Coxarthrosis is one of the most frequent and disabling pathologies. 20% of individuals over 60 years of age will develop symptomatic coxarthrosis and 10% of them will need a hip replacement; it is probably one of the orthopaedic procedures that most increases quality of life. When we recommend arthroplasty in clinical practice, patients often ask about the prognosis of their other hip. Will it deteriorate in the same way? Will it be necessary to replace it? When?
The aim of the study is to determine if there is any variable or radiological sign that predicts the medium-term prognosis of the contralateral hip after total hip arthroplasty.
Material and methodsA retrospective review of patients who underwent total hip arthroplasty in our hospital during 2011 and 2012 was carried out, with a total of 543 patients. The coxarthrosis degree at X-ray was determined at the time of the first arthroplasty and at regular intervals during follow-up, according to the JOA and Tönnis classifications, analyzing each of the items included in these classifications. Its relation with the progression of osteoarthritis and the need of contralateral hip replacement was established.
Results and conclusionsA progression of osteoarthritis of the contralateral hip could be expected in the next 3 years in 10% of patients. This progression will be greater and faster in those with JOA grade III–IV/Tönnis grade II–III, especially, in those with greater joint narrowing and femoral head shape score, and can reach between 25 and 30% of patients. The initial JOA/Tönnis degree is a predictive factor for requiring a hip replacement on the contralateral side.
La coxartrosis es una de las patologías más frecuentes e incapacitantes. El 20% de los mayores de 60 años desarrollarán coxartrosis sintomática y el 10% requerirán una prótesis total de cadera. La artroplastia total de cadera es uno de los procedimientos quirúrgicos que más aumenta la calidad de vida de estos pacientes. Cuando recomendamos la artroplastia en la práctica clínica, los pacientes a menudo preguntan sobre el pronóstico de su otra cadera: ¿Se deteriorará de la misma forma? ¿Será necesario operarla? ¿Cuándo?
El objetivo es determinar si existe alguna variable o signo radiológico que prediga el pronóstico a medio plazo de la cadera contralateral tras una artroplastia total de cadera.
Material y métodosSe realizó un estudio retrospectivo de pacientes intervenidos de artroplastia total de cadera en nuestro hospital durante los años 2011 y 2012, con un total de 543 pacientes.
Se determinó el grado de coxartrosis, según las clasificaciones JOA y Tönnis, en la radiografía de ambas caderas en el momento de la primera artroplastia y a intervalos regulares durante el seguimiento, analizando cada uno de los ítems incluidos en estas clasificaciones. Se estableció la relación de estos hallazgos radiográficos con la progresión de la artrosis y la necesidad de artroplastia contralateral.
Resultados y conclusionesPodría esperarse una progresión de la artrosis de la cadera contralateral en los próximos 3 años en el 10% de los pacientes. Esta progresión será mayor y más rápida en aquellos con grado JOA III-IV/Tönnis II-III, y especialmente en aquellos con mayor estrechamiento articular y mayor alteración de la cabeza femoral, pudiendo alcanzar entre el 25 y el 30% de los pacientes.
El grado de JOA/Tönnis inicial es un factor predictor de necesitar una prótesis de cadera contralateral.
Coxarthrosis is one of the most prevalent diseases in the adult population, consistently ranking as one of the most common causes of functional disability as well as being an immense socio-economic burden.1 Total hip arthroplasty increases patients’ quality of life, with quality-adjusted life years approaching that of healthy patients of similar age.2
The WHO indicates that approximately 10% of men and 18% of women over the age of 60 years have symptomatic osteoarthritis.3 Eighty per cent of people with osteoarthritis have limited movement and up to one third could be considered severely disabled. It is a problem that will increase in incidence over time, with the population of people over 60 estimated to triple by 2050.3
When trauma specialists recommend arthroplasty to treat coxarthrosis in their daily clinical practice, patients often ask about the prognosis of their contralateral hip. Will it deteriorate in the same way? Will it have to be operated in the future? When?
The aim of this study is to determine whether there are any radiological findings that predict the medium-term prognosis of the contralateral hip after total hip arthroplasty for idiopathic coxarthrosis. The aim is to assess the statistical likelihood of needing a contralateral arthroplasty and to answer the aforementioned questions.
