Histoplasmosis is a systemic mycosis caused by Histoplasma capsulatum. The disseminated form is more commonly a result of reactivation of quiescent foci in immunosuppressed patients, more frequently HIV-infected.6,7,9 Disseminated histoplasmosis in immunocompetent individuals is rare. Among 107 cases of disseminated histoplasmosis reported from a University Hospital in Brazil only one case was observed in an immunocompetent patient.3 In a large series of 123 cases of histoplasmosis in HIV-negative immunocompetent patients, 32 (26%) were reported as subacute/chronic disseminated form, half of them associated with other systemic disease.2 In these cases the picture was lung and mucosal involvement associated with lymphadenomegaly or hepatomegaly and the skin was affected in only two patients (6.2%).2 On the other hand, disseminated form of histoplasmosis in HIV-infected patients shows skin lesions in up to 85% of cases.1,8
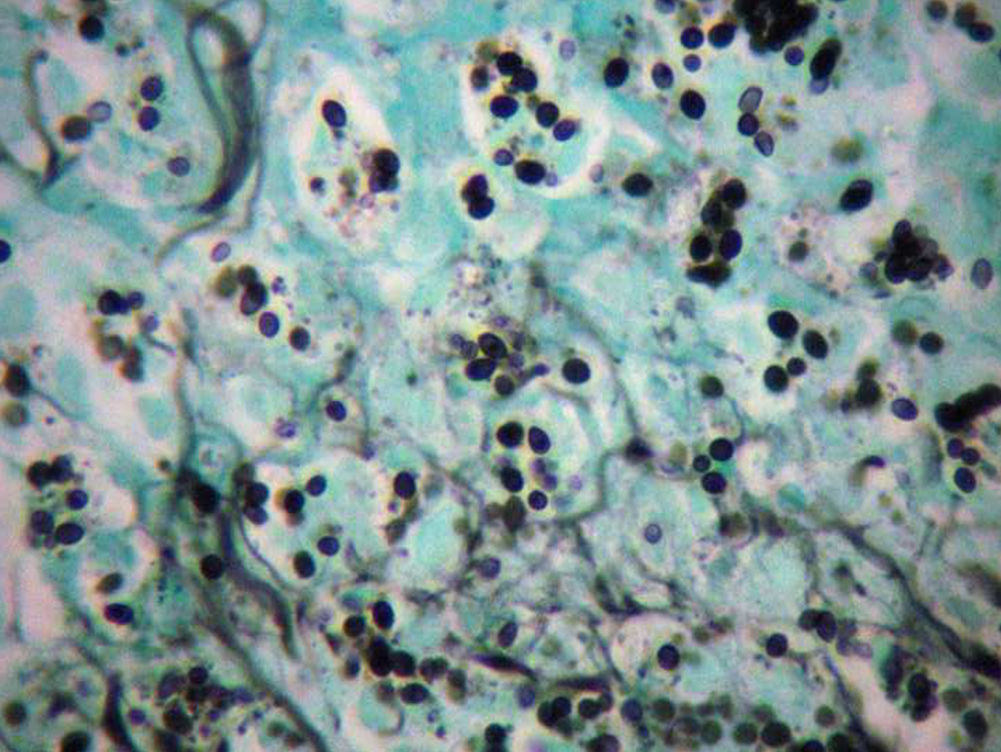
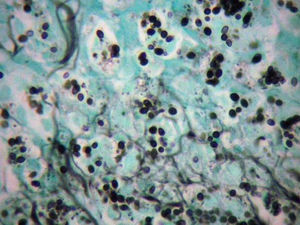
We report the case of a 73-year-old male patient with a 3-month history of genital lesion associated with weight loss and general complaints. The patient denied alcohol or tobacco consumption, and systemic hypertension was the only reported co-morbidity. On examination there were rare papules on the face, genital ulcers on the glans, foreskin and scrotum (Fig. 1), and two ulcerative lesions on the legs. A diffuse reticulonodular infiltrate was observed on the lungs on computed tomography. No visceromegaly or lymphadenomegaly were detected on abdomen investigation. Laboratory workout showed 12.7g/dl of hemoglobin as lone alteration. Albumin and globulins were in the normal range, as well as the CD4+ and CD8+ lymphocytes subpopulations. Serological tests for HIV, HBV and HBC were negative. Two skin biopsies from the genital area and from the leg showed a similar picture: ulcerative epidermis plus a lymphohistiocytic cell infiltration on the dermis with the cytoplasm of histiocytes plenty of microorganisms encircled by a clear halo. The Grocott-Gomori stain revealed fungal cells of small diameter on the cytoplasm, suggestive of Histoplasma capsulatum (Fig. 2). Despite the negative serologic results for histoplasmosis (double immunodiffusion), the hypothesis was confirmed through culture on Mycosel® and by thermal dimorphism. The patient was treated with itraconazol 400mg/day for two months followed by 200mg/day for additional two months, interrupted due to intolerance, with sustained clinical resolution after 18 months of follow-up.
Disseminated histoplasmosis is usually associated with immunosuppression, mostly caused by HIV infection.6,8 Patients under chemotherapy, following solid transplants or taking corticosteroids may also be affected. There are many differences between disseminated histoplasmosis if occurring in immunosuppressed patient or, in contrast, in immunocompetent individual. Immunosuppressed patients are more commonly male, and present co-morbidities, skin lesions, positive direct examination and positive culture, and less commonly positive serology.10 The clinical profile of our patient looked quite similar to the one observed among immunosuppressed patients. As there were no co-morbidities or poor nutritional status as an associated risk factor in this case, the patient's age could be considered as a predisposing factor by itself. Immunosenescence impairs the immune system of aged individuals leading to susceptibility to infections and reduced vaccine responses.4,5 The effects observed on immune system includes changes in CD4 T cells, CD8 T cells, regulatory T cells, reduced intracellular signaling capacities, reduced cell replicative ability and lower antibody production.4,5 These alterations are closely related to the increased mortality and morbidity rates observed in the elderly. Histoplasma capsulatum is an intracellular microorganism whose control depends on cell-mediated immunity and satisfactory macrophages functions. This very uncommon case seems to represent an additional example of possible immunosenescence leading to severe cutaneous-systemic fungal infection.