbiological exams of the sputum (direct microscopy; bacterial, fungi and mycobacterial cultures) were negative. Empirical treatment for a bacterial pneumonia with levofloxacin (500mg/day for 7 days) was prescribed, as well as Pneumocystis prophylaxis with sulfamethoxazole-trimethoprim (SMX-TMP). One week later (March 26th) a first-line ART regimen (HART) (tenofovir/lamivudine and dolutegravir) was started.
In April 2019, the patient returned as an outpatient with complete remission of the respiratory symptoms, and chest CT was not repeated. She complained then about oral lesions (resembling candidiasis), arthralgia and cutaneous pruritic lesions scattered over all her body surface, including her face. Oral loratadine (10mg/day) and oral nystatin (10ml, 1ml containing 100,000U), both four times a day, were prescribed for seven days. On the next day, the blood parameters showed eosinophilia, which was interpreted as a drug reaction. SMX-TMP was discontinued, and promethazine 25mg plus prednisone 40mg daily were prescribed for five days.
The following week she returned with new lesions on her hands, back (central pustules surrounded by erythema) and face (small pustules) (Fig. 1A). Dolutegravir was changed to atazanavir/ritonavir, and prednisone 20mg/day was maintained. Due to the lack of clinical response, after three days, the patient was hospitalized to perform a skin lesion biopsy; all drugs were discontinued, including ART. At this point, hydrocortisone (250mg, intravenous, single dose) and prednisone (40mg/day, orally for five days, and with dose scaling for two weeks) were prescribed.
Disseminated sporotrichosis in an HIV patient. A. Erythematous papules and pustules appeared after 14 days of active antiretroviral treatment (ART) – before the diagnosis of sporotrichosis (April 2019). B. Skin lesions evolution, showing ulcers and crusts. Sporotrichosis was confirmed and amphotericin B deoxycholate treatment was prescribed (May 2019). C. Regression of lesions after 77 days of itraconazole (August 2019).
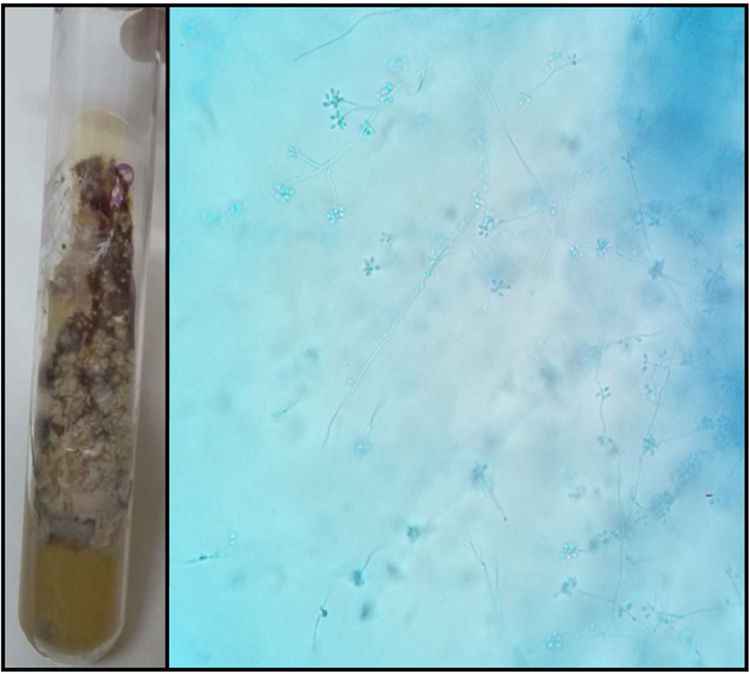
After seven days, her HIV viral load was 350 RNA copies (log=2.54) and CD4 T-cell count 168cells/mm3 (13.6%). The ART was restarted. Sporothrix spp. was isolated from skin biopsy culture (Fig. 2), and identified as Sporothrix brasiliensis by species-specific PCR.11 Histopathological findings showed moderate chronic superficial and deep perivascular inflammatory process, with the presence of macrophages and histiocytes. At the time of the sporotrichosis confirmation (May 2019) (Fig. 1B), intravenous amphotericin B deoxycholate (AmB) was started in an initial dose of 20mg/day, which was gradually increased to 50mg/day. After one week of treatment, the patient reported pain relief and improvement of the cutaneous lesions. Regression of all lesions was observed and several scars appeared on the skin lesions after 21 days of treatment; a week later AmB was stopped. The patient was discharged with a therapeutic plan of ART (atazanavir, lamivudine, ritonavir), SMX-TMP and itraconazole (200mg/day, orally) for 12 months. An undetectable HIV viral load was confirmed and the CD4 T-cell count was 221cells/mm3 (15.4%). In August 2019 (after 77 days of itraconazole), a follow-up appointment confirmed that all lesions had cleared (Fig. 1C).
