Historically first metatarsophlangeal joint fusion has been used to treat patients with joint arthritis or as a salvage procedure for iatrogenic deformities. For the past 20 years the author has used this procedure in older patients with hallux valgus deformity, and it has proven to be a safe and reliable technique. The paper describes the rationale for use of joint fusion as a primary option for hallux valgus repair in this patient population as opposed to other procedures. The surgical technique, fixation, and aftercare are also described.
Históricamente la fusión de la primera articulación metatarsofalángica ha sido una técnica quirúrgica usada para tratar pacientes con grado artrosis avanzada de la articulación o como un procedimiento de salvamento en deformidades iatrogénicas. El autor del presente trabajo ha utilizado este procedimiento durante los últimos 20 años en pacientes ancianos con deformidad en Hallux Valgus y se ha mostrado como un procedimiento seguro y fiable. El artículo describe el razonamiento para el uso de la fusión articular como primera opción en el tratamiento del Hallux Valgus en esta población de pacientes en vez de usar otro tipo de procedimientos. Se describe también la técnica quirúrgica, la fijación y los cuidados postoperatorios.
The repair of hallux valgus deformity in older patients may pose a more difficult problem for surgeons in comparison to the same condition in a younger population. The degree of hallux valgus deformity may be advanced, with a large intermetatarsal angle, fixed deformity, and the bone may be soft. While a proximal osteotomy or Lapidus may function well in a younger patient, in older patients the required non weight bearing associated with these procedures may create a hazard should the patient fall in the postoperative recuperation. In other circumstances where proximal procedures are performed the patient may weight bear postoperatively because they do not have the physical strength or balance to function on only one extremity. Therefore, a procedure which would provide sufficient correction of hallux valgus deformity and permit weight bearing in the postoperative interval would be a distinct advantage and safer for older patients. Many surgeons might consider a distal 1st metatarsal osteotomy even in a patient with a larger intermetatarsal angle or with greater levels of deformity. There are studies that have proven the efficacy of distal procedures in the repair of hallux valgus with large intermetatarsal angles, but the problem in the geriatric population is that the softer bone increases the risk of displacement or disruption of the osteotomy, or the failure to adequately correct the hallux valgus.
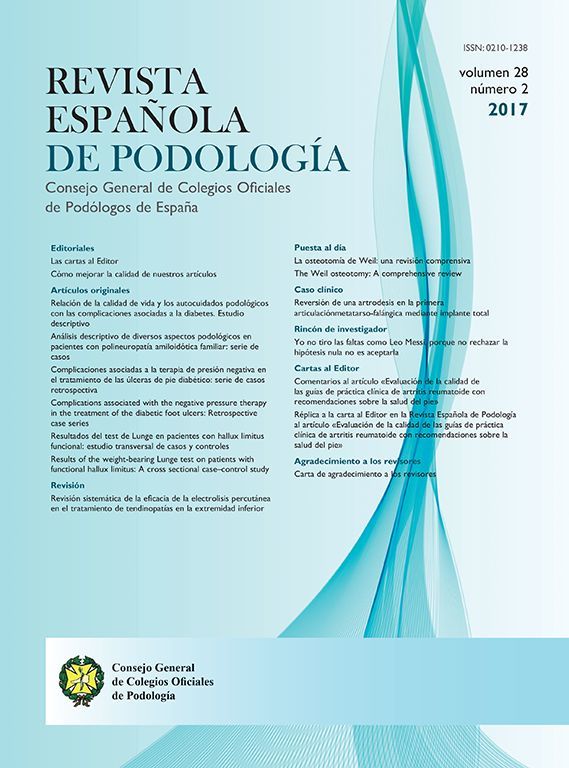
This “geriatric dilemma” lead the author to consider two procedures that for many years were considered somewhat antiquated – a modified Keller procedure and a first metatarsophalangeal joint fusion. For a number of years a modified Keller technique was employed by the author with success in patients with flexible hallux abducto valgus, but there were later patients that caused the author to revise the approach as it was felt the modified Keller would have been inadequate. The patient in Fig. 1 illustrates that dilemma. This was an older woman who had undergone previous removal of the lesser metatarsal heads as well as the proximal phalanges from the intermediate toes. A prior first MPJ fusion had been attempted, yet there was a nonunion. Her primary complaint was not pain relative to the nonunion, but that the additional length of the first ray created problems with balance and pain beneath the first metatarsal head.