Material and methodsThe study was approved by our institution's ethical committee.
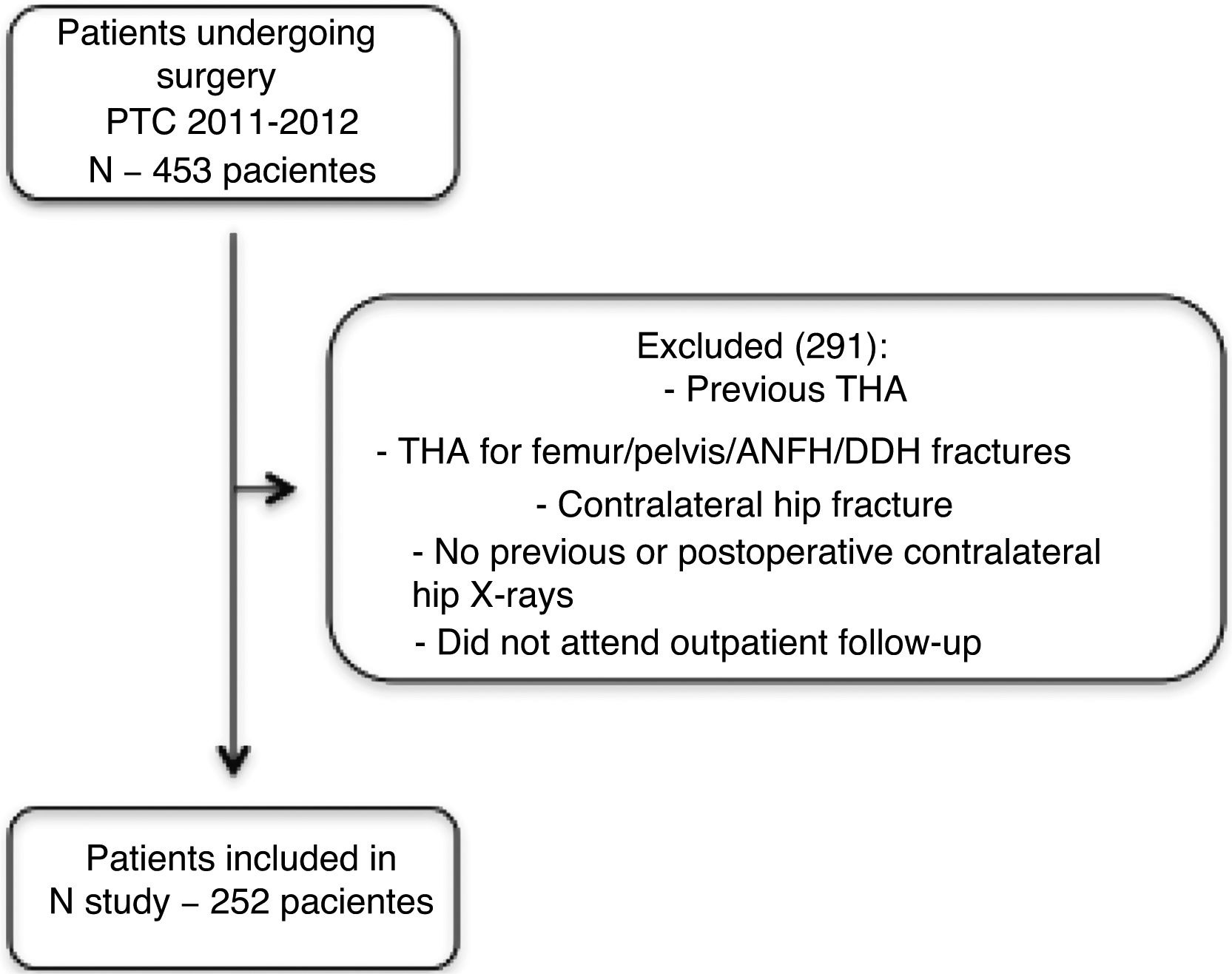
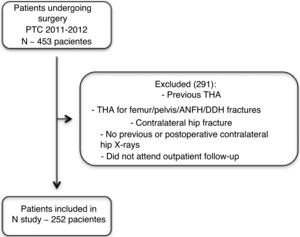
Study populationWe conducted a retrospective study of a case series of patients who underwent total hip arthroplasty in our hospital between 2011 and 2012, comprising a total of 543 patients.
