The objective of this study is to compare the outcomes of using the Femoral Neck System (FNS) (DePuy Synthes®) versus the use of cannulated screws (CS) in the surgical treatment of non-displaced subcapital hip fractures.
Materials and methodsA retrospective cohort study was conducted on non-displaced subcapital hip fractures treated with CS or FNS between 2020 and 2023, with a minimum follow-up of one year. A total of 28 patients were included, 14 treated with CS and 14 with FNS. Demographic, radiological, clinical, and functional variables were analyzed.
ResultsIn the CS group, 64% were male, with a mean age of 66.5 years (SD 14.9) and an average follow-up of 22 months (range, 12-36 months). In the FNS group, 57% were male, with a median age of 60.8 years (SD 13.78) and an average follow-up of 16 months (range, 12-24 months).
Regarding functional outcomes, no significant differences were found between FNS and CS in the Harris scale: 94.21 ± 11.55 for FNS and 96.50 ± 6.9 for CS (p = 0.618).
The total postoperative complications (FNS/CS) were 7.1% versus 43%, and implant failure with conversion to total hip replacement was 0% versus 43%, both significantly higher in the CS group (p = 0.047; p = 0.016, respectively). The FNS also presented a lower rate of avascular necrosis (0% versus 11.1%, p = 0.391) and nonunion (0% versus 20%, p = 0.163), although these differences did not reach statistical significance.
ConclusionsAlthough both treatment methods, cannulated screws and the FNS, showed similar short-term functional outcomes in the management of undisplaced subcapital femoral fractures, the FNS demonstrated a significantly lower rate of complications and reoperations. These results suggest that the FNS could be considered a safer and more effective option compared to cannulated screws.
El objetivo de este estudio es comparar los resultados del uso del dispositivo Femoral Neck System (FNS) (DePuy Synthes®) frente al empleo de tornillos canulados (TC) en el tratamiento quirúrgico de fracturas subcapitales de cadera no desplazadas.
Material y métodosSe realizó un estudio de cohortes retrospectivo sobre fracturas subcapitales de cadera no desplazadas tratadas con TC o con FNS entre los años 2020 y 2023, con un seguimiento mínimo de un año. Se incluyeron 28 pacientes: 14 tratados con TC y 14 con FNS. Se estudiaron variables demográficas, radiológicas, y resultados clínicos y funcionales.
ResultadosEn el grupo TC, el 64% fueron varones con una edad media de 66,5años (DE: 14,9) y un seguimiento medio de 22meses (rango: 12-36 meses). En el grupo FNS, el 57% fueron varones, con una mediana de edad de 60,8años (DE: 13,78) y un seguimiento medio de 16meses (rango: 12-24 meses).
En relación con los resultados funcionales, no se encontraron diferencias significativas entre FNS y TC en la escala de Harris: 94,21±11,55 para FNS y 96,50±6,9 para TC (p=0,618).
Las complicaciones postoperatorias totales (FNS/TC) fueron del 7,1% frente al 43%, y el fracaso del implante con conversión a PTC fue del 0% frente al 43%, siendo significativamente superiores en el grupo de tornillos canulados (p=0,047; p=0,016, respectivamente). El FNS también presentó una menor tasa de necrosis avascular (0% frente al 11,1%, p=0,391) y seudoartrosis (0% frente al 20%, p=0,163), aunque sin alcanzar significación estadística.
ConclusionesAunque ambos métodos de tratamiento, los tornillos canulados y el sistema FNS, mostraron resultados funcionales similares a corto plazo en el manejo de fracturas subcapitales no desplazadas de cadera, el FNS presentó una tasa significativamente menor de complicaciones y reintervenciones. Estos resultados sugieren que el sistema FNS podría considerarse una opción más segura y efectiva en comparación con los tornillos canulados.
Internal fixation is the surgical treatment of choice for non-displaced subcapital or femoral neck fractures (Garden I and II), as it preserves the patient's own joint, resulting in improved long-term hip mobility and function.1–3
Currently, three-screw, cannulated screw (CS) fixation is the gold standard for treatment of non-displaced subcapital hip fractures.4 Cannulated screws provide adequate initial fixation and are commonly used due to their easy availability, low cost, and minimal invasiveness. Although CSs provide uniform load distribution, this is sometimes insufficient to prevent fracture displacement. In fact, the complication rate for CSs amounts to 36% in some studies,5 among which avascular necrosis is most prominent, due to compromised vascular supply to the femoral head. Cases of fracture nonunion or malunion have been reported due to a lack of adequate compression at the fracture site and micromotions generated during the healing process, as well as implant failures and femoral neck shortening.6,7 This has led to the search for new implants to reduce these complications.
