In light of the variability observed in clinical practice and the lack of consensus among professionals, we wish to share our perspective, grounded in scientific evidence and our clinical experience, on the management of displaced metaphyseal distal radius fractures in prepubertal patients.
Recent reviews on the treatment of this type of fracture have reached conclusions that should be shared, both to improve clinical decision-making and to directly benefit patients. While the remarkable potential for bone remodelling in children is well recognised, the idea that many of these fractures can be treated without manipulation or reduction represents a major shift in therapeutic strategy. This change is not always easily adopted, either by clinicians or by families, who are often surprised when offered a less interventional approach. However, the current scientific evidence is clear: immobilisation without reducing the bayonet apposition, provided coronal and sagittal alignment are acceptable, avoids overtreatment, reduces complications and costs, and achieves equivalent—or even superior—functional outcomes.
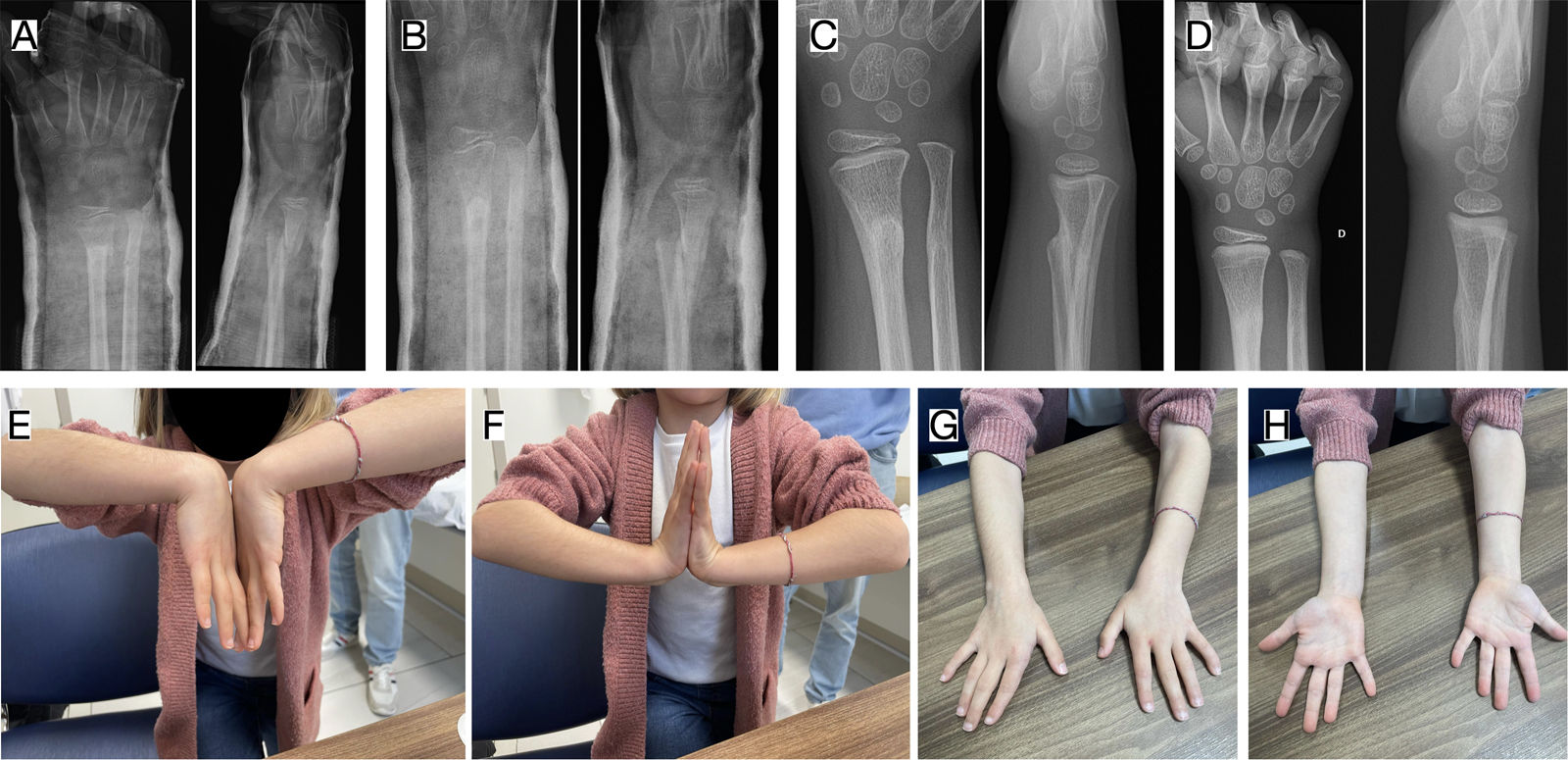
As specialists in a nationally designated Reference Center for Pediatric Orthopaedics and Traumatology, we frequently treat children with overriding metaphyseal distal radius fractures, with bayonet apposition, who have undergone multiple reduction attempts under sedation or anesthesia at other centers—often repeatedly, due to unsatisfactory reductions or loss of alignment. These fractures are often stabilised using Kirschner wires, or in some cases via open reduction and plate fixation. Many of these patients seek a second opinion and present with swelling pain, or even potential risk of compartment syndrome due to excessively tight casts or immobilisation in extreme, unnecessary positions (Fig. 1). Such practices, still common in many departments and often extrapolated from adult fracture care, contrast sharply with recent evidence and accumulated clinical experience, both of which increasingly support a more conservative approach in preadolescent children.