The inclusion criterion was idiopathic coxarthrosis with a minimum radiographic follow-up of 2 years after the operation or until contralateral hip arthroplasty.
Radiographic analysis and imagingIn this group, based on medical history number, epidemiological data on age, sex, laterality, and disease duration were studied in the database of the IMPAX radiological imaging programme (Impax 6, Agfa, Mortsel, Belgium).
The grade of coxarthrosis was determined at the time of the first arthroplasty and at regular intervals during follow-up according to the JOA4 and Tönnis5 classifications, and each of the items included in these classifications, such as joint narrowing, bone architecture, and femoral head/acetabulum shape, was also analysed independently. Imaging follow-up was at 1 month, 6 months, 1 year, and 2 years. New radiographic studies were later performed in patients with symptoms in the contralateral hip.
From these data, the progression of osteoarthritis was analysed based on JOA and Tönnis grades, the progression of the contralateral hip to the status of the first operated hip according to the Tönnis grades, the rate of contralateral hip replacement and its relationship to the JOA and Tönnis grades on the initial radiograph.
Statistical analysisIn the estimation of progression of radiographic grades of coxarthrosis and contralateral prosthesis-free survival, a Kaplan–Meier survival analysis with a Greenwood method was used to estimate its variance. The graphical representation used logarithmic values to plot confidence intervals. A Cox regression test was used to compare survivals.
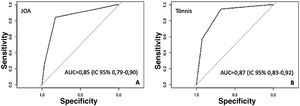
ROC curves were calculated for both classifications to analyse the correlation between the JOA and Tönnis classifications and the need for contralateral total hip arthroplasty (THA).
Statistical analyses were performed using R statistics version 3.5.2 Eggshell Igloo.
ResultsAfter applying the inclusion criteria, the sample analysed consisted of 252 patients (Fig. 1), of whom 131 were female (52%) and 121 male (48%).
Patients underwent surgery at a mean age of 67 years, median 68 years.
Of these patients, 58 underwent surgery on the contralateral hip (23%), which was the left side in 57.1% of cases and the right in 42.9%.
