To assess the connection between the volume of injected cement and the vertebral volume measured through a volumetric analysis with a computed tomography (CT scan) in relation to the clinical result and the appearance of a leakage in patients who underwent a percutaneous vertebroplasty after an osteoporotic fracture.
Materials and methodsA prospective study of 27 patients (18 female–9 male) with an average age of 69 years old (50–81), and with a one-year follow-up. The study group presented 41 vertebrae with osteoporotic fractures that were treated with a percutaneous vertebroplasty with a bilateral transpedicular approach. The volume of injected cement was registered in each procedure and it was assessed together with the spinal volume measured through a volumetric analysis with CT scans. The percentage of the spinal filler was calculated. The appearance of cement leakage was proved by means of a simple radiography and a postoperative CT scan in all the cases. The leaks were classified according to the location in relation to the vertebral body (posterior, lateral, anterior and in the disc), and the significance (minor: smaller than the largest diameter of the pedicle; moderate: larger than the pedicle but smaller than the height of the vertebra; major: larger than the height of the vertebra).
ResultsThe average vertebra volume was 26.1cm3, the average volume of the injected cement was 2.0cm3 and the percentage of the average filler was 9%. A total of 15 leaks in 41 vertebrae appeared (37%). The leaks were posterior in 2 vertebrae, vascular in 8 and into the disc in 5 vertebrae. They were deemed as minor in 12 cases, moderate in 1 and major in 2 cases. The preoperative assessment of the pain was as it follows: VAS (8) and Oswestry (67%). The cessation of pain was immediate after a year with the following postoperative results: VAS (1.7) and Oswestry (19%). The only complication was the temporary neuritis with a spontaneous resolution.
ConclusionsThe injection of small amounts of cement, lower than the ones referred to by literary sources, obtains clinical results similar to the ones obtained by injecting higher amounts and it reduces the number of cement leaks and further complications.
Valorar la relación entre el volumen de cemento inyectado y el volumen vertebral evaluado mediante análisis volumétrico con tomografía axial computarizada (TAC) con relación al resultado clínico y la aparición de fugas en pacientes sometidos a vertebroplastia percutánea por fractura osteoporótica.
Materiales y métodosEstudio prospectivo de 27 pacientes (18 mujeres y 9 varones) con una edad media de 69 años (50-81) con un año de seguimiento, en los que se trataron 41 vértebras con fractura de origen osteoporótico mediante vertebroplastia percutánea con abordaje transpedicular bilateral. Se registró en cada procedimiento el volumen de cemento inyectado y se relaciona con el volumen vertebral medido mediante análisis volumétrico con la TAC. Se calculó el porcentaje de relleno vertebral. La aparición de fugas de cemento se comprobó mediante radiografía simple y la TAC postoperatoria en todos los casos. Las fugas se clasificaron tanto por el lugar de aparición respecto al cuerpo vertebral (posterior, lateral, anterior y al disco) como por la entidad: puntual (menor que el diámetro mayor del pedículo), moderada (mayor que el pedículo, pero menor que la altura de la vértebra) y masiva (mayor que la altura de la vértebra).
ResultadosEl volumen vertebral medio fue de 26,1cc, el volumen de cemento inyectado medio de 2,0cc y el porcentaje de relleno medio del 9%. Aparecieron un total de 15 fugas en 41 vértebras (37%). Las fugas fueron posteriores en 2, vasculares en 8 y al disco en 5 vértebras. Se consideraron puntuales en 12, moderadas en una y masivas en 2 casos. La valoración preoperatoria del dolor fue la siguiente: EAV (8) y Oswestry (67%). El cese de dolor fue inmediato con los siguientes resultados postoperatorios al año: EAV (1,7) y Oswestry (19%). La única complicación fue una neuritis transitoria con resolución espontánea.
ConclusionesLa inyección de pequeñas cantidades de cemento, inferiores a las referidas por la literatura, obtiene unos resultados clínicos similares a los conseguidos inyectando cantidades superiores y disminuye el número de fugas de cemento y la posibilidad de aparición de complicaciones.
