Extracapsular hip fractures in patients over 85 years old represent a therapeutic challenge due to their high vulnerability and risk of complications. This study analyzes the efficacy and safety of bipolar hip arthroplasty with uncemented femoral stems in this population.
Materials and methodsA retrospective study was conducted at three referral hospitals, including 63 patients over 85 years old treated between 2019 and 2023. Clinical, radiological, and functional variables were evaluated with a minimum follow-up of 12 months. Hip function was assessed using the Harris Hip Score (HHS).
ResultsThe mean age was 86.7 years, with a female predominance (63.5%). The average surgical time was 46±7min, and intraoperative blood loss was 220±40ml. The complication rate was low: 14.2% experienced mild hypotension, 1.6% suffered a periprosthetic fracture, and isolated cases of postoperative hyperglycemia and hypoalbuminemia were promptly resolved. The mean HHS was 79±8 points at 6 months and 81±6 points at 12 months. A total of 71.4% of patients regained their pre-injury ambulatory status. No significant prosthetic subsidence or femoral pain was observed.
ConclusionBipolar hip arthroplasty with uncemented femoral stems appears to be a safe and effective option for treating extracapsular hip fractures in patients over 85 years old, allowing early rehabilitation and reducing complications associated with cementation and osteosynthesis.
Las fracturas extracapsulares de cadera en los pacientes mayores de 85 años representan un desafío terapéutico debido a su alta vulnerabilidad y riesgo de complicaciones. Este estudio analiza la eficacia y la seguridad de la artroplastia bipolar de cadera con vástagos femorales no cementados en esta población.
Materiales y métodosSe realizó un estudio retrospectivo en 3 hospitales de referencia, incluyendo 63 pacientes mayores de 85 años tratados entre 2019 y 2023. Se evaluaron variables clínicas, radiológicas y funcionales con un seguimiento mínimo de 12 meses. La función de la cadera se valoró mediante el Harris Hip Score (HHS).
ResultadosLa edad promedio fue de 86,7 años, con un predominio femenino (63,5%). El tiempo quirúrgico promedio fue de 46±7min y la pérdida sanguínea intraoperatoria fue de 220±40ml. La tasa de complicaciones fue baja: 14,2% presentó hipotensión leve, 1,6% fractura periprotésica, y se registraron casos aislados de hiperglucemia posquirúrgica e hipoalbuminemia, ambos resueltos favorablemente. El puntaje HHS promedio fue de 79±8 puntos a los 6 meses y 81±6 puntos a los 12 meses. El 71,4% de los pacientes recuperaron su capacidad ambulatoria previa. No se observaron hundimientos protésicos significativos ni dolor femoral.
ConclusiónLa artroplastia bipolar con vástagos no cementados de fijación distal es una alternativa segura y eficaz para el tratamiento de fracturas extracapsulares de cadera en los pacientes mayores de 85 años, permitiendo rehabilitación temprana y reduciendo las complicaciones asociadas a la cementación y a la osteosíntesis.
Hip fractures in patients over 85 years of age present a significant challenge for orthopaedic surgeons due to the complexity of treatment and the complications associated with conventional therapeutic options. Historically, osteosynthesis and cemented partial hip arthroplasty have been the predominant approaches in this population.1 However, both techniques have significant limitations that can affect the recovery and prognosis of elderly patients.2
Osteosynthesis, although widely used, can be associated with prolonged postoperative immobility, increasing the risk of medical complications and functional decline in this group of frail patients.3 On the other hand, cemented partial hip arthroplasty, while providing immediate fracture stabilisation, carries the risk of developing cement implantation syndrome, a potentially serious complication that can have devastating consequences in geriatric patients.
In this context, bipolar hip arthroplasty using uncemented femoral stems for diaphyseal fixation has emerged as an innovative and promising alternative for managing extracapsular hip fractures in patients over 85 years of age. This technique combines the benefits of mechanical stability provided by total hip arthroplasty with the preservation of bone structure characteristic of partial arthroplasty, without the risks associated with the use of bone cement.
