Spinal metastases are a very common problem which dramatically affects the quality of life of cancer patients. The objective of this review is to address the issue of how minimally invasive surgery can play an important role in treating this pathology.
MethodsA literature review was performed, searching in the Google Scholar, PubMed, Scopus and Cochrane databases. Relevant and quality papers published within the last 10 years were included in the review.
ResultsAfter screening the 2184 initially identified registers, a total of 24 articles were included for review.
ConclusionMinimally invasive spine surgery is specially convenient for fragile cancer patients with spinal metastases, because of its reduced comorbidity compared to conventional open surgery. Technological advances in surgery, such as navigation and robotics, improve accuracy and safety in this technique.
Las metástasis vertebrales son un problema muy frecuente y asocian un deterioro importante de la calidad de vida en los pacientes oncológicos. El objetivo de esta revisión es determinar el encaje de las técnicas quirúrgicas mínimamente invasivas dentro del manejo de esta entidad.
MétodosSe realizó una revisión bibliográfica en las bases de datos Google Scholar, PubMed, Scopus y Cochrane. Se revisaron los artículos publicados en los últimos 10 años que fueran de una relevancia y calidad adecuadas.
ResultadosTras el cribado de los 2.184 trabajos identificados inicialmente en las distintas bases de datos, se incluyeron un total de 24 artículos en esta revisión.
ConclusiónLa cirugía mínimamente invasiva de columna es especialmente útil en pacientes oncológicos frágiles con metástasis vertebrales por la reducida comorbilidad que presentan las técnicas que se engloban en ella en comparación con la de la cirugía abierta convencional. Los avances en tecnología aplicada a la cirugía, como la navegación y la robótica, mejoran la precisión y reducen las complicaciones de esta técnica.
Bones are the most frequent site of metastasis and the spine is the most affected bony region: the spine alone is the third anatomical site most commonly affected by metastasis, after the lung and the liver.1 On rare occasions, surgery of a spine metastasis may aspire to become part of a curative treatment, when there is a single tumour associated with a primary tumour that is also resectable.2 In the remainder of cases, which is the great majority, our role as surgeons in the management of this condition is mainly pain relief and an improvement in the quality of life in cancer patients with disseminated cancer undergoing palliative care. For this reason, minimally invasive spine surgery techniques (known by their acronym MISS) are a fundamental alternative in treatment.3 The purpose of this review is to define the role of MISS and other associated techniques in the treatment of patients with vertebral metastasis.
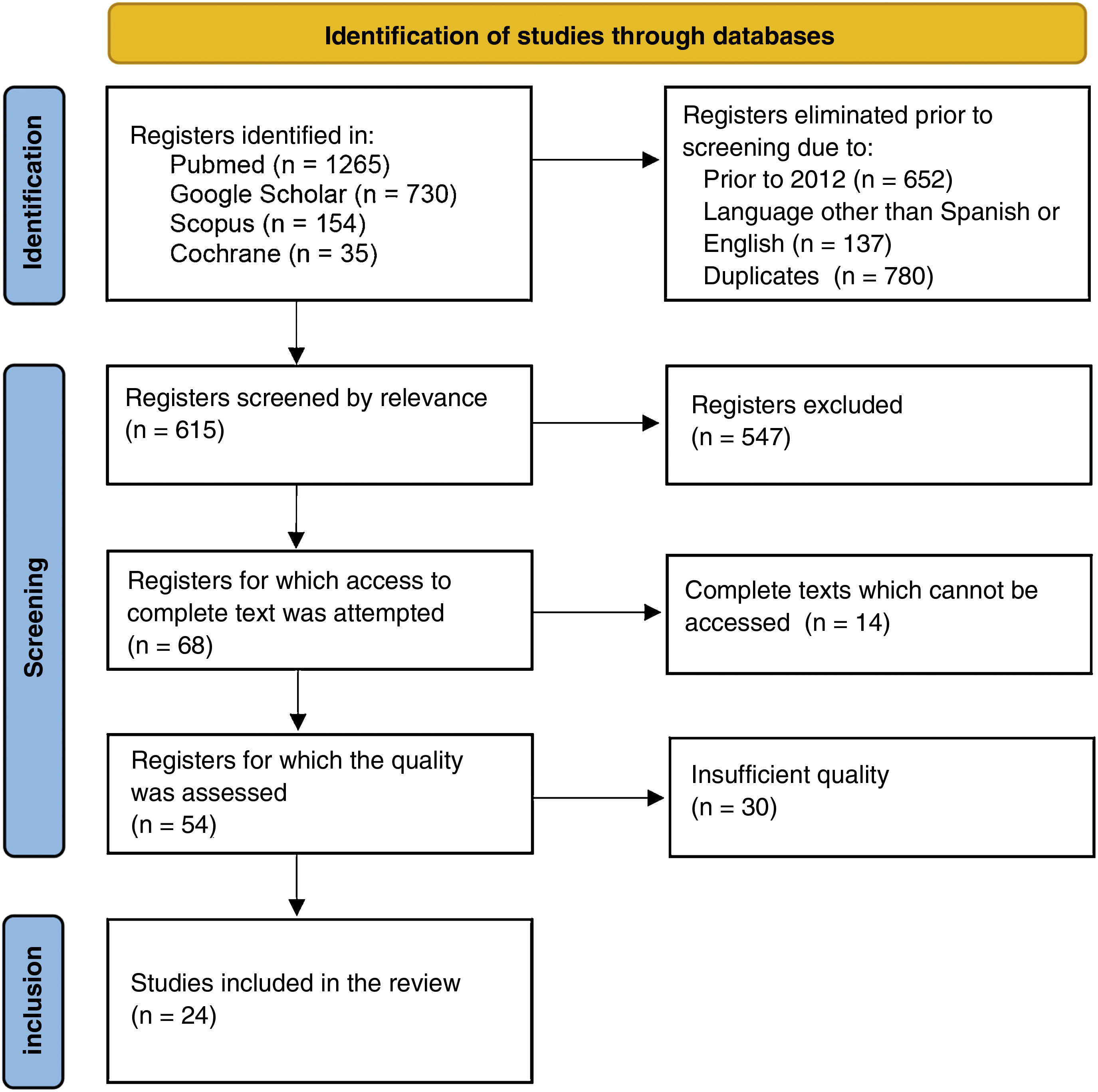