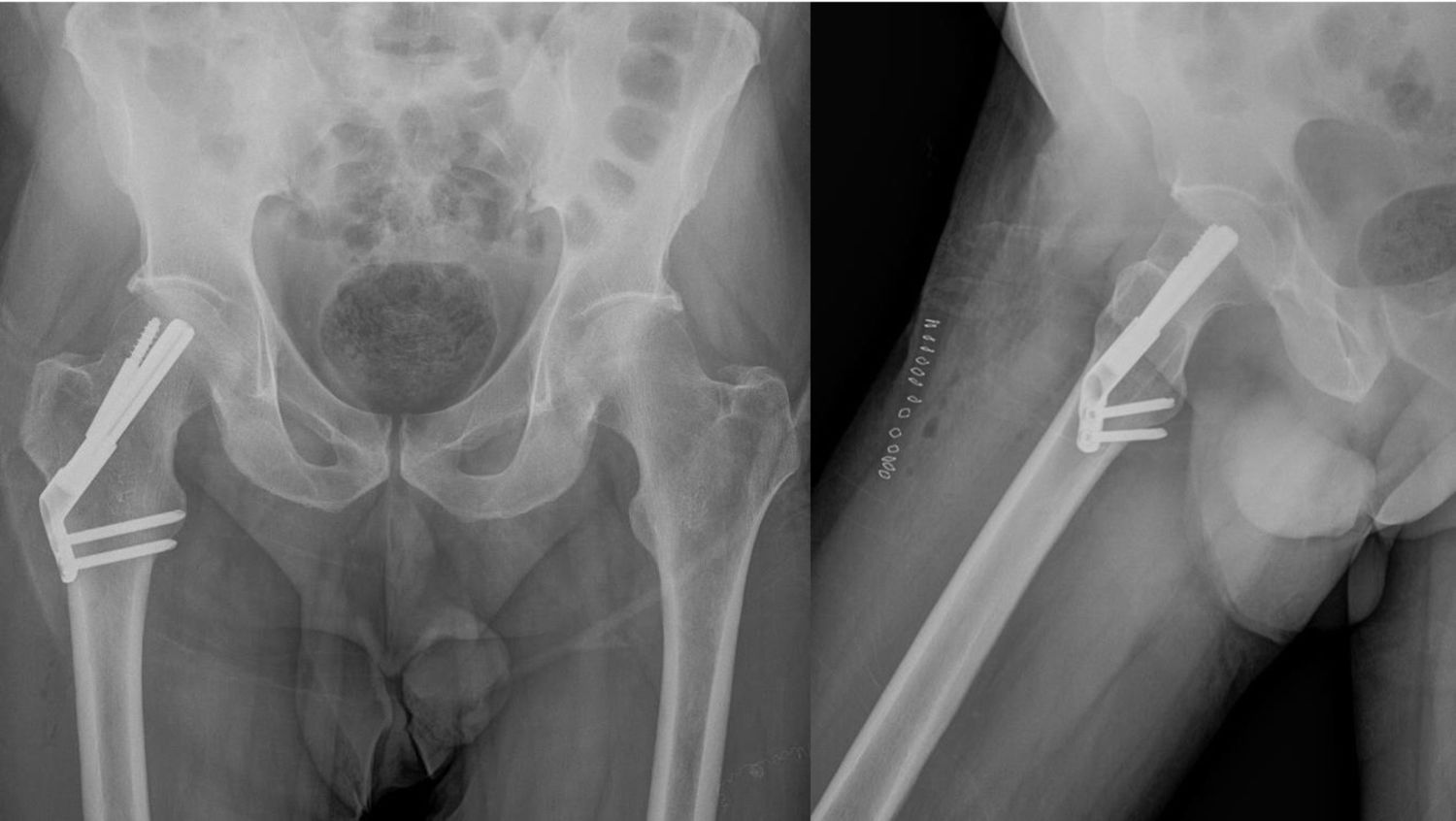
The Femoral Neck System (FNS) (DePuy Synthes®) is an alternative osteosynthesis method for subcapital hip fractures (Fig. 1). Although it has demonstrated mechanical superiority over traditional implants in anatomical studies, it is crucial to evaluate the safety and establish the patient outcomes of this new implant. Few studies analyse clinical outcomes to determine whether it is a superior alternative to CT for the management of non-displaced subcapital hip fractures in adults.8–10
The objective of this study was to compare the functional outcomes and complications after surgical treatment using CT and FNS for non-displaced subcapital hip fractures.
