The effective relief of postsurgical pain in patients undergoing knee arthroscopy is important to allow the initiation of activities of daily living. The objective of this study is to demonstrate the analgesic efficacy of dexmedetomidine as an adjuvant added to ropivacaine by the intra-articular route.
MethodSeventy patients underwent knee arthroscopy which were randomly assigned into two groups (n=35). The RD group received ropivacaine 1.5mg/kg plus dexmedetomidine 1μg/kg intra-articularly. Group R received ropivacaine 1.5mg/kg intra-articularly. The analgesic effect was evaluated by measuring the intensity of pain (VAS score) and the duration of analgesia.
ResultsA longer duration of the analgesic effect was observed in the RD group (655min) compared to the R group (318min) being statistically significant (p=0.03).
ConclusionDexmedetomidine as an adjuvant to intra-articular ropivacaine improves the quality and duration of postoperative analgesia in patients undergoing knee arthroscopy.
Introducción El adecuado control del dolor posquirúrgico en pacientes intervenidos de artroscopia de rodilla resulta de suma importancia para permitir una movilización precoz, y con ello, el inicio de la rehabilitación.
MétodoSe intervino a 70 pacientes de artroscopia de rodilla los cuales fueron asignados aleatoriamente en dos grupos (n=35). El grupo RD recibió ropivacaína 1,5 mg/kg más dexmedetomidina 1 μg/kg por vía intraarticular. El grupo R recibió ropivacaína 1,5 mg/kg por vía intraarticular. Se evaluó el efecto analgésico midiendo la intensidad del dolor (puntuación de escala visual análoga) y la duración de la analgesia.
ResultadosMayor duración analgésica en el grupo RD (655 minutos) comparado con el grupo R (318 minutos), siendo esta diferencia estadísticamente significativa (p=0,03).
ConclusiónLa dexmedetomidina como adyuvante de la ropivacaína por vía intraarticular mejora la calidad y la duración de la analgesia posquirúrgica en pacientes intervenidos de artroscopia de rodilla.
At present, arthroscopic knee surgery is one of the most widely practiced minimally invasive surgical procedures in modern orthopaedics; nevertheless, it has been associated with a varying degree of post-surgical pain.1 Irritation of the free nerve endings of the synovial tissue, the anterior fat pad, and the articular capsule when performing the arthroscopic surgical resection are among the numerous causes of post-surgical pain in individuals who have undergone arthroscopy of the knee.1–3
Post-surgical pain in patients who have undergone this intervention negatively impacts early mobilisation, rehabilitation, and state of mind, which leads to a prolonged hospital stay. Given that pain is common among these subjects, effect relief is of the utmost importance, inasmuch as it enables the person to be discharged from the hospital early and enhances their postoperative recovery.1–7 Postoperative multimodal analgesia provides us with several options for pain relief, such as systemic medication (narcotics, NSAID), central or peripheral nerve block, as well as the intraarticular administration of drugs (ketorolac, α2 agonists, opioids, local anaesthetics). However, none is free of limitations such as the need for special equipment, monitoring, and the risk of complications.2,3 This is why recent studies recommend the administration of intra-articular drug cocktails instead of other types of multimodal analgesia, in light of the great frequency of side effects such as nausea, vomiting, sedation, gastric irritation, pruritus, urinary retention, respiratory depression, and partial motor blockade, among others.8
Intra-articular administration of single-dose local anaesthetic solutions is used to provide better analgesia after knee arthroscopy, minimising the use and possible side effects of oral and intravenous administration of rescue analgesics.9–14 Previous studies have used intra-articular local anaesthetics such as lidocaine; bupivacaine and ropivacaine; opioids, such as morphine and fentanyl, and α2 agonists such as clonidine, dexmedetomidine, and even magnesium sulphate, and have reported variable results in terms of both duration and intensity of analgesia.1–16 Nevertheless, administration of local anaesthetics alone does not guarantee complete analgesia.17