The mean follow-up of the patients who underwent contralateral hip surgery was 30.12 months (1.2–75.84). The remaining 194 patients did not have contralateral hip surgery, with a mean follow-up of 55.56 months (.96–100.44).
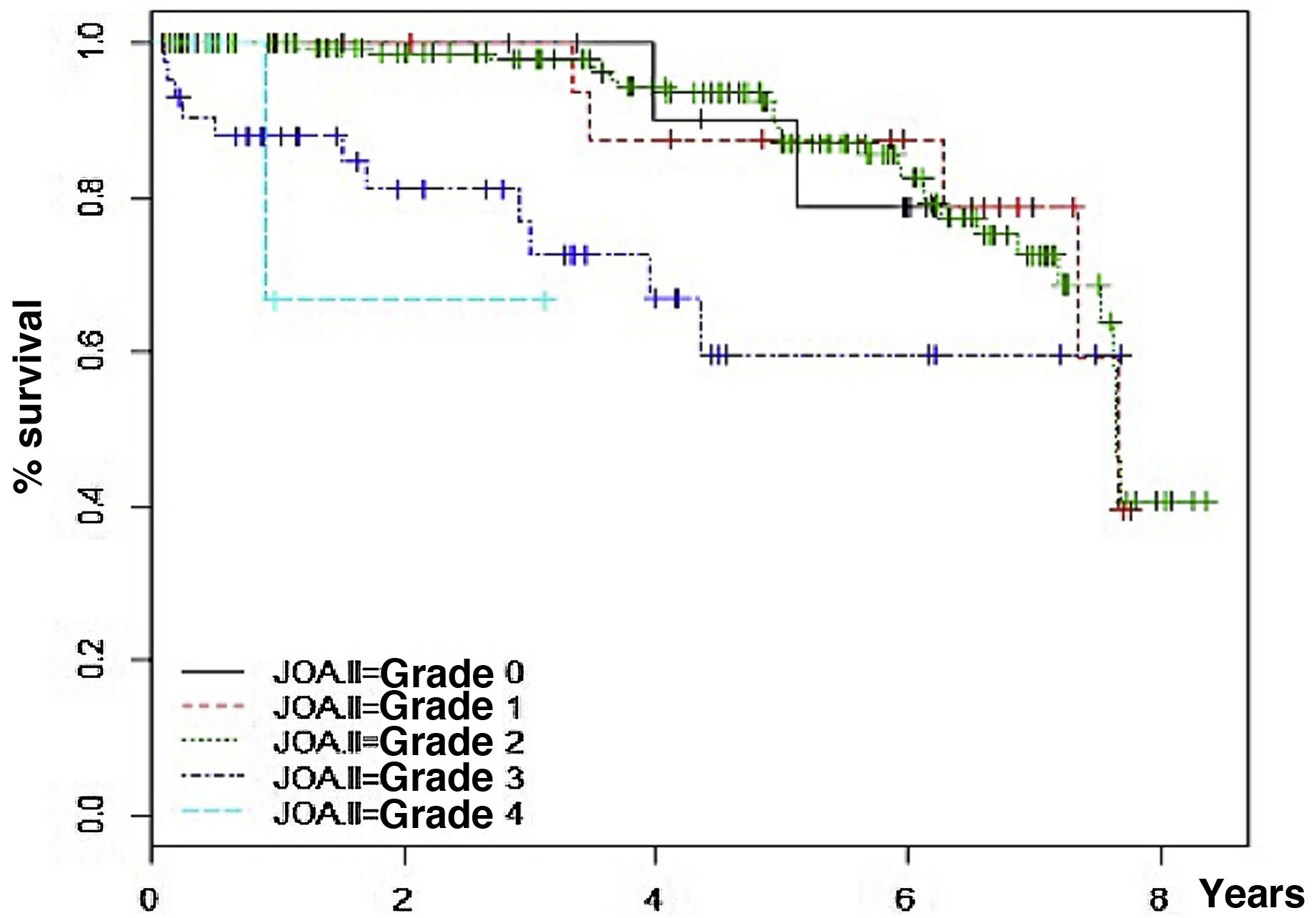
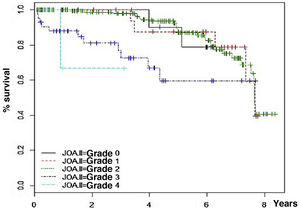
Progression of coxarthrosis according to JOA classification was 7% at 3 years (95% CI 3–10%) and 21% at 6 years (95% CI 14–28%).
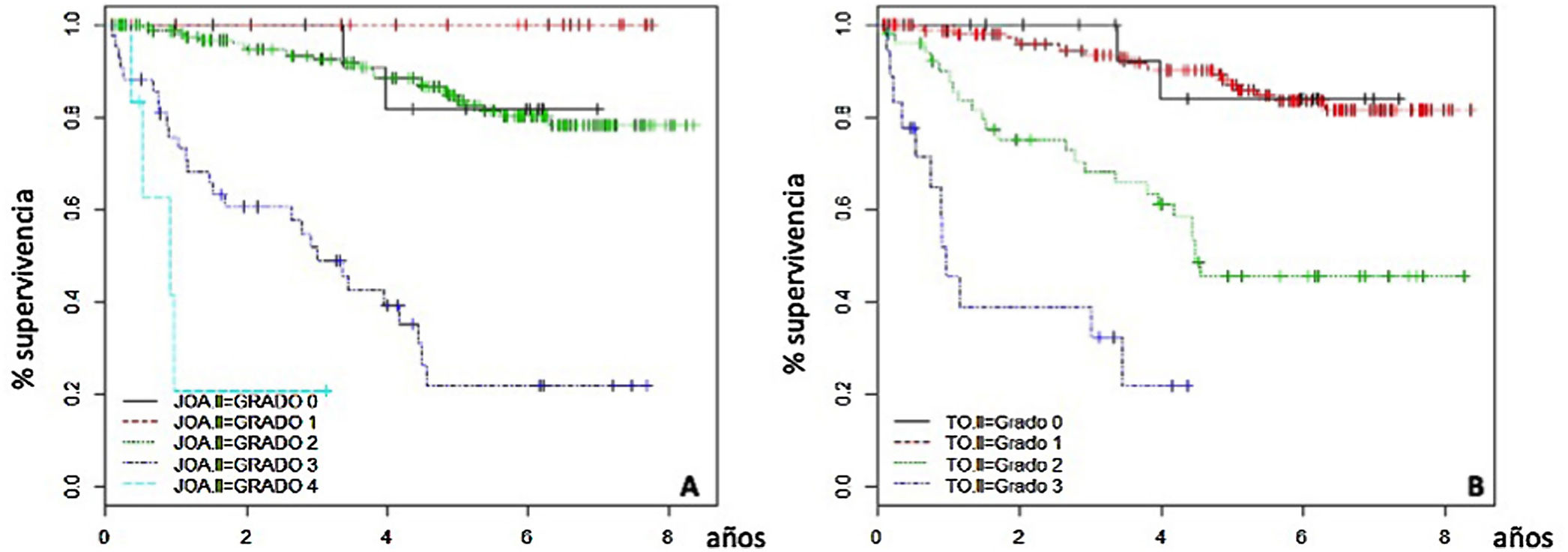
JOA grade III showed a higher progression of coxarthrosis than previous stages (p<.01). Progression of coxarthrosis with a baseline JOA II was 2% (95% CI 0–5%) and 28% in patients with a baseline JOA III (95% CI 10–42%) at 3 years. At 6 years, progression was 18% and 40%, respectively (Fig. 2).
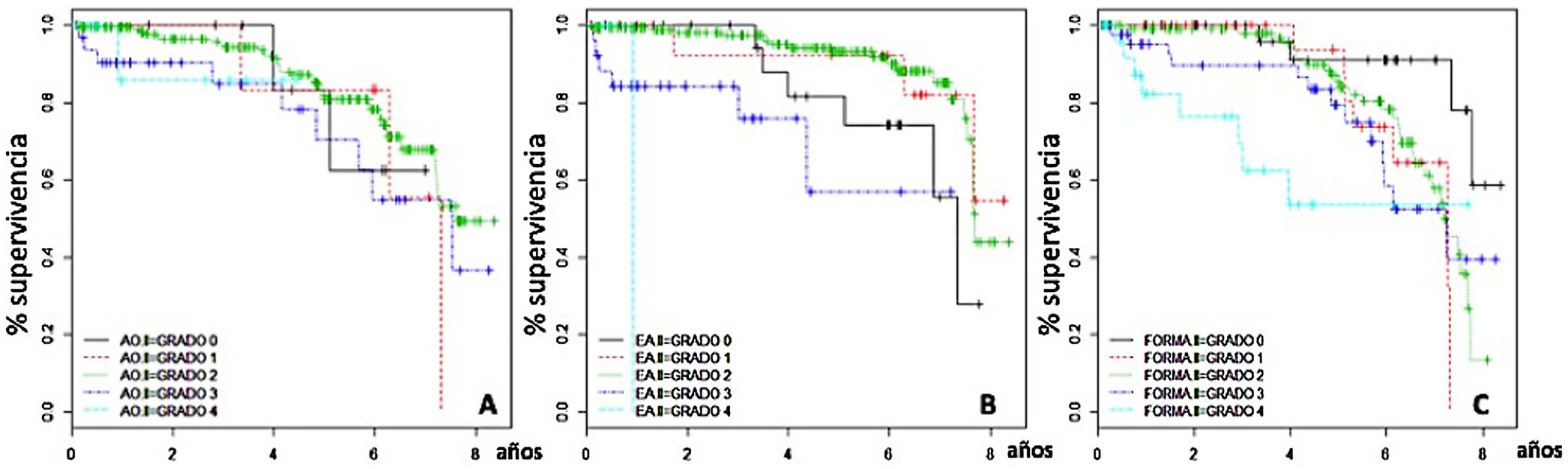
The bone architecture of the JOA classification was not a determinant of progression of coxarthrosis of the contralateral hip after the initial prosthesis; however, joint narrowing was a determinant of progression (p<.01) as was shape; progression of osteoarthritis was influenced by previous morphology (p<.01) (Fig. 3).
