Cementless fixation for hip arthroplasties has increased in the last decades, particularly in younger patients. The purpose of this study was to compare the long-term results three different types of fixations in patients under 50years old.
MethodsCemented, hybrid and cementless fixations were assessed in patients under 50years old with a minimum follow-up of 8years. Loosening, demarcation, complications, and prosthesis survival were assessed. Functional analysis was performed with the modified Harris Hip Score and Visual analogue scale was collected.
ResultsFinal series consisted in 222 patients. Significant improvement was observed regarding mHHS and VAS score in each group. We observed statistically significant difference regarding demarcation between the groups (p<.001). The higher rate of acetabular and femoral stem loosening was observed in the cemented (20.0%) and hybrid (18.9%) group. The lowest prosthesis survival rate after 16 years was observed in hybrid group (p<.001).
ConclusionTotal hip replacement has good long-term clinical and functional outcomes. The lowest rate of prosthesis survival was observed in hybrid group with 84.2% after 16years.
En los últimos años se ha incrementado el uso de la fijación no cementada en artroplastia de cadera, especialmente en pacientes jóvenes. El propósito de nuestro estudio fue analizar comparativamente los resultados a largo plazo de artroplastias de cadera realizadas en pacientes menores de 50años utilizando fijación cementada, híbrida y no cementada.
MétodoRealizamos un estudio retrospectivo incluyendo adultos menores de 50años con un seguimiento mínimo de ocho años. Se confeccionaron tres grupos de estudio según la fijación (total cementada, no cementada e híbrida). La evaluación clínica/funcional fue realizada con el score modificado de cadera de Harris (mHHS) y la escala visual análoga del dolor (EVA). Registramos signos de radiolucencia, aflojamiento y supervivencia en cada grupo.
ResultadosLa serie quedó conformada finalmente por 222 pacientes. Cada grupo mostró mejoría significativa en las escalas de mHHS y EVA. Hubo una diferencia estadísticamente significativa al comparar las radiolucencias de los componentes entre los grupos (p<0,001). No observamos diferencias significativas en la calidad de cementado (p=0,17). El mayor porcentaje de aflojamiento acetabular (20,0%) y femoral (18,9%) fue observado en las artroplastias cementadas e híbridas, respectivamente. La supervivencia a 16años de seguimiento mostró que las artroplastias híbridas tienen el porcentaje más bajo, con 84,2% (p<0,001).
ConclusiónLas artroplastias en pacientes menores de 50años tienen buenos resultados clínicos a largo plazo. Los reemplazos híbridos poseen la menor tasa de supervivencia tras 16años de seguimiento.
Total hip arthroplasty in patients under 50 years of age has increased in recent decades.1 Due to the increase in life expectancy and the higher functional demands of this particular patient group, it is highly likely that revision surgery will be required at some other time in the remainder of their lives.1,2
In recent years, the use of uncemented fixation has increased worldwide, especially in young patients,3 reporting prosthetic survival rates above 90% in the long term.4–7 There are also some additional advantages, such as reduced surgical time, lower risk of thromboembolic events and, in the absence of cement, a subsequently less technically demanding revision.8
Moreover, in the early days of cemented fixation, different authors reported alarming rates of fixation failure (up to 50%) in the short term in young patients.9–11 As a result, its use was restricted to older patients and those with lower functional demand.12,13 Later, with improvements in implant designs and cementation techniques, more recent series have reported excellent prosthetic survival rates (between 85% and 95%) at more than 10years of follow-up in patients under 50years of age.9,10 Some international registries, such as the Norwegian and Finnish registries, have also reported that prosthetic survival of cemented fixation exceeds that of other types of fixation in the long term.14,15
Given this lack of consensus regarding the behaviour of the different types of prosthetic fixation in patients under 50years of age, we decided to comparatively analyse the clinical, functional and radiological results, as well as prosthetic survival in patients under 50, comparing three different fixation methods: cemented, hybrid and non-cemented. Based on our experience and on different previous studies, our hypothesis was that non-cemented fixation would present better long-term survival rates than the other two types of fixation.
MethodThe study was conducted in accordance with the ethical standards recognised by the Declaration of Helsinki and resolution 008430 of 1993 and was approved by the Institution's Ethics Committee (protocol 11262). Informed consent was obtained from the patients who participated in the study. A retrospective comparative study was conducted in consecutive patients operated on at our institution between February 2005 and January 2012. Patients aged 18–49 years who underwent primary THA for osteoarthritis of the hip and who completed a minimum follow-up of 8 years were included. Patients with a history of previous hip surgeries, septic or rheumatoid arthritis, and oncological pathology were excluded. Informed consent was obtained from the patients included in the series prior to the study.
