Ankle sprains are a common musculoskeletal injury, with 10–30% of cases potentially progressing to chronic lateral ankle instability. In this context, a higher prevalence of talar osteochondral lesions (TOLs) has been observed. This study aims to confirm the association between chronic lateral ankle instability and TOLs, while also evaluating lesion location, severity, and morphology based on the Raikin, ICRS, and Hepple classifications.
Material and methodsA multicenter, cross-sectional, observational study was conducted in 7 Spanish hospitals. Patients with MRI-confirmed TOLs were included and subsequently evaluated arthroscopically. Clinical, morphological, and topographic variables were collected. The integrity of the anterior talofibular ligament (ATFL) was assessed through arthroscopy and clinical testing to determine the presence of chronic lateral ankle instability. Lesions were classified using the Hepple, Raikin, and ICRS systems.
ResultsAmong the 42 patients with TOLs, those with recurrent ankle sprains, positive anterior drawer test, and positive talar tilt test showed significantly more severe lesions (p<0.05). Although ATFL rupture was more frequent in patients with severe lesions, this finding did not reach statistical significance. As a secondary finding, medial osteochondral involvement was more common in female patients (p=0.006), and patients without ATFL rupture exhibited a significantly larger chondral surface area affected (p<0.05).
ConclusionThis study demonstrates a statistically significant association between chronic lateral ankle instability and TOL severity, particularly in patients with recurrent sprains and positive clinical tests. Interestingly, greater chondral surface involvement was found in patients without ATFL rupture. A higher frequency of medial lesions was observed in women, though no clear correlation with lesion severity was identified.
Los esguinces de tobillo son una afección frecuente que pueden evolucionar a inestabilidad crónica lateral de tobillo en un 10-30% de los pacientes, y se ha observado una mayor prevalencia de lesiones osteocondrales talares (LOT) en este contexto. Este estudio busca confirmar dicha asociación analizando, además, la localización, el grado y la morfología de las lesiones según las clasificaciones de Hepple, Raikin e ICRS.
Material y métodosEstudio multicéntrico, observacional, de corte transversal analítico, que incluyó a pacientes con LOT confirmadas por RM y evaluadas artroscópicamente en siete hospitales españoles. Se recogieron variables clínicas, morfológicas y topográficas. Se analizó la asociación con la inestabilidad crónica lateral de tobillo, valorando la integridad del ligamento talofibular anterior (LTFA) por artroscopia y pruebas clínicas. Se aplicaron las clasificaciones de Hepple, Raikin e ICRS.
ResultadosEn este estudio con 42 pacientes con LOT se observó que los esguinces de repetición, el test de cajón anterior y el test de inversión positivos, se asociaron con LOT más severas (p<0,05); aunque la lesión del LTFA fue más frecuente en LOT severas, no alcanzó significación estadística. Como hallazgo secundario, se encontró una mayor afectación osteocondral medial en mujeres (p=0,006), y que los pacientes sin lesión del LTFA presentaban lesiones de mayor superficie condral (p<0,05).
ConclusiónEl estudio confirma una asociación estadísticamente significativa entre la inestabilidad crónica lateral de tobillo y la severidad de las LOT, especialmente en pacientes con esguinces de repetición y pruebas clínicas positivas. Los casos sin lesión del LTFA presentaron mayor extensión de lesión condral. Se observó una mayor frecuencia de lesiones mediales en mujeres, sin correlación clara con la gravedad.
Ankle sprains are a common condition that primarily affects the lateral ligament complex of the ankle, particularly the anterior talofibular ligament (ATFL). This ligament is the weakest in the complex and therefore the most frequently injured, followed by the calcaneofibular ligament.1
Most acute sprains are managed with conservative treatment. However, 30–40% of patients may experience chronic discomfort, such as pain, stiffness, weakness, or instability, and up to 10–30% progress to chronic ankle instability.2,3
Osteochondral lesions of the talus are rare, with and estimated incidence of 2.08 cases per 100,000 people per year, according to an extensive review of health system databases. However, the incidence is higher in the context of ankle fractures or sprains.4
Ankle ligament injuries account for between 10% and 30% of all sports injuries.5
The main objective of this study was to determine and confirm the possible association between chronic lateral ankle instability and the presence of osteochondral lesions of the talus in our population. Secondary objectives included analysing whether this association varies according to the lesion's topographical location according to Raikin's classification system, and its degree according to the International Cartilage Regeneration & Joint Preservation Society (ICRS) arthroscopic classification system, in relation to the presence or absence of instability. Additionally, a detailed morphological characterisation of the identified lesions was performed.