Progression of coxarthrosis assessed with the Tönnis classification was 10% at 3 years (95% CI 6–14%) and 35% at 6 years (27–42%).
At 3 years, there was osteoarthritis progression in 32% of the patients with Tönnis II (95% CI 17–44) and in 68% with Tönnis III (95% CI 34–84) (Fig. 4A). In the same time period 35% of the patients with initial Tönnis II reached the grade of osteoarthritis at which the other hip was operated and 68% with Tönnis III (Fig. 4).
The absolute rate of contralateral hip replacement in our population was 16% at 3 years and 23% at the end of follow-up.
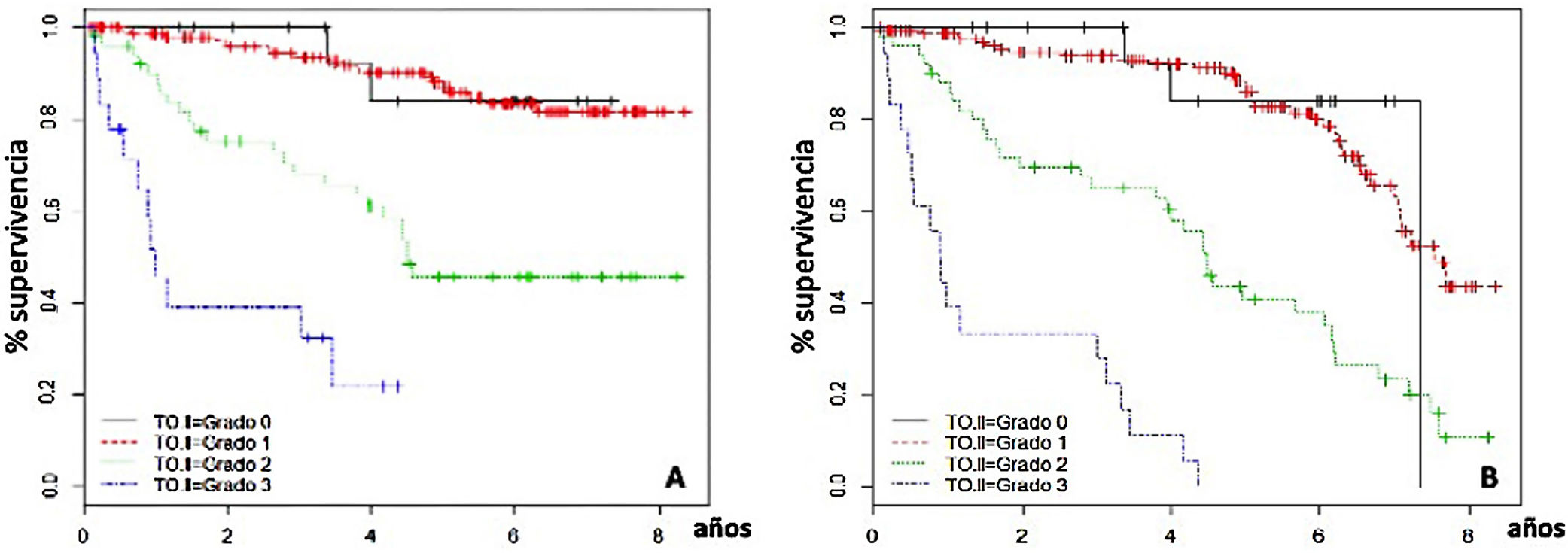
The incidence of contralateral THA at 3 years was 8%, 49%, and 100% for JOA grades II, III, and IV (Fig. 5A) and 7%, 32%, and 68% at 3 years for initial Tönnis grades I, II, and III, respectively (Fig. 5B).