In this study, we explored the efficacy and safety of bipolar hip arthroplasty with uncemented femoral stems in geriatric patients with extracapsular hip fractures, analysing short-term clinical, functional, and radiological outcomes. Furthermore, we discussed the clinical implications and important considerations in selecting this surgical technique for the elderly population, with the aim of improving the care and management of this challenging orthopaedic condition.
Materials and methodsStudy designA retrospective, multicentre study was conducted at three referral hospitals, including patients over 85 years of age with extracapsular hip fractures treated with bipolar arthroplasty using uncemented femoral stems, between June 2019 and October 2023. Clinical, radiological, and functional data were collected, ensuring a minimum follow-up of one year.
Data collection processData collection was performed through a systematic review of electronic and physical medical records from each institution. To minimise recording errors, data were extracted by two independent researchers and subsequently verified by a third reviewer. A centralised and anonymised database was created to preserve patient confidentiality.
The variables collected included:
- •
Demographic data (age, sex).
- •
Fracture characteristics (Boyd and Gryphon classification).
- •
Surgical details (time in surgery, type of prosthesis, blood loss).
- •
Perioperative and postoperative complications.
- •
Time to ambulation.
- •
Functional assessments using the Harris Hip Score (HHS).
- •
Radiographic findings (component alignment, depression osteointegration).
To reduce selection bias, all patients who met the inclusion criteria during the study period were consecutively included. No exclusions based on clinical outcomes were applied. Interinstitutional variability was controlled using standardised surgical protocols and common postoperative management guidelines at both sites. Radiographic evaluation was performed independently by two radiologists, and in case of discrepancy, a consensus was reached through joint review.
Patient selectionThe inclusion criteria were:
- •
Extracapsular intertrochanteric hip fracture.
- •
Aged 85 or older.
- •
Previous ability to walk independently or with assistance (Koval I–V).
Additionally, patients’ cognitive ability and prior functional status were assessed using geriatric assessment records at admission. Patients with active infections, severe uncompensated metabolic disorders, severe cognitive impairment that would prevent active rehabilitation, or fractures associated with bone tumours were excluded.
The decision to opt for uncemented bipolar arthroplasty was made by the surgical team in consultation with the interdisciplinary geriatric team, prioritising risk-benefit criteria for each patient.
Study populationAll patients over 85 years of age with surgically treated extracapsular hip fractures during the study period were consecutively selected. The Boyd and Gryphon classification was used to evaluate the fracture pattern. Twenty-four patients presented with type I fractures, 32 patients with type II fractures, and 7 with type III fractures. The proximal femur geometry corresponded to Dorr type B (28 cases) and Dorr type C (35 cases).
Surgical procedureAll patients underwent bipolar hip arthroplasty using a standardised surgical technique. Preoperative planning was performed following the guidelines of Ranco-Ferrando et al.4 All patients received standard intravenous antibiotic prophylaxis with 1g of cefazolin (2g if the patient's weight exceeded 70kg), administered in three doses every 8h. Additionally, all patients received 1g of tranexamic acid before surgery, except for three patients with a history of thromboembolic disease. The surgical approach was posterolateral.