Material and methodsA review in the databases of Google Scholar, PubMed, Scopus and the Cochrane Library in November 2022 was made to identify all scientific papers addressing the treatment of vertebral metastases by minimally invasive surgery. The search parameter used was: (minimally invasive OR minimally invasive surgery OR minimally invasive spine surgery OR minimal access OR mini-open) AND (vertebral metasta* OR spinal metasta* OR metastatic spine OR metastatic vertebra*) NOT case report. The resulting papers were included if they had been published within the last 10 years and the text was available in English or Spanish. Two independent reviewers filtered these papers according to their titles and abstracts to discard those irrelevant to the topic under review and accessed the full text of the selected studies. Only those studies that met the quality standard of evidence proposed by the Centre for Evidence Based Medicine (CEBM) of the University of Oxford4 were used to write this review.
ResultsThe initial bibliographic search found a total of 2184 articles among the databases consulted. This dropped to 1395 registers when only works in Spanish or English in the last 10 years were included. Once the duplicates had been eliminated, the articles screened for relevance and their evidence assessed for quality a total of 24 studies for review were selected (Fig. 1).
DiscussionThe treatment of spine metastases is mainly conditioned by the combination of the patient's disease stage and the severity of their symptoms.5 In addition, the willingness of patients to accept intensive treatment is multifactorial and complex.6,7 It is essential that the treatment options proposed to these patients reflect respect for their decision-making autonomy and include the alternatives that best fit their preferences in terms of how they want to manage their disease.7 The quality of life of cancer patients in advanced stages of the disease can be severely conditioned by spinal metastatic involvement, so appropriate management is key in these delicate moments of life, forgetting the curative treatment approach and seeking to improve quality of life for as long as posible.8
MISS has developed over the last few decades and has become a comparable alternative to open procedures for the management of spinal instability and spinal cord compression in patients with metastatic spinal disease.9
The survival of patients with vertebral metastases is around 20% at 2 years.10 This survival is not determined by the vertebral extent of the disease and the procedures that can be performed on these metastatic implants are not curative, but are aimed at maintaining or improving quality of life.5,11,12 Most published studies have proposed that surgery should be considered in patients with a life expectancy of more than 3–6 months.11,13–15
Metastatic spinal lesions may present with different symptoms, mainly pain, fractures and neurological impairments derived from spinal cord compression.16 Spinal cord compression may present in up to 14% of patients with metastatic spinal disease and generally lead to untreatable pain which affects mobility and sphincter continence.14 Pain relief and the relief of neurological complications may be achieved through surgery, radiation or both, thereby increasing the patient's quality of life.15,17 The best results of surgery in combination with radiotherapy or surgery alone compared with radiotherapy alone have been supported by numerous studies17 and, surgery has consequently become a standard for all patients with symptomatic vertebral metastasis.