Material and methodsThis is a multicentre, cross-sectional analytical study involving the ad hoc collection of variables. The foot and ankle units of the trauma and orthopaedic surgery departments of seven hospitals in Spain were included, involving a total of eight surgeons.
Patients of both sexes, aged between 18 and 65 years, with osteochondral lesion of the talus confirmed by magnetic resonance imaging (MRI) and who were evaluated by arthroscopic ankle surgery, after signing the informed consent form, were included. Patients with hyperlaxity and/or relevant comorbidities (uncontrolled diabetes, cardiovascular disease, rheumatic disease, severe hindfoot osteoarthritis, or structural misalignment) were excluded to avoid confounding factors. Patients with a history of previous arthroscopy or ligament repair were also excluded, since in these cases the presence of a ligament lesion would already have been assessed in these cases.
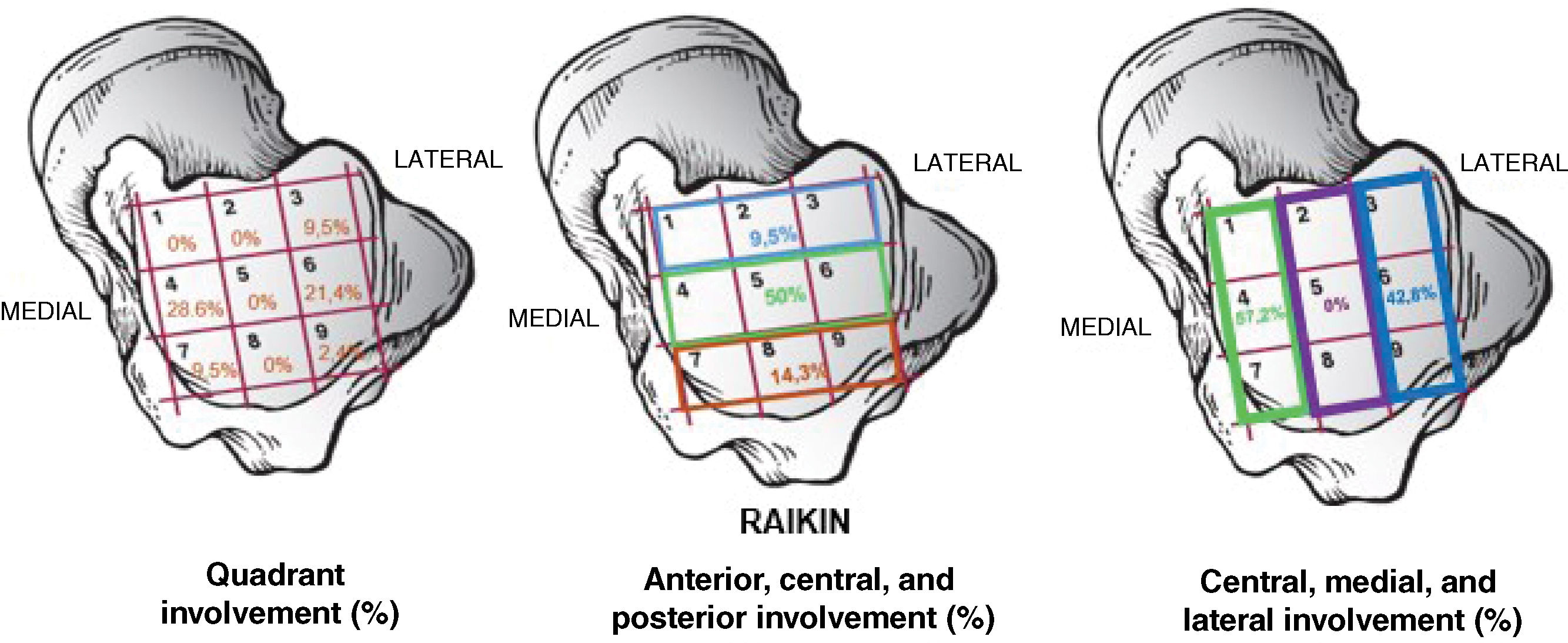
During the preoperative visit, demographic variables were collected for each patient, including age, sex, body mass index (BMI), and laterality. A detailed medical history was also taken, noting the presence of recurrent sprains, feeling of joint failure, or locking. The physical examination included stability assessments using the anterior drawer test and the varus stress test. The T2/STIR MRI scan was evaluated, and injuries were classified according to the Hepple scale, with the size of each lesion determined in square centimetres. The lesion's topographical location was recorded according to the Raikin–Elías quadrant classification system, which differentiates between medial lesions (quadrants 1, 4, and 7) and lateral lesions (quadrants 3, 6, and 9).
In the intraoperative phase, during ankle arthroscopy, osteochondral lesions were classified using the International Cartilage Repair Society (ICRS) system, and divided into four grades according to the depth of cartilage involvement. For the purposes of analysis, an ad hoc binary categorisation was created: mild lesions (ICRS 1A, 1B, and 2) and severe lesions (ICRS 3A to 4B). Finally, the integrity of the lateral ligament complex and associated lesions was assessed.