Depending on the type of fixation used, the patients were grouped into three different categories: group A, consisting of total cemented arthroplasties; group B, with patients where hybrid fixation was used (cementless cup and cemented stem), and group C, where all arthroplasties were cementless.
The types of prostheses used in this series were:
- -
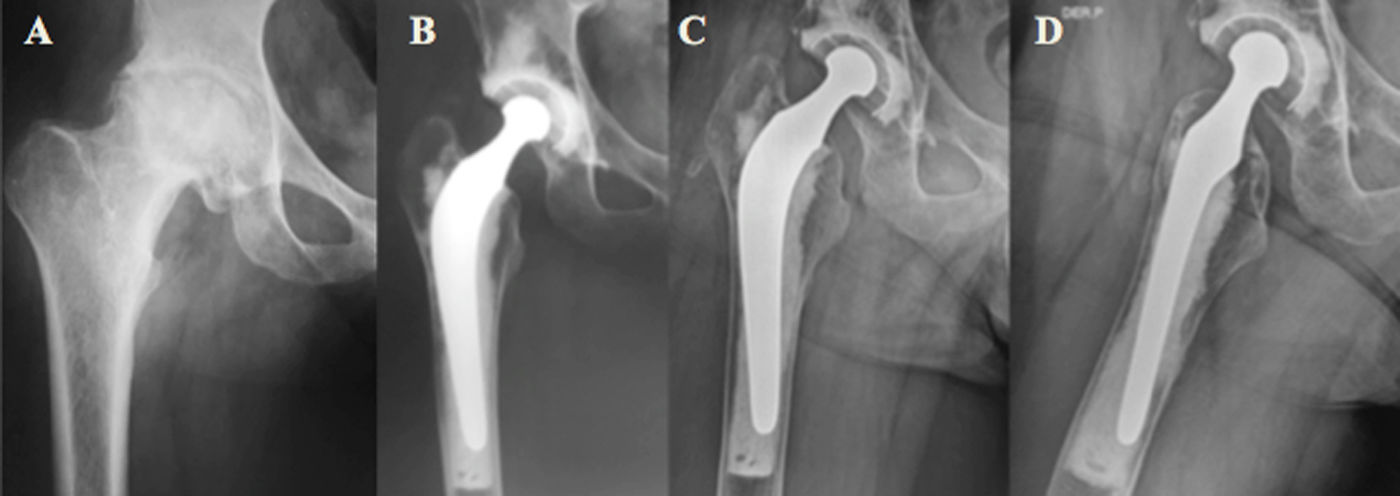
Group A: Ogee cup with cemented Charnley stem (Depuy, Warsaw, Ind, USA) (Fig. 1).
- -
Group B: Duraloc cup with cemented Charnley stem (Depuy, Warsaw, Ind, USA).
- -
Group C: Trident cup with cementless Accolade stem (Stryker, Mahaw, NJ, USA).
All surgeries were performed in a laminar air flow operating theatre under hypotensive spinal anaesthesia by the same team and using the same surgical technique. Antibiotic prophylaxis consisted of the administration of 1g (2g if the patient weighed more than 80kg) of cefazolin, 30min before the skin incision. In all cases, the Bauer anterolateral approach16 was used. Initially, acetabular reaming was performed with implantation of the definitive component and the corresponding polyethylene insert. In the case of cementing the acetabular component, this was done manually using low-viscosity cement, ensuring complete and uniform coverage of the cavity. Then, the preparation of the femoral canal was performed with progressive rasps prior to placing the definitive implant. For cemented stems, a distal plug was placed before implantation and profuse washing with physiological solution and retrograde cementation with a gun was performed.
All patients adopted the same rehabilitation protocol, performing isometric quadriceps and calf exercises on the first postoperative day and sitting on the edge of the bed. From the second day on, they began to walk with full weight, assisted by a walker. According to pain tolerance, they progressed with the assistance of two Canadian canes for 3 weeks and then completed 3 additional weeks with the use of a single cane.
Clinical analysisInformation was collected on the following variables extracted from the institution's medical records: age, sex, operated side, body mass index (BMI), and ASA grade.
Clinical/functional evaluation was carried out using the modified Harris Hip Score [mHHS])17 and the visual analogue pain scale (VAS),18 respectively. We compared the preoperative values with those of the last visit after surgery, at the end of this study.