Clinical case of a 6-year-old patient with a displaced and overriding distal radial metaphyseal fracture treated at a different centre. (A) Initial X-ray after accidental trauma, showing an overriding fracture. (B) Follow-up with closed cast after initial reduction at another centre. Consultation the following day due to severe pain and digital swelling. (C) Follow-up after 10 days, showing loss of reduction. (D) X-ray after re-manipulation and placement of a cast in extreme volar flexion; as reduction was not achieved, the family were offered surgical treatment.
In our routine practice, we explain to families that these fractures can heal favorably without reduction. We apply an “in situ” cast, ensuring correct coronal and sagittal alignment without attempting to correct the shortening. Our experience, consistent with the literature, shows that these patients exhibit remarkable remodelling capacity, resulting in favourable clinical, radiological, and functional outcomes (Fig. 2). This approach avoids unnecessary anesthesia, painful manipulations, and surgical risks, thereby reducing the child's distress and the likelihood of complications. When families understand the reasoning behind and are shown clinical examples with favorable outcomes, they are often deeply appreciative of this alternative.
Same clinical case as in Fig. 1, a 6-year-old patient with a displaced and overriding distal radial metaphysical fracture initially treated at another centre. After surgery had been suggested, she came to our centre for a second opinion. (A) The cast was removed and a non-reducing cast applied, with adequate coronal and sagittal alignment. (B) Follow-up at 5 weeks showed partial consolidation, so the cast was removed and a semi-rigid wrist brace applied. (C) Follow-up X-ray at 3 months, showing complete consolidation and progressive remodelling. (D) Follow-up X-ray at 6 months, showing complete remodelling. (E–H) Clinical images at 6 months with complete mobility in flexion–extension and pronosupination.
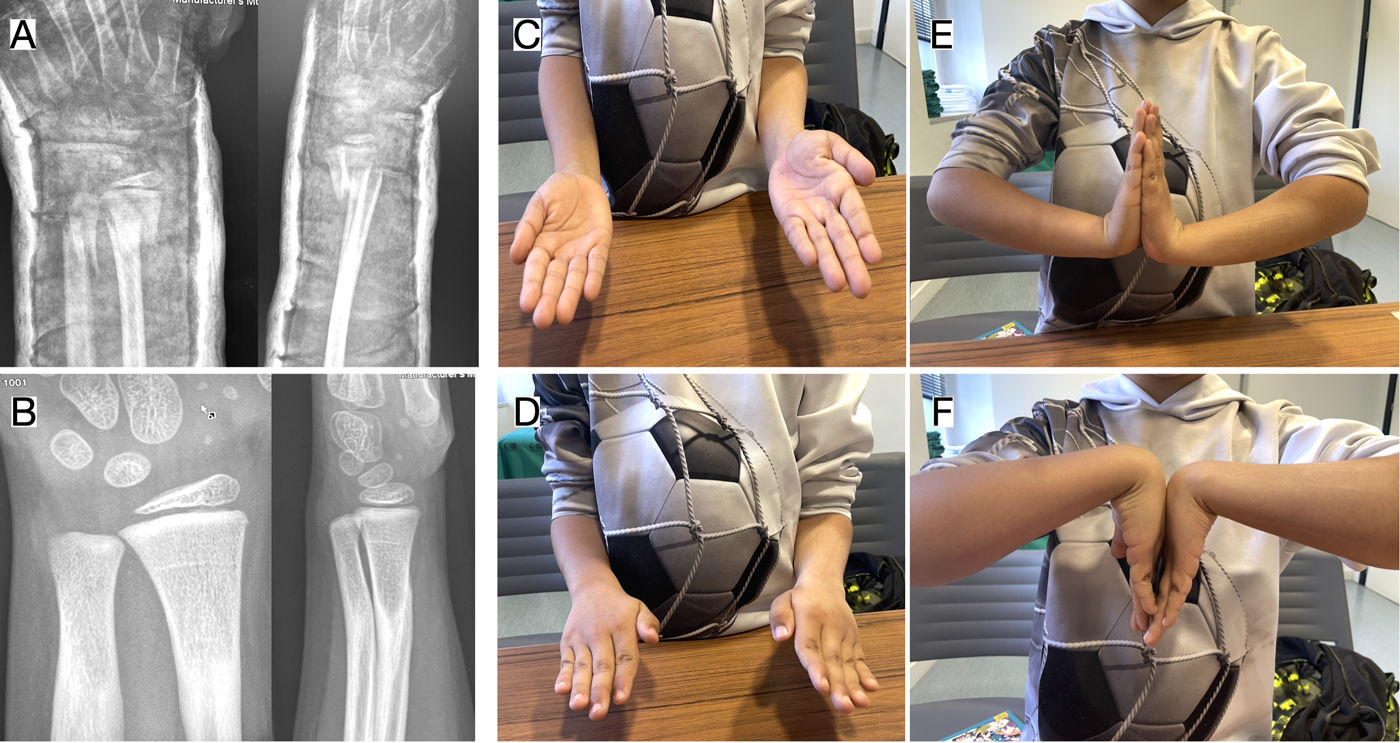
In some cases, however, families prefer that we attempt a reduction under sedation in the emergency department. In such situations, we discuss the case thoroughly and explain in advance that if the reduction is unsuccessful or if the fracture subsequently displaces, surgery will not be necessary for another closed reduction and pin fixation, let alone an open reduction with plate fixation. While families may initially be hesitant, adequate information, evidence-based reassurance, and examples from similar cases usually help them accept the more conservative approach. Detailed counselling, close follow-up, and confidence in the natural healing process often result in these families becoming among the most satisfied (Fig. 3).
(A) Distal radius fracture in an 8-year-old child treated with a non-reduction cast, ‘as is’, with adequate coronal and sagittal alignment. (B) Follow-up at 5 months post-fracture with complete consolidation and remodelling, with adequate alignment. (C–F) Range of wrist mobility in complete supination, pronation, flexion, and extension.