Ropivacaine is a local anaesthetic consisting of an aminoamide, which acts by reversibly blocking the voltage-dependent sodium channels of the membrane of the afferent nerve fibres. It is less toxic than other long-acting local anaesthetics such as bupivacaine, which is why it is currently being increasingly used for post-surgical analgesia.2 However, certain patients may experience the following side effects: hypotension, hypertension; bradycardia, tachycardia; nausea, vomiting; headache, paraesthesia, dizziness, urinary retention, and fever.6 Previous studies have concluded that the use of an intra-articular dose in the knee of 0.75–1.5mg/kg is both effective and safe, without increasing the occurrence of adverse effects.14–16
Dexmedetomidine is a highly selective α2 adrenergic agonist with analgesic, sedative, antihypertensive, and anaesthetic effects when used systemically.2 The analgesic mechanism of this drug when administered intra-articularly has yet to be is clearly defined, although it may be similar to intra-articular clonidine1. It may act on the presynaptic α2 adrenergic receptors and inhibit the release of noradrenaline at the peripheral afferent nociceptors. It is possible that the resulting local anaesthetic effects are related to the inhibition of the conduction of the nerve signals through the C and Aδ fibres, as well as to stimulating the release of an enkephalin-like substance at the peripheral level.1 Other adverse effects have been reported following systemic use such as hypotension, hypertension, bradycardia, myocardial ischaemia, tachycardia, hyperglycaemia, hypoglycaemia, agitation, nausea, vomiting, dry mouth, withdrawal syndrome, hyperthermia, respiratory depression, and polyuria.2–4 Other studies report that intra-articular delivery of dexmedetomidine is capable of significantly lowering the score for post-surgical pain and the usage of post-surgical painkillers, as well as increasing the duration of the analgesic effect when administered directly into the joint in the context of arthroscopy of the knee, either as the sole agent or as an adjuvant to another local analgesic. Thus, the dose that has been found to be safe and efficacious ranges from 1μg/kg to 2μg/kg.16,18
The objective of our study was to assess the analgesic efficacy of the intraarticular administration of ropivacaine plus dexmedetomidine versus ropivacaine alone as an analgesic adjuvant in patients who have undergone arthroscopy of the knee, as well as to report the appearance of possible side effects. Our hypothesis was that the combination of ropivacaine and dexmedetomidine provides better post-surgical analgesic coverage and duration, thereby having a positive effect on rehabilitation and early integration.
MethodologyThis was a controlled, prospective, longitudinal, randomised, blinded, prospective clinical trial conducted at the Hospital Español de México (Spanish Hospital of Mexico) between January 2019 and January 2022.
The inclusion criteria consisted of: patients aged 18–60 years classified as having an ASA I and II physical status, undergoing arthroscopic surgery of the knee during the study period, who gave their informed consent prior to surgery, and whose procedure was carried out under general anaesthesia.
The exclusion criteria consisted of a history of allergy to any of the study drugs, kidney failure, liver failure, cardiovascular disease, hypertension (use of beta-blockers), surgical wound drains, patients undergoing regional anaesthesia, the use of non-steroidal anti-inflammatory drugs (NSAIDs) and opioids 24h prior to surgery, and arthroscopic surgery that was converted to open surgery.
Participants were divided into two main groups for the purposes of our study: those who were undergoing minor knee surgery (procedures including: meniscus repair, release of lateral retinaculum, and removal of free bodies) and those who were having major knee surgery (procedures including: reconstruction of the anterior cruciate ligament [ACL] by any surgical technique and microfractures).
The study group was given ropivacaine (0.75%) at a dose of 1.5mg/kg plus dexmedetomidine (1%) at a dose of 1μg/kg, while the comparator group received ropivacaine (0.75%) at a dose of 1.5mg/kg.
Seventy patients were enrolled. Forty-three were male and 27 were female, and each group included 35 patients. A visual analogue pain scale (VAS) was explained to all patients with prior informed consent, according to which 0 indicated no pain and 10, severe pain. After completion of the arthroscopic procedure and before ischaemia removal and skin closure, intra-articular drug infiltration was performed through the arthroscopic portal by a member of the surgical team, who was blind as to the inclusion group.