Clearly, arthrodesis of the first metatarsophalangeal joint would be the preferred approach and would accomplish several goals – shortening of the first ray to provide better balance with weight-bearing, elimination of the nonunion, and improved stability to the forefoot as a whole. Due to the gross instability in the lesser rays, ultimately the hallux would tend to deviate laterally if a fusion was not performed. At the time that this patient was treated most surgeons believed that non-weight bearing for 6 weeks was necessary following first MPJ fusion. However, preoperatively she was unstable even with regular shoes. Therefore, the patient was permitted to walk with a surgical shoe after surgery, despite the fact that this was different than the protocols employed by most surgeons at that time. Fixation consisted of a linear Steinman pin with an oblique Kirschner wire, and the patient underwent successful arthrodesis and restoration of function despite weight-bearing throughout the postoperative recuperation. Given the success, the author began to consider this approach in other patients as well.
Surgical techniqueThe surgical approach is through a standard dorsomedial incision over the 1st metatarsophalangeal joint. However, the incision is extended distally to the interphalangeal joint of the hallux as this reduces tension on the medial skin with insertion of the distal K-wire for fixation. A linear dorsomedial capsular incision is made, followed by a vertical capsular incision medially at the level of the 1st mpj. The medial prominence of bone is removed and the joint deformity is evaluated. In some patients it is necessary to perform an interspace dissection and release the adductor hallucis tendon and other lateral joint contracture to allow adequate reduction of the phalanx on the metatarsal head without tension.
The author prefers to remove the cartilage from the first metatarsal head with a rongeur, and the cartilage from the base of the proximal phalanx with a curette. Thereafter, a power burr is used to remove any remaining segments of subchondral bone. In many geriatric patients, use of the rongeur is sufficient to remove the cartilage and subchondral bone to a satisfactory level on the metatarsal head. The subchondral plate on the base of the phalanx is thicker and the power burr is a good tool for ensuring that good raw bone is present on the distal side of the joint. Most surgeons tend to remove an insufficient amount from the base of the phalanx when they first start performing 1st mpj arthrodesis.