Radiographic analysisFor radiographic analysis, we used anteroposterior (AP) and lateral (L) projections of both hips with 10° internal rotation. The appearance of radiological demarcations close to the acetabular and femoral components was classified according to the method described by DeLee-Charnley19 and Gruen.20 The quality of cementation was assessed using the Barrack classification.21
We defined acetabular loosening as the progression of radiological demarcation lines>2mm or component migration>3mm in successive controls.22 Furthermore, cemented stems were considered loosened when migration of the component or cement was observed. Loosening of uncemented stems was recorded according to the Engh and Massini classification.23
All images were taken routinely at 30days, 6 and 12months, and then annually. Data were collected by an orthopaedic surgeon trained in hip surgery.
Prosthetic complications and survivalComplications reported included dislocation; infection (according to the criteria described by the MSIS);24 periprosthetic fracture (PPF); gluteal insufficiency (defined by the presence of the Trendelenburg sign in the operated hip) and deep vein thrombosis (DVT). For the calculation of prosthetic survival, we considered revision for any cause as a cut-off point.
Statistical analysisCategorical and continuous variables were reported as frequencies or percentages and as means or standard deviation or median and interquartile range according to their distribution. The Chi-square test (χ2) or Fisher's exact method were used to evaluate qualitative variables, while the Student's t test was used for quantitative variables. The one-way ANOVA test was used to compare clinical and functional results before and after surgery during follow-up between the different groups. The Kaplan–Meier method was used for prosthetic survival analysis, and the Log-rank test (Mantel Cox) was performed to compare survival curves between study groups. We considered a p value of <.5 as statistically significant. All data were entered into an Excel® spreadsheet (Redmond, USA) and calculations were performed using GraphPad Prism® 9.0 software (La Joya, CA, USA).
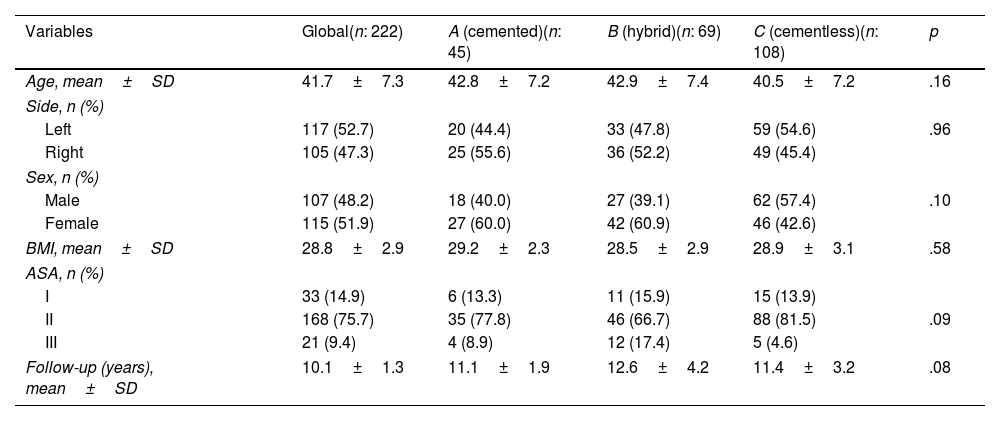
ResultsDuring the period mentioned, 233 THAs were performed in patients younger than 50years of age. Eleven were excluded from our study (4 were lost to follow-up and 7 had incomplete medical records). The series was finally comprised of 222 patients, with 107 (48.2%) male patients. Groups A, B, and C consisted of 45, 69, and 108 patients, respectively. No statistically significant preoperative differences were observed between the groups (Table 1).
Preoperative characteristics of different types of fixation and global series.
| Variables | Global(n: 222) | A (cemented)(n: 45) | B (hybrid)(n: 69) | C (cementless)(n: 108) | p |
|---|---|---|---|---|---|
| Age, mean±SD | 41.7±7.3 | 42.8±7.2 | 42.9±7.4 | 40.5±7.2 | .16 |
| Side, n (%) | |||||
| Left | 117 (52.7) | 20 (44.4) | 33 (47.8) | 59 (54.6) | .96 |
| Right | 105 (47.3) | 25 (55.6) | 36 (52.2) | 49 (45.4) | |
| Sex, n (%) | |||||
| Male | 107 (48.2) | 18 (40.0) | 27 (39.1) | 62 (57.4) | .10 |
| Female | 115 (51.9) | 27 (60.0) | 42 (60.9) | 46 (42.6) | |
| BMI, mean±SD | 28.8±2.9 | 29.2±2.3 | 28.5±2.9 | 28.9±3.1 | .58 |
| ASA, n (%) | |||||
| I | 33 (14.9) | 6 (13.3) | 11 (15.9) | 15 (13.9) | |
| II | 168 (75.7) | 35 (77.8) | 46 (66.7) | 88 (81.5) | .09 |
| III | 21 (9.4) | 4 (8.9) | 12 (17.4) | 5 (4.6) | |
| Follow-up (years), mean±SD | 10.1±1.3 | 11.1±1.9 | 12.6±4.2 | 11.4±3.2 | .08 |
ASA: Anaesthesiologist American Association; BMI: body mass index; SD: standard deviation.