Overall, both MISS procedures and open surgery provide similar pain reduction. However, numerous studies have supported the claim that MISS approaches have overall clinical outcomes that are equal or somewhat more favourable.18 These techniques have less intraoperative bleeding, which is beneficial in terms of not destabilising these fragile patients and improving their postoperative outcomes, as less anaemisation results in fewer transfusions and shorter in-hospital stay after surgery.19 A systematic review by Pennington et al. supports these findings in relation to reduced blood loss and shorter hospital stay20: despite heterogeneity between studies, a shorter hospital stay was found in patients treated with MISS compared to those undergoing open surgery (8.7 vs. 14.7 days).
Another advantage of MISS is its role in reducing surgical site infection. In a meta-analysis, Lu et al. showed a significant reduction in infection rates (1% with MISS competed with 4% with open surgery) in patients treated for vertebral metastasis.21 Other studies have corroborated similar lower infection rates when using MISS, especially when compared with open surgery and this backs up its role as a significant tool for potentially reducing infection.22 Kwan et al. published a series of 50 patients with pathological metastatic vertebral fractures who underwent percutaneous fixation with pedicle screws that did not have a single case of postoperative infection or wound dehiscence, and demonstrated the improved wound healing that can be achieved with smaller incisions.23
MISS may also offer benefits in infection rates when radiotherapy is part of the treatment plan. Radiotherapy contributes to poor wound healing, leading to increased susceptibility to wound dehiscence and subsequent infection. Much higher infection rates have been reported when open spinal surgery is performed in conjunction with radiotherapy, but the use of MISS approaches may allow earlier initiation of radiotherapy than would be possible after open procedures.24
Considering the economic aspects, MISS could lead to a reduction in healthcare costs due to the associated reduced need for days of hospitalisation, transfusions, re-interventions, rehabilitation and pain management. In terms of survival, no differences have been found between patients treated by MISS and open surgery.25
Despite the advantages of MISS for metastatic spinal disease, there are some significant drawbacks, including the surgeon's learning curve, increased radiation exposure and imprecise instrumentation placement.26,27 Accuracy can be compromised, especially in stabilisation procedures, both by the limited visualisation afforded by the smaller approach and the potential for altered anatomy resulting from a metastatic implant. To alleviate these handicaps, technological advances have allowed the incorporation of techniques such as navigation and robotic-assisted surgery, which have great potential to reduce radiation risk and improve accuracy.28 Navigation technology surgery could be considered a well-established technique for the treatment of metastatic spinal disease, as numerous studies have evaluated its ability to mitigate the decreased visualisation inherent to MISS, as well as to reduce the radiation exposure of the equipment.
The use of robotics in spine surgery is a new addition, with potential applications in many aspects of spine surgery. Although robotic-assisted surgical technique is distinct from navigation in terms of instrumentation, in many respects it can be seen as an evolution of navigation surgery because it relies on pre-operative or intra-operative imaging and computer assistance.29,30 The main advantage of robotic surgery over navigation surgery is that it has the potential to eliminate human error. The use of robotic surgery in cases of spinal metastases has not yet been studied, but its use in MISS could be especially useful in cases with distorted anatomy. Several studies have evaluated the accuracy of pedicle screw placement and complication rates of robotic-assisted MISS compared to open surgery. Solomiichuk et al. found increased rates of perfect screw placement (67.2% vs. 63.6%) and acceptable placement (84.4% vs. 83.7%) with robotic, although these differences were not statistically significant.29
ConclusionThe use of MISS techniques in vertebral metastasis combines several advantages over the standard approaches: although they are equal to these in surgical time and number of instrumented levels, they have less bleeding, less need for transfusion and lower infection rates, without compromising the precision of instrumentation or increasing perioperative complications. In addition, in-hospital stay after surgery is shorter with MISS techniques and ambulation is earlier. In terms of survival, both approaches are similar.
It should be noted that these benefits may be especially desirable in these more fragile cancer patients, whose comorbidities often make them poor candidates for open procedures or put them at higher risk of complications associated with open surgery.
MISS surgery and its adjuncts (navigation and robotics) have the potential to improve treatment while reducing the risk of complications that can significantly affect the quality of life of these patients.
Level of evidenceLevel of evidence iv.
Conflict of interestsThe authors have no conflict of interests to declare.
FundingThe authors of this publication declare that they have not received any funding for the preparation and development of the work. The Sociedad Española de Cirugía Ortopédica y Traumatología has financed the expenses related to the open access publication of the article.