Percutaneous vertebroplasty is a minimally invasive procedure involving the injection of an acrylic polymer into a collapsed vertebral body to relieve pain and improve bone stability. Although it was first used in 1987,1 it was not until an evidence-based evaluation in 2000 that the high efficacy of this technique was confirmed,2 demonstrating immediate clinical improvement in more than 80% of cases.3
Patients who are candidates for vertebroplasty are those with vertebral fractures of osteoporotic origin or lytic lesions (haemangioma, metastasis, myeloma) with severe or disabling pain, which cannot be relieved by appropriate medical treatment.
The exact mechanism by which pain relief is achieved is unclear. Two possible mechanisms have been postulated: mechanical, by reinforcement of the bone trabeculae, and thermal or chemical, by destruction of the nerve endings.
Complications associated with the technique are rare. The most serious are venous and arterial embolism, radicular, or medullary compression and are directly related to the amount of cement injected.4–6
The aim of this study was to assess the relationship between the volume of cement injected and the vertebral volume assessed by volumetric analysis with computerised axial tomography (CT) in relation to the clinical outcome and occurrence of leaks in patients undergoing percutaneous vertebroplasty for osteoporotic fracture.
Materials and methodsProspective, observational, and analytical study of patients with vertebral fragility fractures in our institution over a period of 2 years. The minimum follow-up after vertebroplasty was one year. The institutional ethics committee approved the study. The inclusion criteria were the presence of one or more vertebral fractures of at least 3 months’ duration that had not improved with conservative treatment. All the patients underwent plain X-ray and magnetic resonance, treating only vertebrae showing bone oedema in the sequences with fat suppression. Pain was assessed using a visual analogue scale (VAS) from 1 to 10 and disability was assessed using the Spanish version of the Oswestry questionnaire.
Surgical techniqueThe operation was performed in the operating theatre in a sterile environment with the patient in prone position under local anaesthesia and superficial sedation and image intensifier. The same surgical team operated on all patients. A bilateral transpedicular approach with 2 14G hollow trocars, 10cm in length was used in all patients. The trocars were introduced up to the middle third of the vertebral body prior to introduction of the cement, which was injected using a high-pressure system (Wacres®). Vertebrography with contrast injection was performed before injecting the cement, while the cement was being prepared. Although we do not currently routinely perform vertebrography, we believe that it can be useful to assess the venous drainage of the vertebral body and the possible direction of contrast leakage into the disc or epidural space, and to be aware of these leakage areas when injecting the cement. Most leakage occurs into the basivertebral venous complex and segmental veins. If rapid and massive drainage into the venous system is observed, the trocar tip is adjusted to obtain slower or less drainage. Furthermore, this technique does not require additional surgical time, as it can be performed during the cement working time. The cement is injected when it reaches a consistency similar to toothpaste on palpation. The volume of cement injected into each vertebra was recorded for each procedure.
The clinical outcome was assessed within the first 24h (immediate postoperative period), at one month, and at one year after the procedure using VAS and the Oswestry disability questionnaire. All the patients were operated as outpatients without requiring hospital admission.