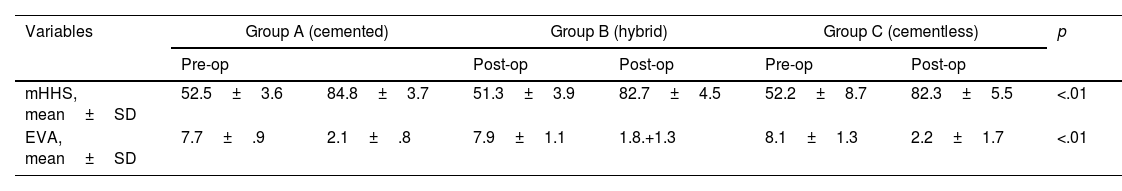
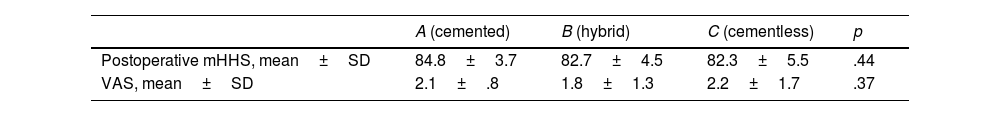
When analysing each group individually, a statistically significant improvement was observed after surgery with respect to the mHHS and VAS scales (Table 2). However, no significant differences were observed when comparing the postoperative values between the different groups (Table 3).
Comparison of the mHHS and VAS values between groups, prior to surgery and at last visit.
| Variables | Group A (cemented) | Group B (hybrid) | Group C (cementless) | p | |||
|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Post-op | Pre-op | Post-op | |||
| mHHS, mean±SD | 52.5±3.6 | 84.8±3.7 | 51.3±3.9 | 82.7±4.5 | 52.2±8.7 | 82.3±5.5 | <.01 |
| EVA, mean±SD | 7.7±.9 | 2.1±.8 | 7.9±1.1 | 1.8.+1.3 | 8.1±1.3 | 2.2±1.7 | <.01 |
mHHS: modified Harris Hip Score; VAS: visual analogue scale.
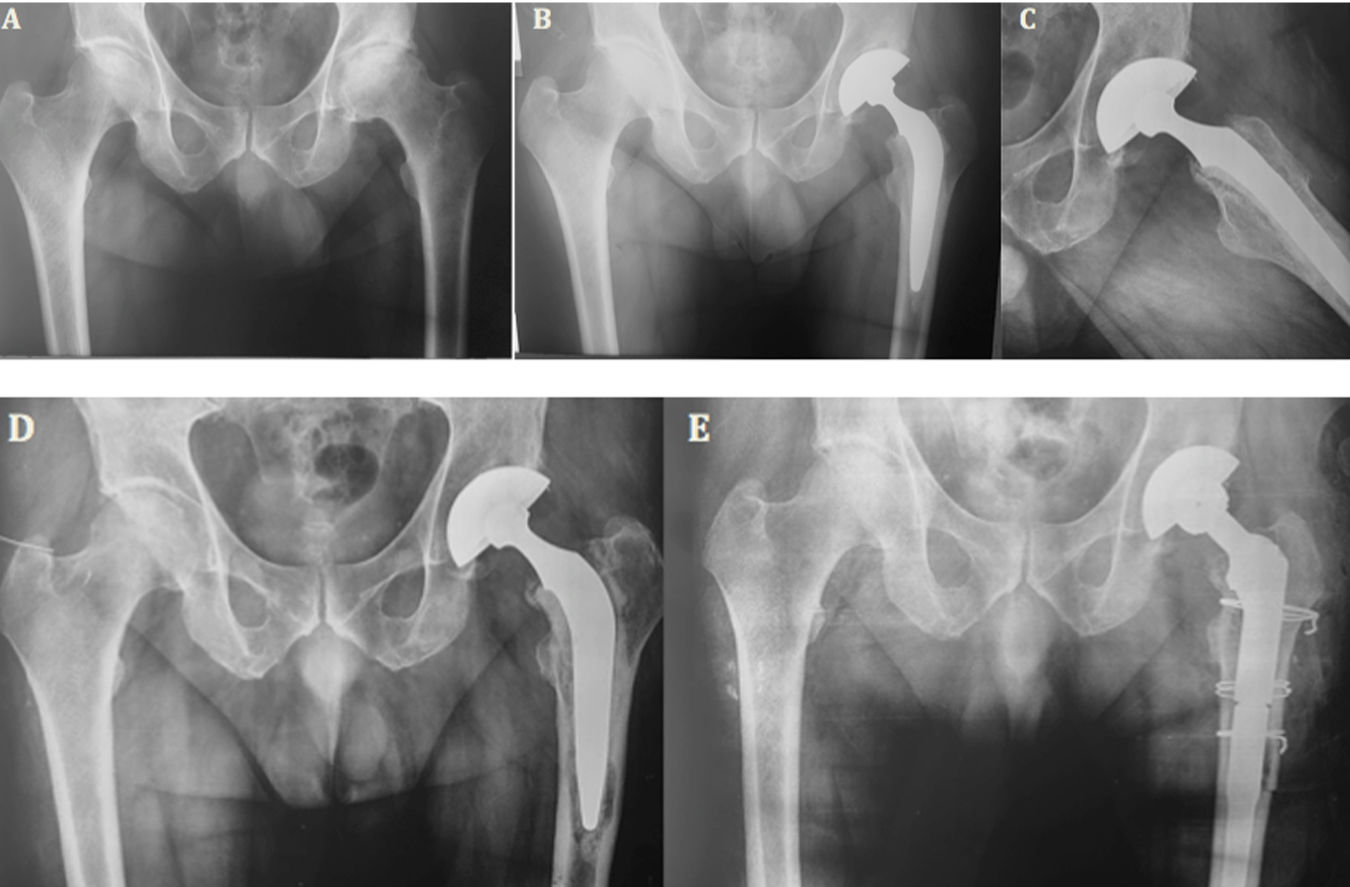
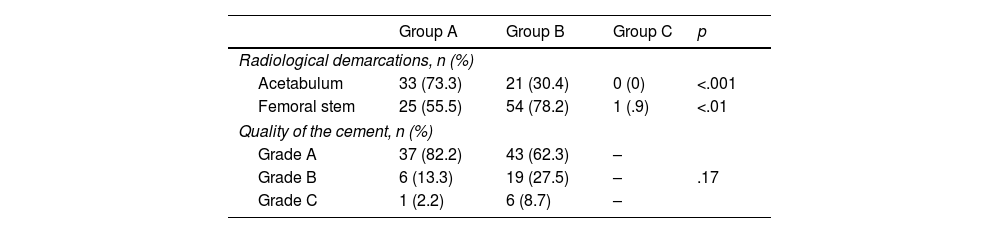
Group A (cemented) presented the highest percentage (73.3%) of cups with signs of demarcation and group B (hybrid) presented the highest rate of stems with signs of demarcation (78.2%), representing a statistically significant difference when comparing the three groups (p<.001). Cementation quality analysis raised no significant differences between groups A and B (p=.17) (Table 4; Fig. 2).