The parameters observed were the time to the first dose of rescue analgesia (defined as the time elapsed from the post-surgical intra-articular injection, to the time of the first request for rescue analgesia consisting of 50mg tramadol hydrochloride administered intravenously when the patients presented with a VAS score of ≥4), the number of times rescue analgesia was requested over the following 24h, the visual analogue scale (VAS) at rest and the mobilisation at 1, 2, 6, 12, and 24h assessed by the medical staff of orthopaedic residents on duty at the Hospital Español, blinded as which drug was being given. Adverse effects such as nausea, vomiting, hypotension (defined as a reduction of the MAP<25% of baseline), bradycardia (defined as HR<45beats/min), respiratory depression, pruritus, and urinary retention were recorded. Finally, the length of hospital stay following the surgical event was recorded.
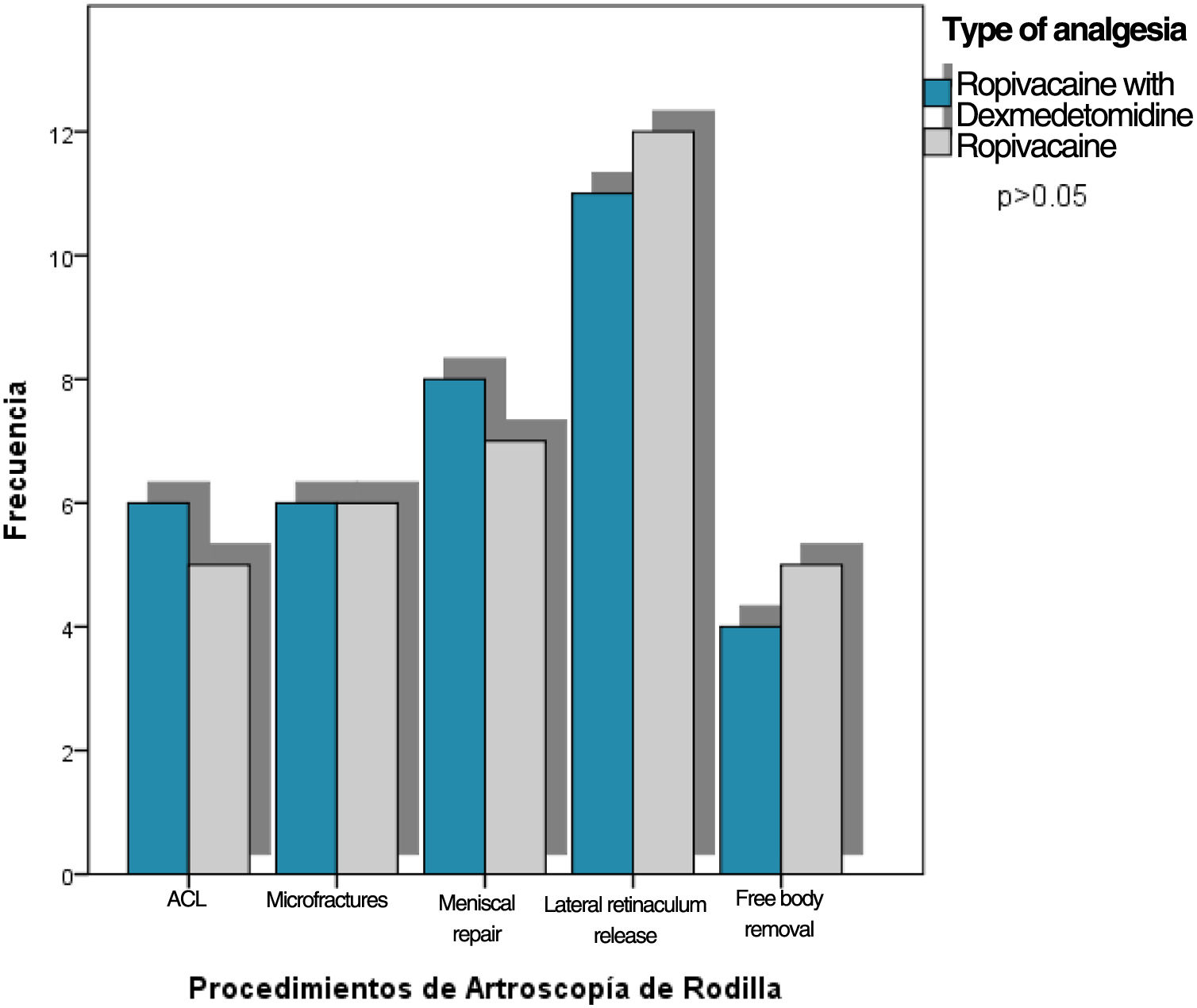
ResultsClinical characteristics were compared, with 61.4% of the general population being male and the mean age between the two groups being 39 years. In the study group [ropivacaine plus dexmedetomidine, RD], the surgical procedure duration was shorter (54min) (p=.01); likewise, 80% of the cases required a single dose of rescue analgesia (p=.03) compared to the control group [ropivacaine alone, R] (Table 1). There were no differences with regard to the procedures performed between the two groups, the most common one being lateral retinaculum release (p=.78) (Fig. 1).