Material and methodsStudy design and patientsThe study was approved by the centre's Ethics Committee (Code 24/591-O_P). A retrospective study was conducted that included patients with non-displaced or impacted valgus subcapital hip fractures (Garden I or Garden II) treated at our centre between 2020 and 2023. The inclusion criteria were: patients over 18 years of age with an acute traumatic femoral neck fracture, without other associated fractures, with surgery performed within a maximum of 48h, and a minimum follow-up of 12 months after surgery.
The study included fourteen patients who underwent surgery using the FNS system with two holes in the metaphyseal plate (FNS group) and 14 patients who underwent surgery using three cannulated screws in an inverted triangle arrangement (CS group).
Surgical technique and hospital managementThe surgical technique was always performed by a senior surgeon from our centre's Fracture Unit, choosing one or the other technique based on the preference of the primary surgeon. The procedure was performed under intraspinal anaesthesia and in the supine position on a traction table.
For patients in the FNS group, an antirotation Kirschner wire was first placed to maintain fracture reduction. The wire was positioned as superior and lateral as possible to the centre of the femoral neck to avoid interfering with the placement of the initial FNS pin. A guide wire was then inserted towards the femoral neck with the assistance of a guide device, centering it in the femoral neck. After achieving a satisfactory position, the FNS pin was placed. Once the lateral femoral plate was correctly positioned, two metaphyseal locking screws were inserted after performing the guided drill holes. Finally, an antirotation screw of the appropriate length was inserted. The position of the FNS was confirmed by fluoroscopy, and the anti-rotation K-wire was removed after confirming its correct position (Fig. 2).
For patients in the CT group, K-wires were placed under fluoroscopic guidance, forming an inverted triangle. Once properly positioned, three cannulated, partially threaded screws were inserted following the direction of the wires to fix the fracture (Fig. 3).
After the procedure, the patient was transferred to the Traumatology Department, where a postoperative follow-up X-ray was performed. All patients began ambulating the day after surgery.
Data collectionBaseline patient characteristics were recorded: sex, age, history of osteoporosis, walking aids requirements, and other relevant medical history. Fractures were classified according to the Garden classification. Laboratory and clinical variables were collected upon admission (pre- and postoperative haemoglobin), time to surgery, and total hospitalisation. In addition, variables were recorded during postoperative follow-up: presence of femoral neck shortening on follow-up radiographs; radiological signs of avascular necrosis; implant failure (within the first three months); nonunion (after 6 months); need for osteosynthesis hardware removal; need for reoperation, and total complications. Finally, variables were collected at the end of each patient's follow-up: months of follow-up, presence of inguinal pain, joint balance, need for walking aids, and functional outcome measured using the modified Harris Hip Score at 6 months.
Statistical methodsStatistical analysis was performed using SPSS 20.0 software (IBM, Armonk, NY, USA). Quantitative variables were expressed as means and standard deviations for normal distributions, or as medians and interquartile ranges (p50 [p25, p75]) for non-normal distributions. Comparisons were performed using the Student's t test and the Mann–Whitney U test. Categorical data were expressed as absolute frequencies (n) and percentages (%), and comparisons were performed using the Chi-square test. A p value less than .05 was considered statistically significant.
ResultsIn the cannulated screw fixation group (CS group), 36% were men and 64% were women, and the mean age was 66.5 years (SD 14.9); in the FNS fixation group (FNS group), 57% were men and 43% were women, and the mean age was 60.85 years (SD 13.78). In the CS group, 36% of patients had a diagnosis of osteoporosis prior to the fracture (BMD<−2.5 SD), and in the FNS group, 21%.
In the CS group, 50% of fractures were Garden I and 50% Garden II, while in the FNS group, 21% were Garden I and 79% Garden II.
Surgery was performed within 48h of fracture diagnosis in all cases. The mean follow-up time in the CT group was 22 months (range 12–36 months), and in the FNS group it was 16 months (range 12–24 months).