Incidence of radiological demarcation around the acetabular and femoral components and the quality of the cementation cemented.
| Group A | Group B | Group C | p | |
|---|---|---|---|---|
| Radiological demarcations, n (%) | ||||
| Acetabulum | 33 (73.3) | 21 (30.4) | 0 (0) | <.001 |
| Femoral stem | 25 (55.5) | 54 (78.2) | 1 (.9) | <.01 |
| Quality of the cement, n (%) | ||||
| Grade A | 37 (82.2) | 43 (62.3) | – | |
| Grade B | 6 (13.3) | 19 (27.5) | – | .17 |
| Grade C | 1 (2.2) | 6 (8.7) | – | |
Female patient aged 48years. (A) Preoperative AP projection: left hip osteoarthritis is observed. (B, C) Total hybrid replacement, immediate postoperative control. (D) Control at 14years: evolution with loosening of the femoral component. (E) Revision to distal fixation stem with extended femoral osteotomy.
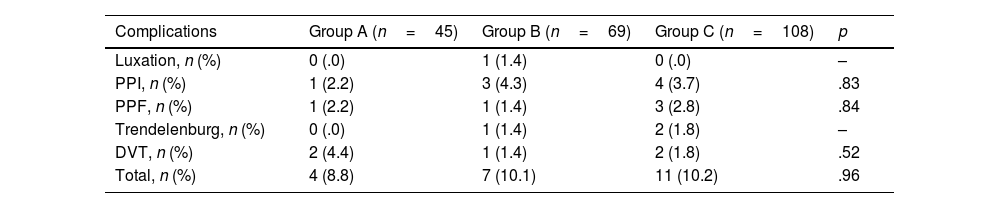
The overall complication rate was 10.0% (22 patients). No statistically significant differences were observed when comparing the complication rates between the groups (p=.58) (Table 5).