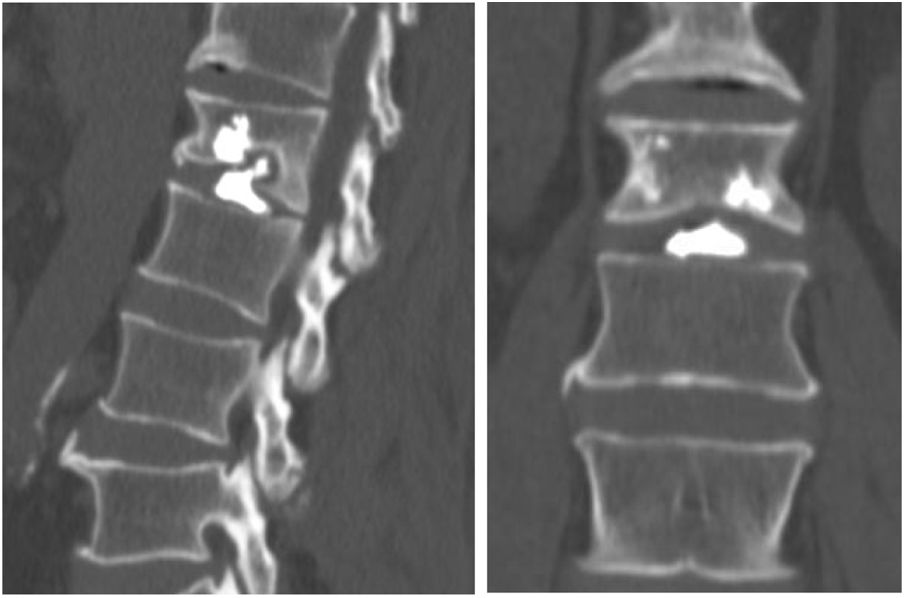
The occurrence of cement leakage was verified postoperatively by plain X-ray and CT (Aquileon 16, Toshiba) in all cases. We used a specific protocol (without contrast, collimation 1mm and reconstruction interval 1.8mm) and post-processed the images using multiplanar and 3D reconstructions. Vertebral body volume (pedicles and posterior arch excluded) was determined using software, which had been previously validated on pig vertebrae. Leaks were classified both by the location of their occurrence with respect to the vertebral body (posterior, lateral, anterior, and disc) and by the amount: punctate (smaller than the largest diameter of the pedicle), moderate (larger than the pedicle, but smaller than the height of the vertebra), and massive (larger than the height of the vertebra).
The percentage of vertebral filling was calculated by analysing the vertebral volume and the volume of cement injected together. All post-surgical images were evaluated and measured by the same radiologist.
Statistical methodologyWith the data collected from the medical records, an Excel® database was created and then used for statistical processing. For quantitative variables, measures of centralisation and dispersion (mean and standard deviation) were calculated, and for categorical variables, absolute and percentage distributions were calculated. Kruskal–Wallis or Student's t-tests were used for the comparison of means (after applying the Shapiro–Wilks normality test) and the χ2 test to correlate categorical variables. A significance level of .05 was used in all cases. The statistical software InfoStat® (v.2020) was used for statistical processing. The results are presented as graphs or tables as appropriate.
ResultsGeneral characteristicsThe study was based on a sample of 27 patients (41 vertebrae) operated consecutively for osteoporotic vertebral fracture (with more than 3 months’ duration) by means of percutaneous vertebroplasty. Of these, 18 were women and 9 men with a mean age of 69 years (50–81 years). The cause in 98% of cases was osteoporosis, 2% with rheumatoid arthritis.
The location of the fractures was mostly lumbar, at 73% (Table 1), and within these the L1 vertebra was the most frequently treated. It was the thoracic vertebrae in 27% and the most frequent was T12 in this group.
The mean vertebral volume was 26.1cm3 (T8: 15.6; L5: 38.1), the mean injected cement volume was 2.0cm3 (1–4cm3), and the mean filling percentage was 9% (Table 2).
Analysis of leaksA total of 15 cement leaks occurred in 41 vertebrae, which is 37% of the total number of vertebrae (Fig. 1). More than half of the leaks were vascular (Fig. 2), to the disc in 5 vertebrae (Fig. 3), and 2 posterior vertebrae (Fig. 4).
They were considered punctate in 12 cases, moderate in one case, and massive in 2 cases.
When evaluating the mean vertebral volume according to patient group with and without leakage, it was observed that the mean of the group without leakage was higher than those with leakage: 27 vs. 24.5cm3 (Table 3). In the case of injected cement, it was the other way around, the average amount of cement injected in the group that had a leak was higher: 2.13 vs. 1.95cm3.
Preoperative pain assessment was as follows: VAS (8) and Oswestry (67%). Cessation of pain was immediate in all patients, showing a decrease to scores of 2.0 and the postoperative results were maintained at one year: VAS (1.8) and Oswestry (19%).
Overall, no statistically significant differences were found in terms of mean VAS in the groups with and without leakage. It is noteworthy that the VAS assessment at one month was higher for the group of patients with cement leakage: 2.9 vs. 1.8 (Table 4).
The only complication was a transient neuritis with spontaneous resolution. At the postoperative follow-up at one year, no new vertebral fractures had appeared.