Once adequate bone surfaces are present on each side of the joint the two segments are approximated and additional remodeling with the power burr is employed until the bones fit together well. At this stage fixation of the fusion site commences, with a special focus on maintaining the alignment and position desired for fusion.
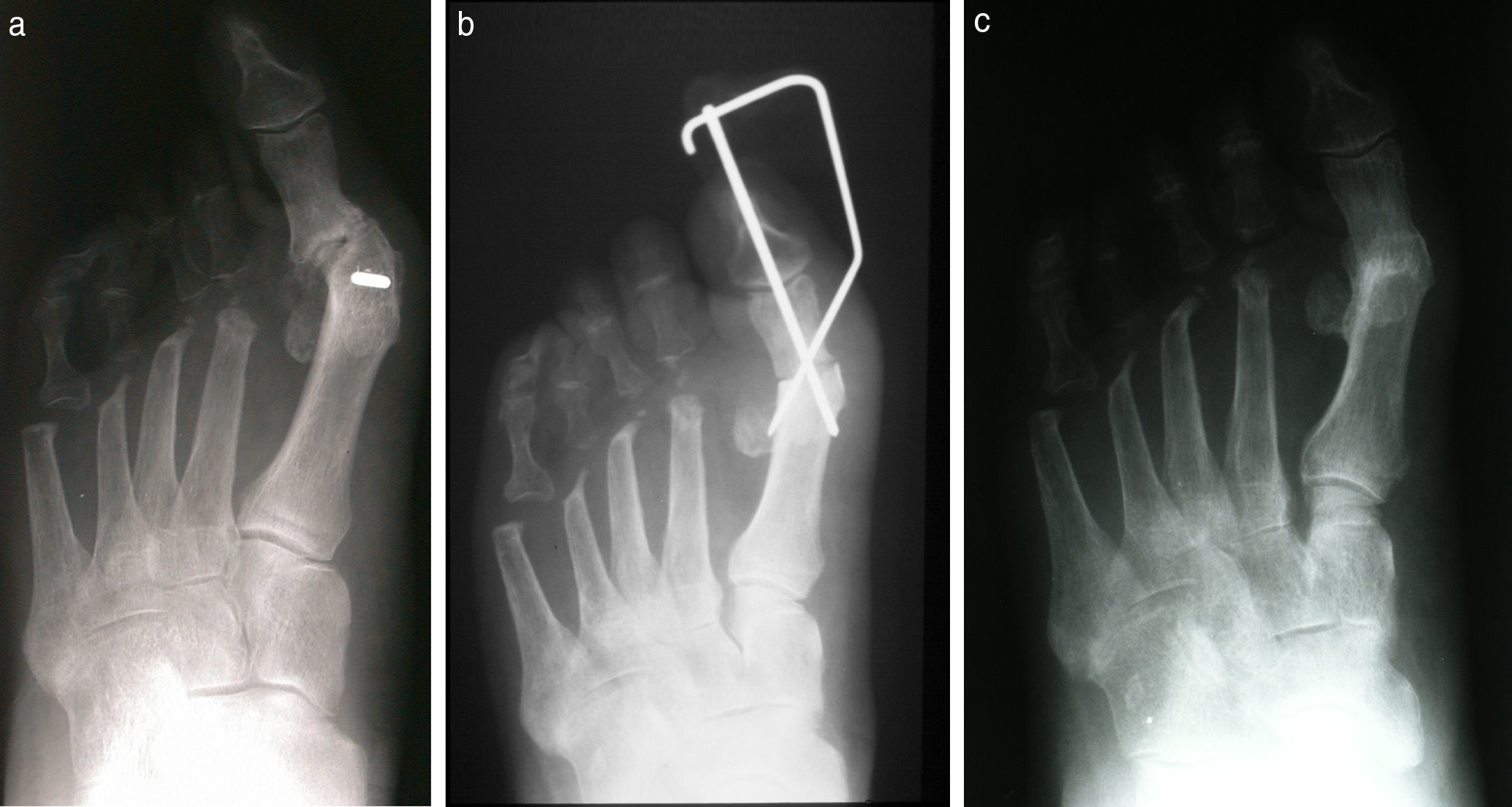
The author uses three 0.062in. Kirschner wires for stabilization of the first MPJ fusion in older patients.1 There are several different configurations which can be employed. For a number of years a linear wire extending from the tip of the toe into the first metatarsal was inserted for initial fixation and adjustment of alignment. Generally speaking, the other two wires were buried. In the past eight or ten years the preference has been to bury all of the wires whenever possible (Fig. 2). If none of the wires cross the hallux interphalangeal joint, the interphalangeal joint itself is able to absorb some of the weight-bearing forces or stresses during the recuperation interval until fusion occurs. In theory, this results in less potential for disruption of the fusion site.
(a) Preoperative clinical and (b) radiographic appearance of an older patient with hallux abducto valgus deformity and an overlapping 2nd toe. (c) Clinical and (d) radiographic appearance 6 months following surgery with arthrodesis of the first metatarsophalangeal joint and hammertoe repair. A partial 2nd metatarsal head resection was performed as well.
The first wire is typically inserted from the medial aspect of the base of the proximal phalanx and directed into the lateral aspect of the first metatarsal head. After this first wire is inserted a flat surface is used to assess the position of the first metatarsophalangeal joint. Typically one can take one of the metal boxes which contained the power equipment and place this on the plantar aspect of the foot to simulate weight-bearing. This is the best way to assess the position of the foot relative to the functional weight-bearing position postoperatively. The goal is to have the hallux rest a few millimeters above the weight-bearing surface with the interphalangeal joint in a neutral position. In addition, one can also assess the transverse plane alignment of the first MPJ to ensure adequate position in this plane. Radiographs are made in surgery at this point for confirmation of alignment, approximation of the fusion site, and alignment of the wire.