Populational demographics with respect to type of analgesia.
| Ropivacaine with dexmedetomidinen=35 | Ropivacaine simplen=35 | p | |
|---|---|---|---|
| Age, years (mean, SD, 95% CI) | 39.9±9.8 (36.5–43.3) | 38.9±10.6 (35.2–42.5) | .68 |
| Sex | (n, %) | (n, %) | |
| Male | 23 (65.7) | 20 (57.1) | .46 |
| Female | 12 (34.3) | 15 (42.9) | |
| Weight, kg (mean, SD, 95% CI) | 75.3±6.7 (72.9–77.6) | 73.8±4.9 (72–75.5) | .29 |
| Duration of surgery, minutes (mean, SD, 95% CI) | 54.2±6.1 (52.1–56.3) | 58.5±8.2 (55.7–61.3) | .01 |
| Group 1 | (n, %) | (n, %) | .78 |
| ACL reconstruction | 6 (17.1) | 5 (14.3) | |
| Microfractures | 6 (17.1) | 6 (17.1) | |
| Group 2 | (n, %) | (n, %) | |
| Meniscus repair | 8 (22.9) | 7 (20) | |
| Lateral retinaculum release | 11 (31.4) | 12 (34.3) | |
| Free body removal | 4 (11.4) | 5 (14.3) | |
| Dose of rescue analgesia | (n, %) | (n, %) | .03 |
| 1 dose | 28 (80) | 20 (57.1) | |
| 2 doses | 7 (20) | 15 (42.9) | |
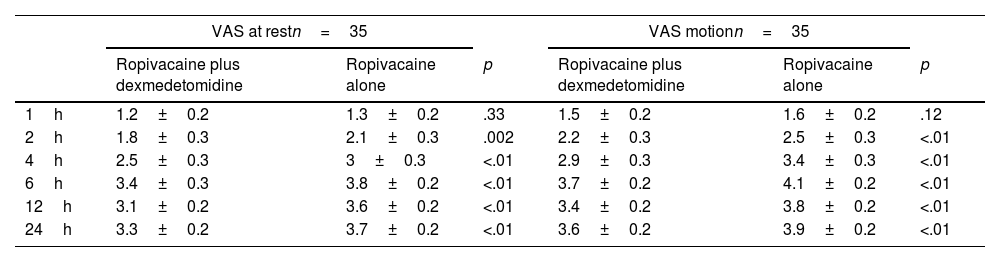
According to the pain scale (VAS) at rest and in motion, significant differences were noted starting at two hours following surgery, with pain intensity being lower in the DR study group, both at rest and in motion (Table 2).
Comparison of post-surgical pain assessment (VAS) at rest and in motion compared to the type of therapy (combination or monotherapy).
| VAS at restn=35 | VAS motionn=35 | |||||
|---|---|---|---|---|---|---|
| Ropivacaine plus dexmedetomidine | Ropivacaine alone | p | Ropivacaine plus dexmedetomidine | Ropivacaine alone | p | |
| 1h | 1.2±0.2 | 1.3±0.2 | .33 | 1.5±0.2 | 1.6±0.2 | .12 |
| 2h | 1.8±0.3 | 2.1±0.3 | .002 | 2.2±0.3 | 2.5±0.3 | <.01 |
| 4h | 2.5±0.3 | 3±0.3 | <.01 | 2.9±0.3 | 3.4±0.3 | <.01 |
| 6h | 3.4±0.3 | 3.8±0.2 | <.01 | 3.7±0.2 | 4.1±0.2 | <.01 |
| 12h | 3.1±0.2 | 3.6±0.2 | <.01 | 3.4±0.2 | 3.8±0.2 | <.01 |
| 24h | 3.3±0.2 | 3.7±0.2 | <.01 | 3.6±0.2 | 3.9±0.2 | <.01 |
Mean, SD, Student's t.