Summary of complications according to type of fixation.
| Complications | Group A (n=45) | Group B (n=69) | Group C (n=108) | p |
|---|---|---|---|---|
| Luxation, n (%) | 0 (.0) | 1 (1.4) | 0 (.0) | – |
| PPI, n (%) | 1 (2.2) | 3 (4.3) | 4 (3.7) | .83 |
| PPF, n (%) | 1 (2.2) | 1 (1.4) | 3 (2.8) | .84 |
| Trendelenburg, n (%) | 0 (.0) | 1 (1.4) | 2 (1.8) | – |
| DVT, n (%) | 2 (4.4) | 1 (1.4) | 2 (1.8) | .52 |
| Total, n (%) | 4 (8.8) | 7 (10.1) | 11 (10.2) | .96 |
DVT: deep vein thrombosis; PPF: periprosthetic fracture; PPI: periprosthetic infection.
We observed 9 (20.0%) cases of acetabular loosening in group A, of which 4 (8.8%) patients required revision.
In group B, 3 (4.3%) cases with cup loosening were observed, in patients who had undergone revision at 10, 11, and 12years, respectively. Finally, in group C, no acetabular components with signs of loosening were found.
Regarding the behaviour of the stems, 4 (8.9%), 13 (18.9%) and 2 (1.8%) patients in groups A, B and C, respectively developed signs of loosening, which was a statistically significant difference (p=.0003).
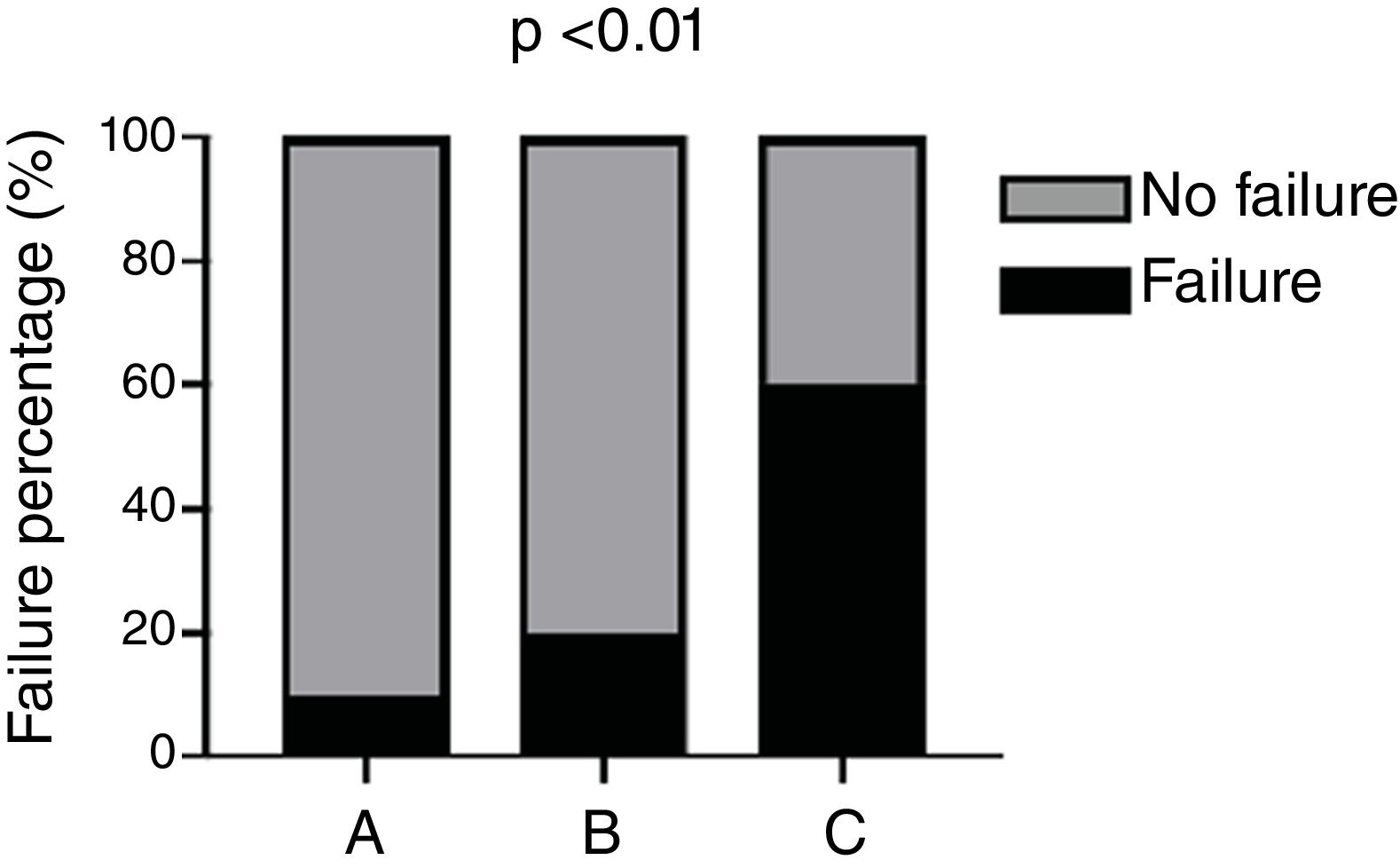
We also observed a significant association between revision and grade C cementation quality according to the Barrack classification (Fig. 3).