The second wire begins at the medial aspect of the first metatarsal head and is directed distally and laterally into the proximal phalanx. Once again, after the wire has been inserted the position of the hallux is reevaluated to ensure that the original alignment has not been disturbed. The third wire can be inserted in a number of different orientations. The author tends to place the third wire at the first metatarsal head either dorsally or dorsolateral with the wire exiting through the plantar cortex of the phalanx. The goal is to try and ensure that each wire crosses cortical bone on each side of the fusion site to provide the maximum stability. Radiographs are taken once again to verify that the wires are sufficiently aligned and of appropriate length.
The wires are then bent and cut and a lock pin technique is employed to complete the fixation. This technique was popularized by the late Gerard Yu, DPM, who used it for stabilization of the Austin osteotomy.2 However, the author has used this for a variety of surgical procedures with good results. In order to accomplish the lock technique the surgeon needs a good strong pair of pliers. After the wire has been bent and cut it is then rotated until it contacts the cortical surface of the bone. The wire is then turned a little further until the wire bends and locks on top of the cortex. This adds an additional level of stability to the fixation.
Following surgery the patient is allowed to fully weight bear with a padded surgical shoe. The author prefers to use a cork liner in the surgical shoe which extends from the heel to the level of the digital sulcus so that weight bearing does not apply direct pressure to the hallux. However, there are also a number of surgeons in the US who use a surgical shoe without modification, yet still allow patients to weight bear.
DiscussionThe author was not an early advocate for first metatarsophalangeal joint fusion as a primary technique for repair of hallux valgus or hallux limitus. For many years the podiatric community in the United States considered preservation of motion at the first metatarsophalangeal joint to be critical relative to normal foot function. This was one reason that 1st metatarsophalangeal implants were very popular in the United States, and there are still some surgeons who use implants in lieu of fusion of this joint. This author became disillusioned with implants early in his career, and for a period of time used a modified Keller technique for hallux limitus and hallux valgus in older patients. A modified Keller procedure may still be a reasonable consideration for patients in this age group. However, in patients with advanced hallux valgus, or, in circumstances with other specific concerns, fusion of the 1st mpj is reliable, provides excellent stability, and there is less shortening of the 1st ray as compared to a modified Keller procedure. Patients may also weight bear safely after 1st metatarsophalangeal fusion.1,3
While a full discussion of the modified Keller procedure is beyond the scope of this paper, the author feels that the key features of the modified approach should be mentioned as these steps overcome the complications and shortcomings of the traditional Keller procedure, and it is important for the reader to appreciate that these modifications are essential to restoration of function in the forefoot.4 In short, the only thing that the modified Keller and the traditional Keller have in common is the resection of the base of the proximal phalanx.
Modifications:
- -
Creation of a U-shaped capsular flap dissected from the medial aspect of the base of the phalanx and metatarsal head with the base proximal.
- -
Release of interspace contracture in cases of HAV.
- -
Resection of slightly less than 1/3 of the total length of the proximal phalanx.
- -
Suturing the flexor hallucis longus tendon into the base of the proximal phalanx after bone resection to restore flexor stability.
- -
Insertion of a 0.062in. Kirschner wire across the hallux and into the metatarsal with the toe in the corrected position. The wire is maintained for 6 weeks in patients with hallux valgus.
- -
Reattachment of the medial capsular flap into two holes at the medial aspect of the proximal phalanx.
- -
Transfer of the adductor hallucis tendon to the medial joint capsule in patients with hallux valgus.
The modified Keller may still be a reasonable alternative in patients with flexible and reducible hallux valgus, patients with hallux limitus or hallux valgus who would prefer to avoid a rigid joint, or where concerns about compliance with postoperative instructions may be a concern, such as in patients with some loss of memory or early dementia.
However, over time there have been patients who presented with conditions that seem to be better suited for fusion of the joint. Patients who are undergoing pan metatarsal head resection, or who have some pre-existing instability of the lesser rays, may have a greater tendency for recurrence of the hallux valgus. Fusion of the joint eliminates the potential for subsequent lateral deviation of the hallux. Patients who possess neurologic disease, such as Parkinson's, will be able to function and maintain correction with fusion as opposed to joint arthroplasty. Muscle imbalance may also be seen in some cases of hallux varus, and therefore, the preference of the author is to perform joint fusion in these patients as well. Patients who possess some degree of lesser metatarsal pain or iatrogenic deformities seem to do better with arthrodesis of the joint. While some degree of 1st ray flexibility is needed for reduction of deformity with a modified Keller procedure, a patient with a hypermobile 1st ray would tend to respond better with 1st mpj arthrodesis. The same would be true for a patient with a short 1st metatarsal. Fusion would appear to be preferred in patients with advanced metatarsus adductus since there is a high rate of recurrence when joint mobility is preserved. Finally, in some patients with recurrent hallux valgus there is a significant loss of bone from aggressive resection of the bunion that prevent adequate lateral transposition of the capital fragment with a distal or a Scarf osteotomy. Arthrodesis of the joint is the best option in many of these patients.