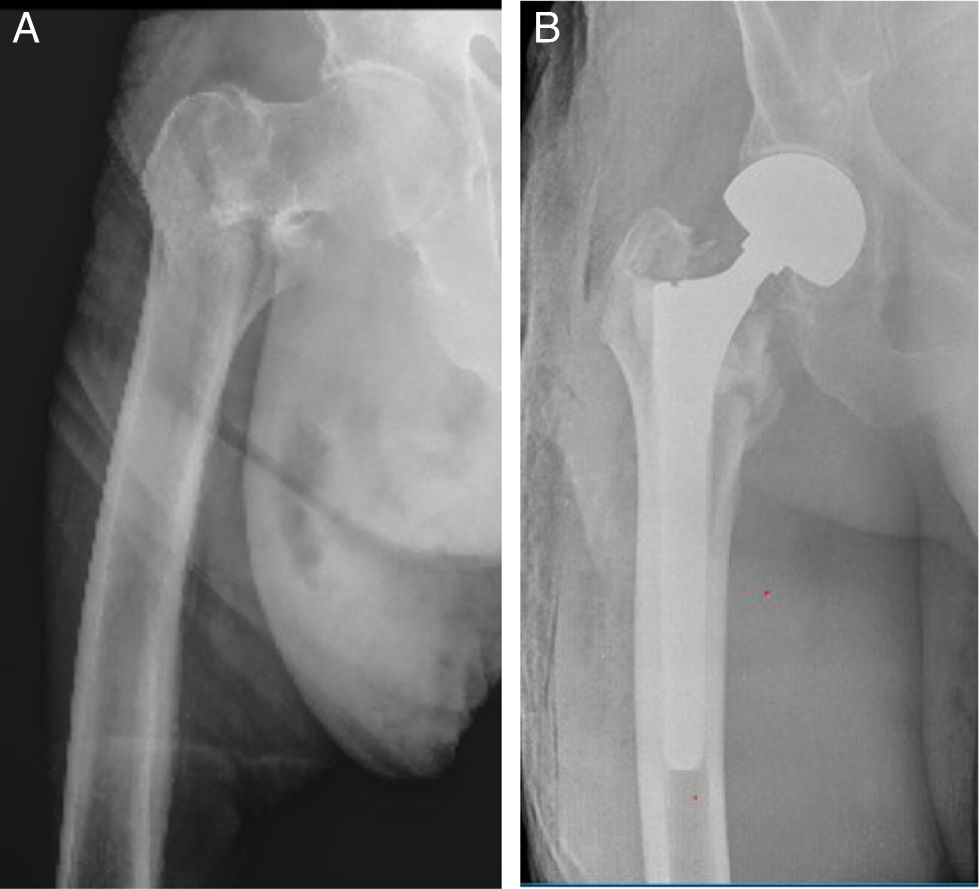
A non-cemented, tapered, grooved femoral stem was used for distal fixation, selected according to the patient's anatomical characteristics and bone quality. The stem used in this study, MD6® (Vincula, Rio Claro, Brazil), is made of titanium alloy and has a highly textured surface along its entire length. The stem features eight longitudinal grooves with relatively sharp edges designed to achieve effective anchorage with the femoral cortex (Fig. 1). The average stem length was 180mm, and in all cases, a 28mm femoral head was used along with a bipolar acetabular component. The femoral canal was always reamed manually.
Lower limb length was measured by direct palpation. The patient's pelvis was positioned vertically by palpating and aligning both iliac crests in the same vertical plane. The operated leg was placed on top of the contralateral leg at the same abduction angle, and both heels were aligned. Subsequently, the poles of the patellae were palpated to verify the length of the lower limbs.
It is important to note that our standard method for assessing adequate lower limb length in total hip arthroplasty involves measuring the distance from the lesser trochanter to the bisector of the ischial tuberosities. However, in the context of extracapsular fractures, this anatomical landmark is lost, rendering it unusable. Direct intraoperative comparison between both limbs is not the most reliable method and is generally associated with a higher proportion of discrepancies in lower limb length.
Statistical analysisA descriptive analysis of the collected data was performed. Continuous variables were expressed as mean±standard deviation or median (interquartile range) depending on the distribution. Categorical variables were reported as absolute frequencies and percentages.
Informed consent was obtained from all patients included in the study, or from their legal representatives, in accordance with the ethical principles of the Declaration of Helsinki.
ResultsPopulation descriptionSixty-three patients were included in the study, with a mean age of 86.7 years (range: 85–94 years). The gender distribution was: 40 women (63.5%) and 23 men (36.5%).
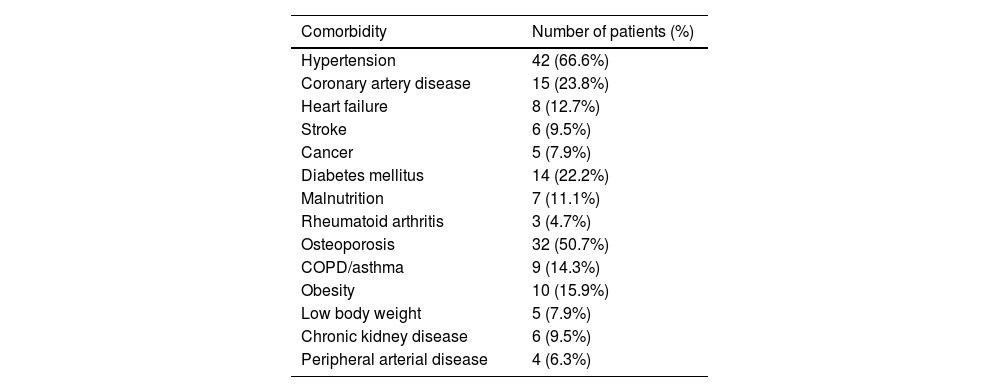
All patients had at least one comorbidity. The observed comorbidities are detailed in Table 1.