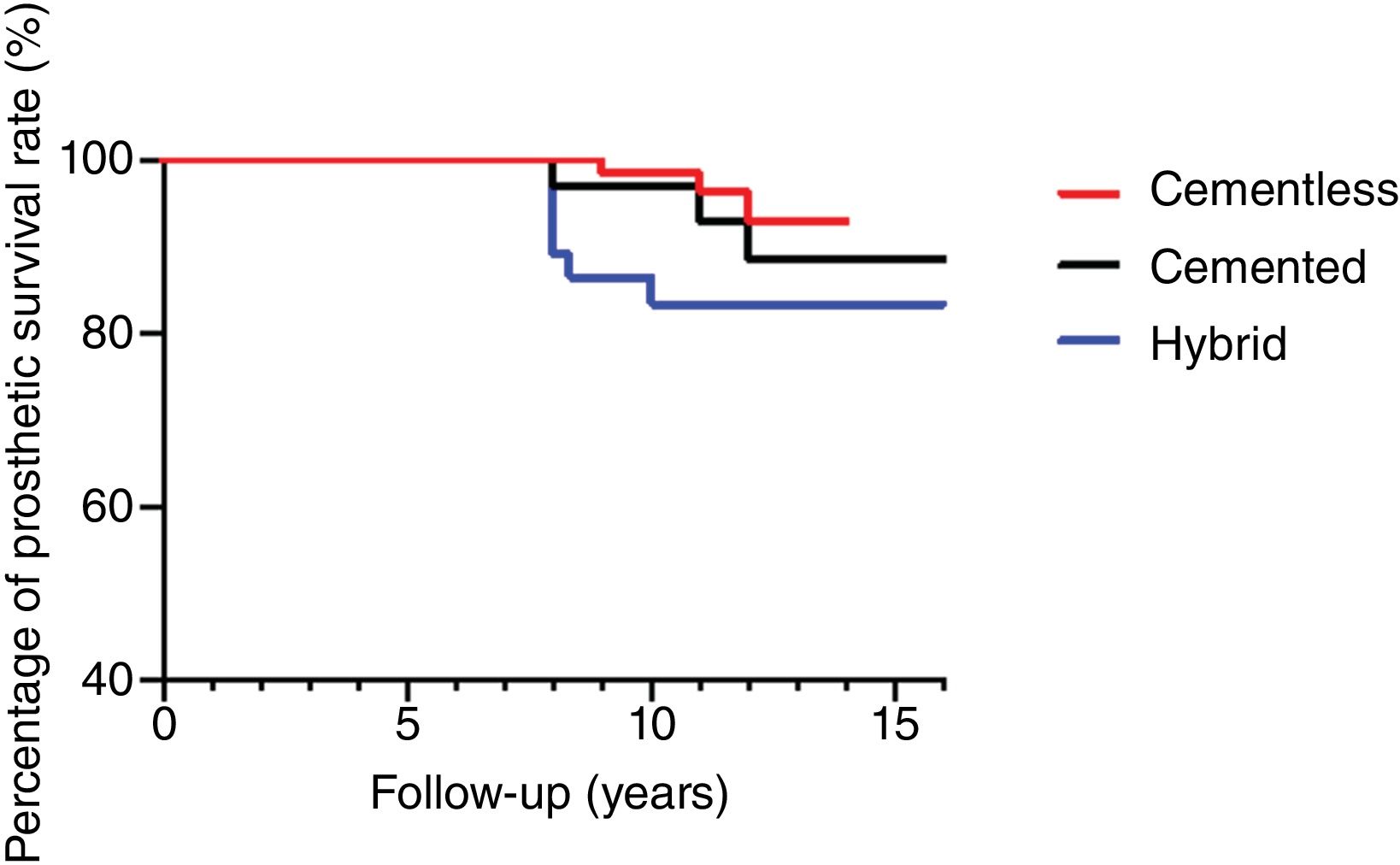
The survival analysis after 16 years of follow-up showed a significantly lower percentage (84.2%) in patients in the hybrid replacement group compared to total cemented (89.9%) and uncemented (94.6%) replacements (p<.001) (Fig. 4).