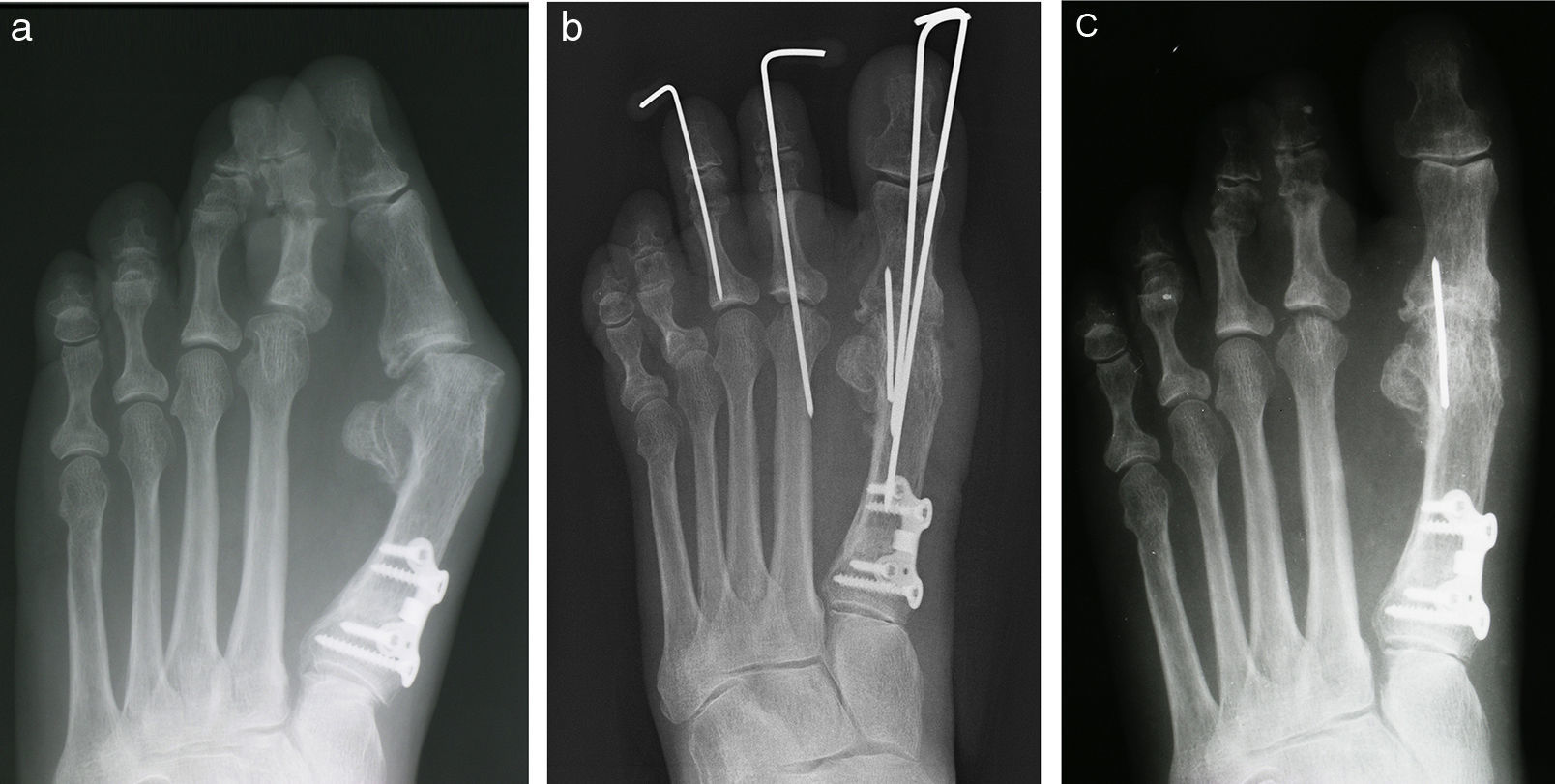
Another concern is when the surgeon must simultaneously address arthritis or deformity at the hallux interphalangeal joint. Fusion of both the metatarsophalangeal joint and the hallux interphalangeal joints in the same foot results in a very rigid structure that does not adapt readily to different surfaces in weight bearing. While an Akin procedure could be used to correct abduction of the toe distally and preserve the interphalangeal joint motion, this may limit the options of fixation for the arthrodesis of the metatarsophalangeal joint. In these settings the author prefers to perform an arthroplasty at the hallux interphalangeal joint, removing the bone from the distal aspect of the proximal phalanx needed to straighten the toe and reduce deformity. A linear wire is typically used to stabilize the interphalangeal arthroplasty for 6 weeks.