Post-surgical analgesia time was determined to be longer in the ropivacaine plus dexmedetomidine group (655min) compared to the ropivacaine alone group (318min) (p=.03). This time was longer in men (p=.76) and more than 60% of cases required a rescue dose in both sexes (p=.18). The analgesia time was shorter in those cases undergoing lateral retinaculum release and free body extraction being 364 and 385min, respectively. Conversely, analgesia time in ACL reconstruction was 515min and in microfractures it was 465min, although in those patients undergoing ACL reconstruction, 72.7% required two rescue doses. Individuals undergoing meniscus repair had the longest analgesia time (607min), with 80% requiring a single rescue dose (Table 3).
Differences in time of analgesia and rescue analgesic n=70.
| Time of analgesia (minutes) | Rescue analgesic1 dose 2 doses | ||||
|---|---|---|---|---|---|
| Median, p25–75 | p | n (%) | n (%) | p | |
| Analgesia RD | 655 (605–710) | <.01 | 28 (58.3) | 7 (31.8) | .03* |
| Analgesia R | 318 (312–326) | 20 (41.7) | 15 (68.2) | ||
| Sex | |||||
| Male | 520 (318–655) | .76 | 27 (62.8) | 16 (37.2) | .18 |
| Female | 356 (318–655) | 21 (77.8) | 6 (22.2) | ||
| ACL | |||||
| Procedure | 515 (297–560) | .60 | 3 (27.3) | 8 (72.7) | .16 |
| Microfractures | 465 (317–702) | 9 (75) | 3 (25) | ||
| Meniscus repair | 607 (315–712) | 12 (80) | 3 (20) | ||
| Release of the lateral retinaculum | 364 (321–664) | 17 (73.9) | 6 (26.1) | ||
| Free body removal | 385 (317–627) | 7 (77.8) | 2 (22.2) | ||
Finally, we stratified the study population into two groups depending on the type of arthroscopic intervention, Group 1 [ACL reconstruction and microfractures] and Group 2 [meniscus repair, lateral retinacular release, free body removal]. In both, post-surgical analgesia time was longer in the RD treatment group and was 623 and 671min, respectively, compared to the R treatment group in which analgesia duration was 313 and 325min (p-value<.001). In Group 1, rescue doses were similar between RD and R alone (p=.68), whereas, in Group 2, 91% of the RD-treated individuals required one rescue dose and in the group that received R alone, 40% required two rescue doses (p=.016) (Table 4).
Analysis stratified by duration of post-surgical analgesia and combined or single-agent therapy.
| Group 1n=24 | RDn=12 | Rn=12 | p |
|---|---|---|---|
| Mean, SD, 95% CI | Mean, SD, 95% CI | ||
| Time of post-surgical analgesia (min) | 623±83.5(570–676) | 313±14.5(303–322) | <.001 |
| Rescue analgesia | n (%) | n (%) | |
| 1 dose | 7 (58.3) | 6 (50) | .68 |
| 2 doses | 5 (41.7) | 6 (50) | |
| Group 2n=46 | RDn=23 | Rn=23 | p |
|---|---|---|---|
| Mean, SD, 95% CI | Mean, SD, 95% CI | ||
| Time of post-surgical analgesia (min) | 671±57 (647–669) | 325±20.1 (316–334) | <.001 |
| Rescue analgesia | n (%) | n (%) | |
| 1 dose | 21 (91.3) | 14 (60.9) | .016 |
| 2 doses | 2 (8.7) | 9 (39.1) | |
No side effects were reported in either group.