Patient comorbidities.
| Comorbidity | Number of patients (%) |
|---|---|
| Hypertension | 42 (66.6%) |
| Coronary artery disease | 15 (23.8%) |
| Heart failure | 8 (12.7%) |
| Stroke | 6 (9.5%) |
| Cancer | 5 (7.9%) |
| Diabetes mellitus | 14 (22.2%) |
| Malnutrition | 7 (11.1%) |
| Rheumatoid arthritis | 3 (4.7%) |
| Osteoporosis | 32 (50.7%) |
| COPD/asthma | 9 (14.3%) |
| Obesity | 10 (15.9%) |
| Low body weight | 5 (7.9%) |
| Chronic kidney disease | 6 (9.5%) |
| Peripheral arterial disease | 4 (6.3%) |
The average surgical time was 46±7min, and the average intraoperative blood loss was 220±40ml. Three patients (4.7%) experienced more significant blood loss requiring blood transfusion, attributed to a history of thromboembolic disease; tranexamic acid was not administered to these patients.
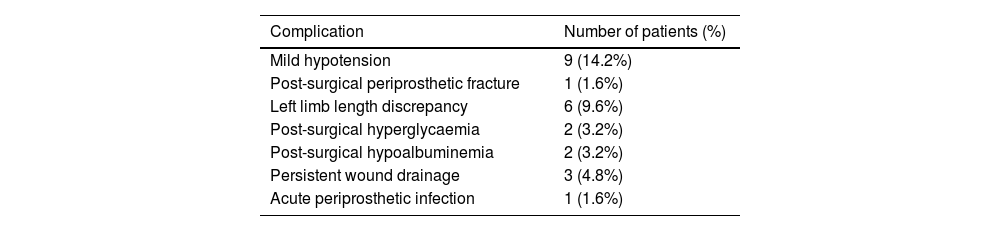
Clinical and functional resultsPerioperative and postoperative complications- •
Nine patients (14.2%) required vasoactive drug infusions for mild hypotension.
- •
One patient (1.6%) suffered a periprosthetic fracture secondary to a fall from standing height three months postoperatively, which resolved with rest.
- •
Six patients (9.6%) presented with lower limb length discrepancy, which did not exceed 5mm in any case and was not associated with clinical symptoms.
- •
Two patients (3.2%) developed postoperative hyperglycaemia, successfully controlled with adjustment of the insulin regimen.
- •
Two patients (3.2%) presented with mild hypoalbuminemia, corrected with nutritional support during hospitalisation.
- •
Three patients (4.8%) presented with persistent surgical wound drainage; in all cases, the anticoagulant regimen was modified, discontinuing low-molecular-weight heparin and administering acetylsalicylic acid 325mg/day.
- •
One patient (1.6%) presented with acute periprosthetic infection diagnosed according to the criteria of the second Consensus on Periprosthetic Infections (CPI). The patient had two phenotypically identical positive cultures in two synovial fluid samples obtained from ultrasound-guided arthrocentesis prior to surgery (major ICM criterion).5 The patient required a debridement procedure, irrigation, replacement of modular components, and antibiotic therapy, successfully controlling the acute infection (Table 2).
Table 2.Observed complications.
Complication Number of patients (%) Mild hypotension 9 (14.2%) Post-surgical periprosthetic fracture 1 (1.6%) Left limb length discrepancy 6 (9.6%) Post-surgical hyperglycaemia 2 (3.2%) Post-surgical hypoalbuminemia 2 (3.2%) Persistent wound drainage 3 (4.8%) Acute periprosthetic infection 1 (1.6%) - •
No deaths were recorded during hospitalisation. One patient died in the first postoperative month (1.58%). The one-year mortality rate was 9.52% (6 patients).