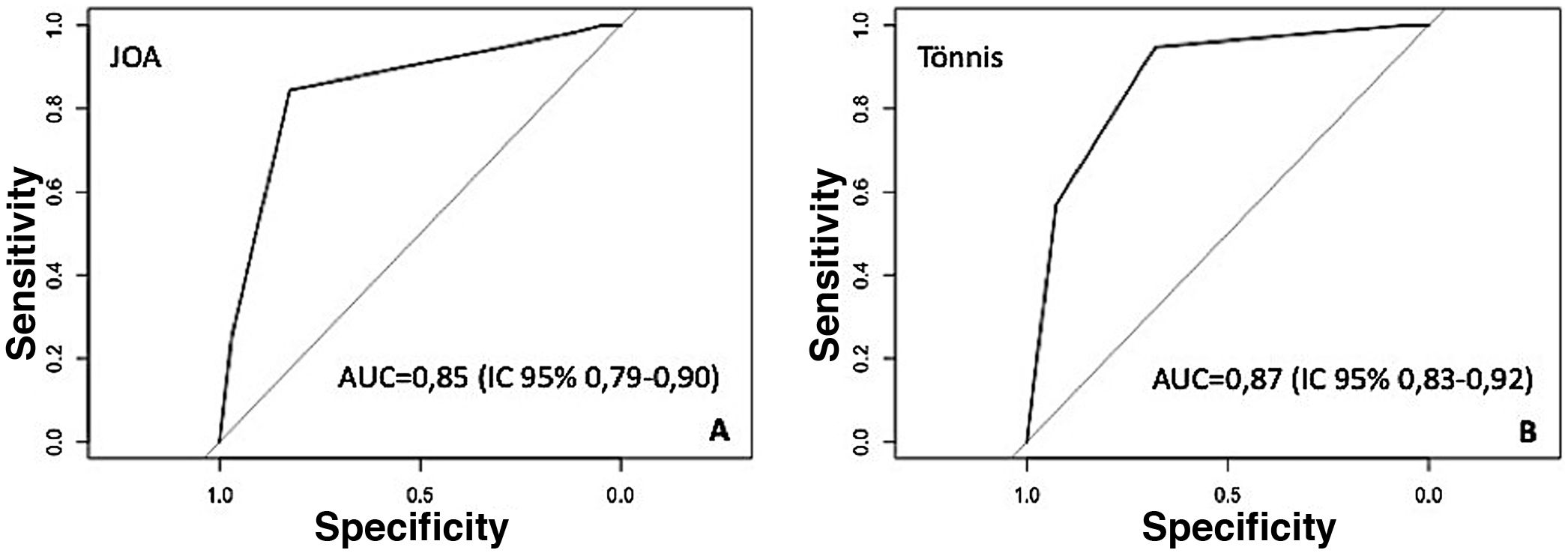
Considering the ability to determine the need for contralateral hip replacement, the area under the ROC curve was .85 for the JOA classification (95% CI .79–.9), whereas for the Tönnis classification the area under the ROC curve was .87 (95% CI .83–.92) (Fig. 6).
DiscussionA total of 16% of patients undergoing hip replacement will require contralateral hip surgery within 3 years; this proportion will double in those with moderate contralateral osteoarthritis.
Several studies have analysed the risk factors for developing hip osteoarthritis.6–8 Ritter et al.,6 as early as 1996, found that 37% of contralateral hips diagnosed as “normal” would develop osteoarthritis within 10 years, and 8% would eventually undergo total hip arthroplasty. Vossinakis et al.7 described that patients with idiopathic unilateral osteoarthritis have a greater tendency to develop osteoarthritis in the contralateral hip than patients with hip dysplasia. Polat et al.8 found that femoroacetabular impingement was more frequently observed in the asymptomatic contralateral hip of patients who underwent hip arthroplasty secondary to idiopathic coxarthrosis than in the control group. Amstutz and Le Duff9 estimated that the percentage of patients with a symptom-free contralateral hip was 59% at 10 years and 73% at 5 years. In their series, 87% of patients were free of arthroplasty at 5 years and 81% at 10 years. These results are similar to those obtained in our study, where a radiological progression at 3 years of 7% and 10% and at 6 years of 20% and 35% was observed for each one-grade increase in JOA and Tönnis classifications, respectively. The risk of progression of osteoarthritis is different according to the grade of the initial osteoarthritis, with Tönnis grades II and III, for example, showing a much higher risk of progression. A total of 83% of patients were found to be free of contralateral prostheses at 5 years.