DiscussionArthroscopic surgery of the knee is associated with post-surgical pain of varying degrees, which is not directly proportional to the procedure performed or to the surgeon's expertise or to surgical time, although these are all factors to be considered. Consequently, controlling postoperative pain takes on importance inasmuch as it has direct repercussions on how soon rehabilitation can be initiated. Nevertheless, the fact that there is no regulation with respect to the sale and use of analgesics and anti-inflammatories has harmed health around the world. Gastrointestinal diseases are among the leading causes of mortality around the globe, the most common of which is gastritis. While this disease has a multifactorial aetiology, the of NSAIDs is a factor of significant relevance.19
Therefore, and due to the side effects resulting from non-steroid anti-inflammatories and opioids, such as gastritis, nausea, vomiting, bradycardia, pruritus, and somnolence, studies have currently been conducted with different medications being delivered directly inside the joint that provide local analgesia and decrease the appearance of said side effects.2,3 Various authors have studied the analgesic effect of intraarticular dexmedetomidine, ropivacaine, fentanyl, or buprenorphine; however, there is a paucity of head-to-head studies comparing dexmedetomidine plus ropivacaine against ropivacaine alone.16
Ropivacaine is structurally related to bupivacaine; nonetheless, given that it is less soluble in lipids, it is less toxic to the heart and central nervous system. This property together with administering it directly into the joint simultaneously with local anaesthetics lessens postoperative pain without presenting significant side effects.4
The use of intraarticular analgesics in arthroscopic surgery of knee has been documented to increase the duration of analgesia up to 10h.16 In our study, the time elapsed until the first dose of rescue analgesia was significantly greater in the RD-treated group compared to the group that received R; this duration is comparable to that reported in earlier studies.
In their study, Paul et al.15 demonstrated that the combination of 19ml of ropivacaine plus 100μg of dexmedetomidine was superior to the administration of 19ml of ropivacaine in monotherapy, in that the combination provided between quality and duration of analgesia. The number of doses of rescue analgesics received by the patients was considerably higher in the R Group in comparison to the RD Group. These results are similar to those of previous studies.15–18 Similarly, it is important to highlight that one of the most significant qualities of our study is the capacity to distinguish between major and minor surgery. Although the arthroscopy of the knee is considered a minimally invasive surgery, performing techniques on bone has never been the same as carrying out procedures on soft tissues. Nevertheless, our study enables us to see that even in the group of major surgeries, analgesia time was longer in the RD Group versus the R Group.
We found no significant differences as regards the intensity of pain at rest and in motion on the basis of the VAS assessment at 1, 2, 4, and 6h. However, at 12 and 24h, the VAS score was significantly higher in the R Group in motion.
In studies comparing single-use, non-adjuvant drugs such as those of Manuar et al.,2 ropivacaine has a significant advantage over fentanyl and dexmedetomidine in terms of analgesic duration and the need for postoperative rescue; as a result, using ropivacaine as the basis for treatment and combining it with an adjuvant is an excellent analgesic foundation. We compared this base of ropivacaine with previous excellent results in the literature and compared it with a mixture containing an adjuvant in order to obtain a better result. Dexmedetomidine has been documented to have great potential for post-surgical pain control over oral anti-inflammatory analgesics as described by Li et al.3 In some studies, such as that by Agarwal et al.,10 morphine provides extended analgesic time when used concomitantly with levobupivacaine compared to dexmedetomidine, apparently because of the slow rate of intra-articular absorption due to the low vascularity, without presenting the typical adverse effects of morphine. There are several analgesic combinations such as bupivacaine+morphine/dexmedetomidine,5,7 levobupivacaine with dexmedetomidine,4 levobupivacaine+sulphate of magnesium,8 levobupivacaine+tramadol, (10/11) dexmedetomidine+ketamine, or fentanyl (20/26) finding that the use of an analgesic plus adjuvants together have better efficacy for post-surgical pain control than the use of an analgesic alone, both applied intra-articularly. This is evident in our study in which we observe a better analgesic status in the group of patients who received the combination of ropivacaine with dexmedetomidine over that of the amide alone, despite the fact that the study groups are still small.
ConclusionsDexmedetomidine administered directly into the joint at a dose of 1μg/kg together as an adjuvant to a local anaesthetic, such as ropivacaine, enhances the quality and duration of post-surgical analgesia, reduces the use of rescue analgesics, thereby decreasing the adverse effects in patients undergoing arthroscopy of the of knee.
FundingThis work has not received any funding.
Conflict of interestsThe authors have no conflict of interests to declare.
FundingThis article does not involve any financial or personal relationship that could imply a conflict of interest. No work was done, no consultancy or funding was received, and no participation was obtained from companies or others external entities to the authors.