No iatrogenic fractures occurred during the surgical procedure.
Postoperative rehabilitationRehabilitation began on the same day as surgery with lower limb exercises. Patients were able to sit up in bed at 24h and began partial weight-bearing ambulation over 3 weeks, assisted by a walker at 48h postoperatively.
Functional assessmentHip function was assessed using the Harris Hip Score (HHS):
- •
Average score at 6 months: 79±8 points.
- •
Average score at 12 months: 81±6 points.
Ambulation ability was assessed using the Koval categories6:
- •
Forty-five patients (71.4%) recovered their pre-fracture ambulation status.
- •
Eighteen patients (28.6%) experienced a one-level decline in their ambulation category.
Component alignment was adequate in all cases (Fig. 2). Diaphyseal osseointegration was evident on follow-up radiographs at 6 months post-surgery. The radiographic criteria of Engh et al.7 were followed for evaluating the fixation of uncemented femoral stems, assessing the absence of peri-implant radiolucent lines in Gruen zones 2, 3, 4, 5, and 6, signs of bone remodelling around the stem, and confirming implant stability one year after the procedure. No subsidence greater than 5mm was observed, and no femoral pain was reported in any of the patients.
DiscussionThe results of this study demonstrate that bipolar hip arthroplasty with uncemented femoral stems is an effective and safe option for the treatment of extracapsular hip fractures in patients over 85 years of age. The adequate osseointegration of the components, the absence of severe complications, and satisfactory functionality indicate that this surgical approach is safe and beneficial for this age group.
Our findings are consistent with the conclusions of Kim et al., who note that uncemented primary hip replacement is a generally accepted indication for intertrochanteric fractures with extensive comminution and poor bone quality, which preclude open reduction and internal fixation.8 The choice of arthroplasty in our study allowed patients to bear weight and begin rehabilitation early, without worrying about complications such as malunion, nonunion, or osteonecrosis. In a study of 230 patients, Iosifidis et al. found that early ambulation after a hip fracture was the most important predictor of long-term survival.9
Cemented partial hip arthroplasty and osteosynthesis are therapeutic options with advantages and disadvantages for treating these fractures in elderly patients. Cementing the femoral canal can trigger “cement implantation syndrome,” a major cause of morbidity and mortality in these patients.10,11 This syndrome, of embolic origin and associated with the cementation process, is characterised by hypotension, hypoxia, loss of consciousness, pulmonary hypertension, right ventricular failure, arrhythmias, and, eventually, cardiac arrest. Donaldson et al.12 distinguish three grades of this syndrome according to the severity of the event:
- •
Grade 1: Oxygen saturation decrease<94% or hypotension<20% of the preoperative value.
- •
Grade 2: Oxygen saturation decrease<88%, hypotension<40% of the preoperative level, and/or loss of consciousness.
- •
Grade 3: Cardiovascular collapse.
The overall incidence is 25%–30% (Grade 1: 21%, Grade 2: 5.1%, Grade 3: 1.7%). Extracapsular hip fracture and the use of long femoral stems are predisposing factors. Intraoperative mortality in cemented hemiarthroplasties ranges from .2% to 4.3%, while at 30 days it rises to 9% and at one year to 29%.13
Several studies have reported complications associated with osteosynthesis using sliding screws or cephalomedullary nails in intertrochanteric fractures, such as loss of reduction and femoral shortening. Haentjens et al. also highlighted a higher incidence of pneumonia and pressure ulcers in patients with internal fixation, possibly related to early weight-bearing restriction.14
Sniderman et al., in a comparative study of 150 patients, observed that hemiarthroplasty allowed for earlier mobilisation, less blood loss, and lower reintervention rates compared to open and internal fixation (ORIF). Although they reported more cases of trochanteric displacement, this did not affect functional outcomes.15
Dündar et al., in a study of 132 elderly patients (mean: 89.4 years), found that both uncemented hemiarthroplasty with a long stem and proximal femoral nailing were effective, although they highlighted the advantage of hemiarthroplasty in terms of early mobilisation and less postoperative dependence.16
Similarly, Çiloğlu et al. and Çelen et al. reported lower complication rates, lower mortality, and lower prosthetic failure rates in the groups treated with uncemented hemiarthroplasty compared to those treated with proximal femoral nails.17,18 Finally, Agar et al. concluded that both surgical methods offer satisfactory functional results in elderly patients with unstable fractures.19
Conversion to arthroplasty after osteosynthesis failure is complex and has uncertain outcomes, whereas prosthetic replacement in our study effectively restored hip mechanics and eliminated the risk of future complications, such as malunion, nonunion, and avascular necrosis.