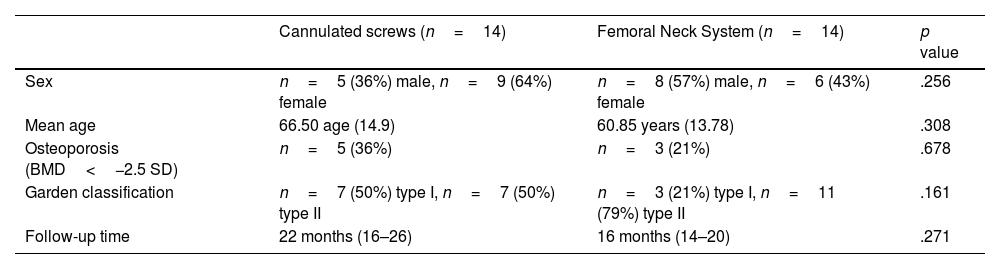
Demographic variables are shown in Table 1.
Demographic characteristics of both study groups.
| Cannulated screws (n=14) | Femoral Neck System (n=14) | p value | |
|---|---|---|---|
| Sex | n=5 (36%) male, n=9 (64%) female | n=8 (57%) male, n=6 (43%) female | .256 |
| Mean age | 66.50 age (14.9) | 60.85 years (13.78) | .308 |
| Osteoporosis (BMD<−2.5 SD) | n=5 (36%) | n=3 (21%) | .678 |
| Garden classification | n=7 (50%) type I, n=7 (50%) type II | n=3 (21%) type I, n=11 (79%) type II | .161 |
| Follow-up time | 22 months (16–26) | 16 months (14–20) | .271 |
Absolute values (n) and percentages (%), and comparisons were performed using the Chi-square test. A p-value of less than 0.05 was considered statistically significant.
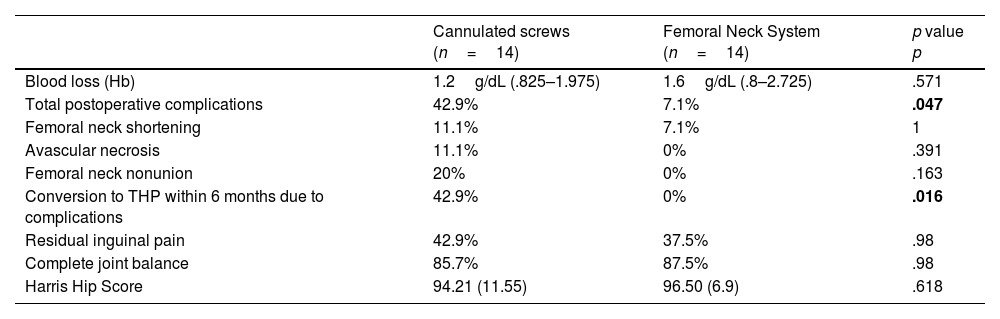
FNS presented a 7.1% rate of total postoperative complications compared to 42.9% for CT at the end of follow-up (p=.047). No FNS patient required subsequent conversion to THR in the first six months, compared to 42.9% for CT (p=.016).
The remaining variables did not show significant differences (CT vs. FNS): avascular necrosis of the femoral head (Fig. 3) (0% vs. 11.1%; p=.391); Femoral neck nonunion (0% vs. 20%; p=.163); residual groin pain (42.9% vs. 37.5%, p=.98); complete joint balance (85.7% vs. 87.5%, p=.98); blood loss or difference (measured in haemoglobin levels g/dL) before and after surgery (median 1.6g/dL vs. median 1.2g/dL; p=.571); and presence of femoral neck shortening on follow-up radiographs (7.1% vs. 11.1%; p=1).
Regarding functional outcomes, no significant differences were found on the Modified Harris Hip Score: mean FNS 94.21 (SD 11.55) versus mean CS 96.50 (SD 6.9); p=.618.
A summary of the variables measured and their statistical significance is shown in Table 2.