The question that is often posed is whether or not there is sufficient reduction of the intermetatarsal angle with a fusion of the first MPJ and without osteotomy or proximal procedure. Provided the first ray is flexible, reduction of the hallux valgus deformity and restoration of a rectus first metatarsophalangeal joint will reduce the intermetatarsal angle (Fig. 3).5–7 Patients with a rigid first ray will have a more limited reduction of the intermetatarsal angle.
(a) A patient with recurrent hallux valgus deformity with a large intermetatarsal angle. (b) Immediate postoperative appearance and (c) 3 months postoperative. Notice the reduction in the intermetatarsal angle despite the fact that no osteotomy was performed as part of the revisional surgery.
The surgeon has a large number of options for fixation with 1st mpj fusion. Wires provide the most economical choice, and the stability achieved with 3 Kirschner wires is impressive. The rate of healing for patients who are weight-bearing following first MPJ fusion are equivalent to patients who are nonweightbearing. The form of fixation does not seem to make any difference relative to healing rates.1,3 The use of three Kirschner wires is a simple and cost-effective technique and does not create a large bulky mass of fixation that can be seen in some plate systems. Furthermore, the mass of a plate also makes assessment of joint fusion more difficult as it obscures visualization of the surgical site on radiographs. The Kirschner wires can be easily removed in the office under local anesthesia if required at a later time.
ComplicationsFollowing any joint fusion nonunion may be encountered, but fortunately the rate of nonunion with this technique has been equivalent to the rate of nonunion in patients regardless as to the form of fixation, and in patients who have been maintained non weight bearing after surgery. However, the responses of patients with nonunion using the 3 wire fixation technique have been quite interesting. It has been the author's experience that patients who develop a nonunion generally function well and asymptomatically once the K wires are removed. Instead of attempting to perform a revisional fusion, the first step following nonunion may be to simply remove any residual fixation. It would appear that the interference of motion created by the fixation is the primary source of pain as opposed to the nonunion itself.8 Interestingly, the reduction of hallux valgus deformity is largely preserved in most patients with nonunion (Fig. 4).
(a and b) Preoperative appearance of a patient with hallux varus and arthritic changes at the hallux interphalangeal joint. (c) Immediate postop films after 1st mpj fusion and hallux interphalangeal arthroplasty. (d and e) Clinical and radiographic appearance 6 months postoperatively with a nonunion of the 1st mpj. (f and g) Clinical and radiographic appearance of the foot 6 months after the removal of the wires with an asymptomatic nonunion.
Otherwise, there have been only a few patients where removal of a buried wire has been needed postoperatively, and this has been secondary to direct shoe irritation. Typically this occurs with the dorsal or medial wire at the level of the first metatarsal.
ConclusionArthrodesis of the 1st mpj is a very useful technique for the repair of hallux valgus deformity in the older patient. It is a simple technique with good outcomes and poses limited risk to this group of patients. Fixation with Kirschner wires is a simple, stable, effective, and economical form of fixation with healing rates equivalent to other methods of stabilization.
Financial disclosureNone declared.
Conflicts of InterestAuthor declare no potential conflicts of interest.