If prosthetic replacement is chosen for an intertrochanteric fracture, an uncemented femoral stem with distal fixation is preferred due to calcar deficiency, given the lower risk of cardiopulmonary complications related to bone cement in elderly patients.5 Yoo et al. conducted a meta-analysis and systematic review comparing cemented versus uncemented bipolar hemiarthroplasty in elderly patients with unstable intertrochanteric fractures. A higher incidence of lower limb length discrepancies (>1cm) was observed in the cemented group, suggesting a lower rate of prosthetic subsidence in uncemented hemiarthroplasties.20 Cankaya et al. evaluated the reliability of cemented versus uncemented hemiarthroplasty in 86 elderly patients with unstable intertrochanteric fractures. Cementless hemiarthroplasty proved to be a safe option, with early mobilisation, satisfactory functional outcomes, shorter surgical times, less blood loss, and lower perioperative mortality. No implant loosening, osteolysis, greater trochanter pseudoarthrosis, or cases of prosthetic instability or subsidence were observed.21 Park et al. concluded that the clinical results and mechanical stability achieved with this distal fixation and splined design are comparable to or even superior to other uncemented stem designs in femoral revisions for proximal femoral deficiency.22
Regarding fixation of the posteromedial fragment or the greater trochanter, Chu et al. reported that, when treating unstable intertrochanteric fractures with splinted, tapered monoblock stems, all fractures in the trochanteric region healed adequately, regardless of fragment fixation.23 Similar results were described by Zha et al.,24 and Kang et al. Excellent clinical and radiographic results were achieved by performing bipolar hemiarthroplasties using uncemented distal fixation stems in osteoporotic femoral neck fractures in patients with Dorr type B and C25 femurs.
This surgical treatment not only demonstrated a low rate of perioperative complications but also a low rate of complications in the medium-term follow-up, allowing for safer and more sustained rehabilitation in highly frail patients.16,26–29 The choice of a technique that promotes osseointegration and avoids the complications associated with cement and osteosynthesis represents a significant advance in improving functional outcomes and reducing morbidity and mortality in this age group.
Strengths and limitations of the studyStrengths of the study include the well-defined target population, the reasonable sample size for this type of population, the standardised surgical protocol, documented early rehabilitation, objective outcome assessments, and carefully recorded postoperative complications. Limitations include the retrospective design, the absence of a control group, the lack of randomisation (all patients were treated with the same technique without randomisation, preventing control for unmeasured confounding factors), and the relatively short follow-up period.
ConclusionThe results of this study suggest that bipolar hip arthroplasty with uncemented femoral stems is a viable and safe option for patients over 85 years of age with extracapsular hip fractures. This technique allows for early rehabilitation and reduces the risk of complications associated with cementation and osteosynthesis.
Level of evidenceLevel of evidence iv.
Informed consentInformed consent was obtained despite the retrospective nature of the study.
Ethical approvalThe study was conducted retrospectively and approved by our institution's Ethics Committee. All procedures performed in studies involving human participants were carried out in accordance with our institution's ethical standards and the 1964 Declaration of Helsinki and its subsequent amendments or comparable ethical standards.
Statement on the use of generative AI and AI-assisted technologies in the writing processThe author(s) used Chat GPT during the preparation of this study to improve readability and language. After using this tool, the author(s) reviewed and edited the content as needed and assume full responsibility for the content of the publication.
FundingNone.
Conflict of interestsNone.
Javier Pizarro.
Andrés Scarcella.