Our experience aligns with the scientific literature. Crawford et al. were the first to question the need for reduction, presenting a prospective series of 51 children treated without reduction or sedation, with excellent functional results and high family satisfaction.1,2 Subsequent high-quality studies, including that by Laaksonen et al., compared conservative treatment with reduction and fixation, reporting no clinical or radiological differences but a higher complication rate in the surgical group.3 Similarly, Marson et al. reported very favorable outcomes with straight casting in bayonet position, without reduction or surgery, and a lower rate of residual deformity and stiffness compared to operative treatment.4
In 2024, our group published a systematic review and meta-analysis including these studies, concluding that anatomical reduction is not necessary in children under 11 with displaced distal radius metaphyseal fractures in bayonet position. All patients treated without reduction healed adequately, with good radiological alignment, significantly fewer complications, lower reintervention rates, and less residual stiffness.5
At least five randomised clinical trials are currently underway comparing the two therapeutic strategies, reflecting growing interest in this paradigm shift. Although the final results have not yet been published, some participating centres have already shared preliminary data that further support the conservative approach. Meanwhile, we believe there is already sufficient evidence to change clinical practice and avoid unnecessary interventions in this age group.
For all these reasons, we believe it is essential to disseminate this approach among all professionals involved. Avoiding unnecessary reductions, reoperations, and surgeries in fractures that we know, through evidence and experience, can heal satisfactorily without intervention is an achievable and desirable goal. By providing clear communication, clinical examples, and support from the literature, we can help families understand the value of a growth-respectful, less invasive, and cost-effective strategy that achieves equal or better outcomes. Otherwise, many children will continue to undergo aggressive reductions or even surgeries simply due to lack of awareness or confidence in a conservative alternative that, in these cases, could be the first-line treatment.
Level of evidenceLevel V evidence.
Ethical approvalThis letter does not constitute a clinical study. It did not involve systematic data collection or intervention on patients and therefore did not require approval by a Medicinal Research Ethics Committee (CEIm). The clinical cases presented form part of routine healthcare practice. The images have been fully anonymised, and informed consent has been obtained from the patients’ legal guardians for their publication.
FundingNone of the authors has received payments, funding, or other benefits from commercial entities linked to the subject matter.
Conflict of interestsThe authors have no conflict of interests to declare.