The odds ratio observed in group B regarding the risk of revision versus groups A and C was 2.44 (95% CI: 1.00–5.96).
DiscussionThe most important finding of our study was that no statistically significant long-term differences were observed when comparing clinical or functional results between total cemented replacements (group A), hybrid (group B) and uncemented (group C). However, the prosthetic survival rate at 16years was significantly lower in those with hybrid fixation compared to the rest.
Various authors have described excellent long-term functional results after hip arthroplasty regardless of the type of fixation used in patients older than 55years.25,26 In young patients and therefore with greater functional demand, there is concern that these results may be inferior in the long term.2 However, our findings demonstrated that excellent mHHS and VAS scores can be achieved in patients younger than 50 years, regardless of the fixation method (cemented, hybrid, or cementless).
With the advent of cementless components, the frequency of cemented hip replacement has decreased, and this is even more pronounced in young patients.14 The cementing of acetabular components has been associated with high rates of loosening (between 21% and 34%) in the long term.27 Furthermore, Exeter's experience in the field led to the development of studies such as that of Maggs et al.,28 who, after analysing 203 THAs, observed an aseptic loosening rate of 0% after 12.5years of follow-up.
In our study, a higher rate of acetabular loosening was observed in group A (73.3%) compared to the before-mentioned authors. We believe that one reason for this difference could be that in many of the patients (n=98) included in the study, ultra-high molecular weight polyethylenes were used instead of highly cross-linked polyethylenes, which we now know leads to early fixation failure due to particle production.29
Regarding femoral stem behaviour, the highest percentage of loosening was observed in group B (hybrid), with 18.9%. Kiran et al.26 described a loosening rate of 3.8% after evaluating 104 patients under 55 years of age who underwent cemented THA. However, Khatun's group published a loosening rate of 2.3% after 20–22 years of follow-up using the Exeter stem.30 We consider that, despite third-generation cementing, the use of a distal plug in the femoral canal, pressurisation, and retrograde cementing with a gun, there were cases where a uniform cement mantle could not be obtained around the femoral component, thus explaining the loosening rate in the present study.31
We know that a certain degree of deficiency in the cement mantle around the prosthesis could lead to early loosening.32 This was observed in our analysis, where there was a statistically significant association between patients with grade C (according to Barrack's classification) and fixation failure (p<.01). This matches that reported by Bardou–Jacquet,33 where they observed a higher risk of fixation failure in patients with grade C and D when compared to grade A and B.
Many international registries, such as the Norwegian,14 Finnish15 and that of the United Kingdom34 have reported an increase in the use of cementless components in patients under 55years of age in the last decade.
According to the Norwegian registry, regarding the overall prosthetic survival rate during the last 30 years, cemented components (70%) exceed that of uncemented components (50%). However, when adjusting for age, in patients under 55years, in the last 14years we were able to observe that this percentage is reversed with a slight superiority of uncemented components (89% versus 84%).14
The Parvizi group35 published a meta-analysis where they compared 13,059 cemented components with 13,067 uncemented components, and their conclusions were that, in terms of survival or revision, there were no statistically significant differences in the long term. This is consistent with our findings, where we observed that after 16years of follow-up, patients in group C had a higher survival rate (94.6%) than those in group A (89.9%) or B (84.2%). In addition, we did not observe significant differences when comparing the rates between hybrid and total cemented replacements.
Our study is not free from limitations, including its retrospective design and the low number of patients analysed. Although we did not perform an evaluation of the intrinsic comorbidities of the patients, we consider that as it is a series with young patients, this should not have had a direct impact on our results. We also believe that being able to compare three types of fixation frequently used in hip arthroplasty in this age group, the long-term follow-up of the series, and the fact that these were patients operated on by the same surgical team should encourage us to perform a more appropriately designed study to reinforce our conclusions.
ConclusionOur study suggests that in patients under 50 years of age, cementless fixation does not present significant clinical or functional differences in the long term compared to hybrid or total cemented or cementless fixation. However, regardless of our hypothesis, cementless THAs had the highest survival rate (94.6%), while hybrid fixation had significantly lower values (84.2%) after 16 years.
Level of evidenceLevel of evidence iii.
Ethical considerationsThis article has been approved by the Institutional Review Board.
FundingThis research did not receive any specific support from public sector agencies, the commercial sector or non-profit entities.
Conflict of interestsThe authors have no conflict of interests to declare.