Comparison of the variables studied between both groups, and their statistical significance.
| Cannulated screws (n=14) | Femoral Neck System (n=14) | p value p | |
|---|---|---|---|
| Blood loss (Hb) | 1.2g/dL (.825–1.975) | 1.6g/dL (.8–2.725) | .571 |
| Total postoperative complications | 42.9% | 7.1% | .047 |
| Femoral neck shortening | 11.1% | 7.1% | 1 |
| Avascular necrosis | 11.1% | 0% | .391 |
| Femoral neck nonunion | 20% | 0% | .163 |
| Conversion to THP within 6 months due to complications | 42.9% | 0% | .016 |
| Residual inguinal pain | 42.9% | 37.5% | .98 |
| Complete joint balance | 85.7% | 87.5% | .98 |
| Harris Hip Score | 94.21 (11.55) | 96.50 (6.9) | .618 |
Internal fixation of a non-displaced subcapital hip fracture with three cannulated screws offers several advantages, such as minimal soft tissue damage, good functional outcomes in short- and medium-term follow-up, and a low associated cost. Furthermore, the material is readily available. This has led to its emergence as the most common treatment technique.11,12
Notwithstanding, several studies5–7 have demonstrated a high complication rate associated with this implant. When comparing different fixation systems, the implant with cannulated screws has been shown to have less overall resistance to superior-inferior shear stress at the fracture site, leading to displacement of the bone.13 It has also been shown that the axial force and load cycles supported by a CT fixation system are lower and more likely to fail.14 This implant failure leads to significant complications for the patient, such as nonunion, avascular necrosis, peri-implant fracture, or femoral neck shortening, negatively impacting the patient's functional outcome and potentially leading to reoperations and conversion to total hip arthroplasty.15
Recent studies5,8,9 suggest that treatment with the new FNS implant could provide greater biomechanical stability than the use of cannulated screws, offering improved rotational and angular stability of the fixation, thereby reducing the associated complication rate and the need for reoperation. Stoffel et al. compared the biomechanical behaviour of the FNS system versus three cannulated screws in fractures with a vertical path, demonstrating a lower rate of femoral neck shortening and greater support of loading cycles until implant failure.16 The FNS implant demonstrated greater stability, decreasing the inter-fragmentary sliding distance, as well as compressive and shear stresses when the implant pin tip was placed subchondral rather than centred in the femoral head.17
Blood loss was slightly lower in the CS group compared to the FNS group. Yan et al., in their 2021 study, as well as other authors,18–21 showed significantly less blood loss in the CS group. This could be explained by the fact that the FNS technique generally requires a larger incision, approximately 4–5cm, to insert the plate,22 while the CS technique requires a smaller incision, approximately 2.7cm.23 This parameter did not translate into subsequent medical complications for the patients in our series or for those included in the studies reported in the literature.
Postoperative complications during the total follow-up period were an important indicator of safety with both fixation methods. Our study demonstrated superiority of FNS over CS by comparing the number of total complications or implant failures with subsequent conversion to THR in the first 6 months. The groups of Yan et al.,10 and other authors24–26 showed similar results. Thus, these results, both in the literature and in our study, seem to demonstrate that the mechanical superiority of FNS translates into a lower rate of mechanical complications and implant failure.
Previous studies describe a 19% nonunion rate for femoral neck fractures fixed with CS, while the nonunion rate for fractures treated with internal fixators that provide angular stability was 8%.27,28 In our study, we found no significant differences when comparing both groups regarding the development of femoral neck nonunion. Yan et al.,10 Hu et al.,19 Zhou et al.,21 and Zhang et al.26 also did not show any differences when comparing this variable. This may be explained by the smaller number of patients involved in the study.
Finally, a favourable trend was observed in the Harris Hip Score in the FNS group compared to the CS group. Both Tang et al.,25 and Hu et al.19 had previously reported higher mean Harris Hip Score scores for FNS fixation than for CS fixation. This may be due to the fact that the number of patients who developed complications, more frequent in the CS group, was crucial in the comparison of the scale scores.
The main limitations of our study were the small sample size, which was limited by the time of implementation of the FNS in our centre; the retrospective nature of the study and therefore the lack of treatment randomisation; the follow-up time that can limit the detection of long-term complications was different for both groups, and the presence of more than one surgeon performing the surgical techniques.
ConclusionAlthough both treatment methods, cannulated screws and the FNS system, showed similar short-term functional results in the management of non-displaced subcapital hip fractures, the FNS system had a significantly lower rate of complications and re-interventions. These results suggest that the FNS system could be considered a safer and more effective option compared to cannulated screws. However, additional randomised studies with long-term follow-up are essential to validate these findings and evaluate their long-term applicability in clinical practice.
Level of evidenceLevel of evidence iv.
Ethical considerationsThis study did not require animal or human experimentation and was approved by the Ethics Committee of the Clínico San Carlos in Madrid.
FundingNo funding was requested for this study.
Conflict of interestsThe authors have no conflict of interests to declare.