DiscussionPercutaneous vertebroplasty in the treatment of osteoporotic vertebral fractures which do not respond to medical treatment, is a safe, effective, and widespread procedure used in recent years.1–9 The main complications of this technique are due to the possible leakage of cement from inside the vertebral body, either into the epidural space, the venous plexus, adjacent discs, and even the production of pulmonary embolism.7,10–12 Spinal cord injury, infection in the operated site, and even death are also complications reported in the literature.6–18
However, despite wide dissemination of the technique, there is great variability in the procedure followed by the different authors, especially with regard to the volume of cement required to achieve a good clinical result and minimise the possibility of leaks.7,19–24
Different strategies have been developed to prevent cement extravasation. The advocates of kyphoplasty argue that there are fewer cement leaks compared to vertebroplasty, however it now seems that these are higher than previously thought.3,6,17,25–27
This great variability is due to the idea that injecting large amounts of cement to fill the vertebral body as much as possible increases the strength and resistance of the vertebral body and, therefore, the clinical results. Unfortunately, this increased filling of the vertebral body is accompanied by an increase in the presence of cement leakage.9
There are few studies relating the volume of cement injected and clinical outcomes.3,8,18,20,21,28
Zhu et al.26 conclude that cement leakage is very common with percutaneous vertebroplasty. Fracture severity and a larger volume of injected bone cement are the 2 independent risk factors that most predispose to leakage.
He et al.27 studied the effect of bone cement distribution and clinical response with percutaneous kyphoplasty in osteoporotic vertebral compression fractures. As the volume of cement injected was greater, they had a higher percentage of leaks, despite the use of the kyphoplasty balloon, fortunately all of which were asymptomatic.
It is generally accepted that the percentage of filling of the fractured vertebral body is not related to the clinical outcome,8,12,27 and therefore it would be reasonable to establish the minimum percentage of filling of the vertebral body necessary to achieve a good result. In this sense, we believe it important to establish the individualised volume of each vertebra according to its location (thoracic, lumbar) and the volume of cement necessary to achieve a clinically significant effect.
We found a significantly lower percentage of leakage (37%) assessed by CT than that reported by other authors, such as Álvarez et al.5 (88%), achieving a percentage of filling of the vertebral body of 9% and a clinical improvement both measured by VAS (from 8 to 1.7) and by the Oswestry disability questionnaire (from 67% to 19%) similar to those obtained by other series where a greater amount of cement is used.
The mean amount of cement injected in our series was 2.0cm3, significantly lower than that usually reported in the literature, where an average of 3–5ml is used,7,27,27 which may be related to the lower incidence of leaks found in our patients.
Other authors have investigated the effects of polymethylmethacrylate cement viscosity and bone porosity on cement leakage and the occurrence of new vertebral fractures after percutaneous vertebroplasty. In a prospective study, Alhashash et al.29 conclude that the clinical outcome of vertebroplasty is not related to cement viscosity. However, they point out that lower cement viscosity and a higher degree of osteoporosis are significant risk factors for the occurrence of cement leakage.
Tomé-Bermejo et al.30 after CT scanning of 272 vertebrae treated with vertebroplasty report a cement leakage rate of 76%, and the basivertebral and segmental veins are the areas with the highest incidence. These authors use from 4cm3 to 5cm3 of cement per vertebra, injecting the cement with a viscosity similar to toothpaste, as we do.
The limitation of our work are the limited number of patients and vertebrae, not having a record of the pressure at which the cement is injected, not having measured the degree of osteoporosis of the fractured vertebra or correlating the loss of vertebral height with the clinical result. It was also not possible to perform volumetric CT measurement of the leaks, and therefore the described classification was used.
ConclusionsThe injection of small amounts of cement, lower than those referred to in the literature, achieves similar clinical results to those by injecting larger amounts and reduces the number of cement leaks and thus the possibility of complications.
We recommend using quantities between 1 and 1.5cm3 per pedicle depending on the vertebral size (dorsal/lumbar) as the same clinical outcome is achieved, reducing cement leakage and its severity.
Level of evidenceLevel of evidence II.
Conflict of interestsThe authors have no conflict of interests to declare.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Ethics committee approvalApproved by the ethics committee of the centre.