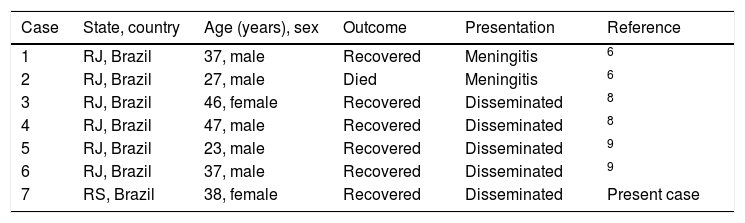
A bibliography search performed in PubMed database using the descriptors “IRIS or immune reconstitution inflammatory syndrome and sporotrichosis” resulted in only three studies, which described six cases of IRIS presentation in patients with sporotrichosis (Table 1).
Cases of IRIS in patients with sporotrichosis reported in scientific literature until 2019.
| Case | State, country | Age (years), sex | Outcome | Presentation | Reference |
|---|---|---|---|---|---|
| 1 | RJ, Brazil | 37, male | Recovered | Meningitis | 6 |
| 2 | RJ, Brazil | 27, male | Died | Meningitis | 6 |
| 3 | RJ, Brazil | 46, female | Recovered | Disseminated | 8 |
| 4 | RJ, Brazil | 47, male | Recovered | Disseminated | 8 |
| 5 | RJ, Brazil | 23, male | Recovered | Disseminated | 9 |
| 6 | RJ, Brazil | 37, male | Recovered | Disseminated | 9 |
| 7 | RS, Brazil | 38, female | Recovered | Disseminated | Present case |
Despite the high incidence of sporotrichosis and HIV in Southern RS, co-infection with these diseases in this region is not often reported.3,10 Here we report a case of an unusual presentation of sporotrichosis in an HIV patient with a clinical diagnosis of IRIS. The main criterion to define IRIS is the development of diseases that show atypical presentations in patients treated with ART, resulting in HIV viral load reduction and the recovery of the immune response; these conditions were well documented in our patient.5 In the initial presentation the patient had neither skin lesions nor a history of traumatic fungal inoculation, therefore, there was no clinical or epidemiological suspicion of sporotrichosis.1 Acute disseminated lesions appeared concurrently along with immune system recovery. However, the appearance of highly pruritic lesions with eosinophilia suggested a drug-induced dermatitis. Thus, the patient was treated with corticosteroids, which resulted in exacerbation of the lesions and delayed of sporotrichosis diagnosis associated with IRIS.
The source of infection could be pinpointed with the molecular identification of S. brasiliensis, inferring the zoonotic transmission. The patient had contact with cats in a high incidence region of sporotrichosis among felines, caused by S. brasiliensis.2 Indeed, this species may exhibit unusual clinical forms of this disease, as in the present report.7 This case highlights that in hyperendemic areas of sporotrichosis this mycosis must be considered in the differential diagnosis in all patients with cutaneous lesions, especially in those under immunosuppressed conditions, to facilitate early diagnosis and appropriate treatment.8
This is the first report of IRIS associated with HIV and sporotrichosis co-infection in Southern RS. The assessment with a few other reports from our country (Table 1) shows that all cases occurred in regions of high incidence of zoonotic sporotrichosis.7 It is important to emphasize that as a huge and quick geographic expansion of zoonotic sporotrichosis has been occurring in Brazil, health professionals must be aware regarding atypical and more severe cases which can occur mainly in immunosuppressed patients.
Ethical approvalThis project was approved by the Health Research Ethics Committee of the Universidade Federal do Rio Grande (FURG), under number 234/2018. Patient consent was obtained, and all the procedures performed were in accordance with the ethical standards of the institution. Informed consent was obtained from all individual participants reported in the study.
Conflict of interestAll authors declare that they have no conflicts of interest pertaining to this work.
This study was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior from the Ministry of Education, Brazil (CAPES-BR), under the CAPES-PrInt Program - Finance Code 001. RMZ-O was supported in part by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq 302796/2017-7) and Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio deJaneiro (FAPERJ E-26/202.527/2019).