The scales used are based on radiographic parameters, including bone architecture (sclerosis and cysts in the femoral head and acetabulum), joint space narrowing, and joint shape (including osteophytes and sphericity of the femoral head). There is general agreement that joint narrowing is the most reproducible parameter10,11 and that it is strongly linked to pain and disease progression.12 In our study, joint space narrowing and femoral head morphology were found to be the main factors conditioning coxarthrosis progression (p<.01), whereas bone architecture is not a determinant of coxarthrosis progression in the JOA and Tönnis classifications.
In 2016, Wyles et al.13 analysed the progression of the contralateral hip in 172 patients aged 55 years or younger who had previously undergone total hip arthroplasty, with no signs of osteoarthritis (Tönnis grade 0) in the contralateral hip at the time of surgery. They observed, with a mean follow-up of 20 years, that degenerative changes occurred more rapidly in patients who had undergone surgery for hip dysplasia, followed by femoroacetabular impingement, and normal morphology. In patients who developed early incipient degenerative changes (Tönnis grade 1), the probability of requiring total hip arthroplasty implantation at 10 years was one in 3 for hip dysplasia and one in 5 for those with femoroacetabular impingement or normal morphology. At 20 years, the likelihood was 2 in 3 for hip dysplasia and 1 in 2 for femoroacetabular impingement and normal morphology. With these findings, they concluded that degenerative changes occurred early in patients with hip dysplasia, while the natural progression of femoroacetabular impingement was similar for hips with normal morphology. However, patients with cam deformity and concomitant acetabular dysplasia developed osteoarthritis early.
Because not all patients have the same clinical manifestations in the different grades of osteoarthritis and do not require arthroplasty with the same degree of radiographic involvement, we have analysed, using Tönnis grades, the time of progression of the contralateral hip to the grade of osteoarthritis of the hip that was operated on, stratified by the initial degree. At 3 years, 7% with initial Tönnis I, 35% with Tönnis II, and 68% with Tönnis III have reached this grade. The likelihood of the contralateral hip progressing to the status of the operated hip is a function of the Tönnis grade at the time of the first operation and the grade of the contralateral hip at the start of follow-up. In other words, if the patient with Tönnis grade 2 undergoes surgery, the healthy hip will be more likely to reach that grade.
ROC curves were calculated for both classifications to analyse the correlation between the JOA and Tönnis classifications with the need for contralateral THA. The area under the curve was higher for the latter. This difference suggests that the Tönnis classification could better predict the outcome of the contralateral hip, however, it does not reach statistical significance (p=.16).
All these data allow us to inform the patient of the likelihood of contralateral hip osteoarthritis progression and the risk of requiring another hip arthroplasty. Given that the probability of contralateral prosthesis at 3 years is 100% for JOA IV and 68% for Tönnis III, it would be interesting to evaluate in future studies the option of performing bilateral arthroplasties in selected patients in a single stage, since, according to several studies, this does not increase complications in selected patients.14–17
This study has limitations: it is a retrospective study, and the personal history and clinical situation of each patient were not analysed, nor were their socioeconomic circumstances. The radiographs were obtained at protocolised intervals, which implies that the patients may have needed hip arthroplasty earlier than recorded. The reason for doing it this way was to avoid unnecessary visits and radiation in asymptomatic patients after total hip arthroplasty, but these data should be considered in the analysis of the results. The surgical waiting list, which in certain circumstances could be up to one year, generates a delay that would overestimate the survival of the contralateral hip.
ConclusionsProgression of osteoarthritis in the contralateral hip over the following 3 years can be expected in about 10% of patients. This progression will be greater and more rapid in those with grade II–III (JOA or Tönnis) and, particularly, in those with greater joint narrowing and higher head shape scores, and may reach 25–30% of patients.
We can inform our patients that the likelihood of having to operate on the other hip in the short to medium term would be between 16% and 23%, but would increase in cases that already have moderate osteoarthritis, which could be between 32% and 49% and would be around 100% in cases with severe osteoarthritis.
It is difficult to determine the prognosis of total hip arthroplasty but, despite the limitations of this study, we can make a reliable approximation and the patient can be informed of the likelihood of requiring a contralateral hip replacement.
Level of evidenceLevel of evidence III.
FundingNo specific support from public sector agencies, commercial sector or non-profit organisations was received for this research study.
Conflict of interestsThe authors have no conflict of interests to declare.