An a priori power analysis was performed to calculate the minimum sample size required to detect a 5% effect size at a one-sided significance level of <5%. In this pilot study, it was estimated that approximately 25% of patients without ATFL lesion would have grade 3A or higher chondral involvement, compared to an estimated 70% of patients with ATFL lesion. Assuming 80% statistical power, an alpha error of 5%, and an estimated ratio of 2:1 between patients with and without ATFL lesion, it was calculated that at least 42 patients (28 with lesion and 14 without) would need to be selected. Fleiss's correction was not applied, as sample losses were not considered in the study design.
Data analysis was performed using SPSS® 20.0 software (Armonk, NY, USA). Continuous variables were presented as median±interquartile range, while categorical variables were expressed in terms of counts and percentages.
The sample was considered to be non-normally distributed. The non-parametric Mann–Whitney U test was used to compare quantitative variables (age, weight, BMI, size of osteochondral lesion, etc.). For the categorical variables (ICRS, ligament injury, sex, dominance, Raikin, etc.), contingency tables and χ2 tests were used (and Fisher's exact statistic was used in some cases where the expected frequency obtained was less than 5).
A confidence level of 95% was established, and a p-value <.05 was considered statistically significant for all tests performed.
ResultsThe study included 42 individuals. According to the general descriptive study, the median age was 36 years (interquartile range 28.5–49), and the median BMI was 25.5 (interquartile range 23–28). The distribution by sex was 19 women (45.2%) and 23 men (54.8%). In terms of laterality, 19 patients (45.2%) had the condition in their right ankle, and 23 patients (54.8%) had it in their left ankle. Twenty-eight patients (66.7%) reported previous recurrent sprains, compared to 14 patients (33.3%) who did not. Twenty-one patients (50%) had a positive anterior drawer test on physical examination, and 14 patients (33.3%) had a positive inversion test. When we looked at feeling of failure, 25 patients (59.5%) reported having it, compared to 17 (40.5%) who did not; a feeling of locking was reported by 9 patients (21.4%) compared to 33 (78.6%) patients who did not.
Using the Hepple classification system to analyse the MRI, we found that 5 patients (11.9%) had grade II, 16 patients (38.1%) had grade III, 20 patients (47.6%) had grade IV, and one patient (2.4%) grade V, with a mean size of .98cm2 (median: .90cm2).
Regarding Raikin's topographical classification, it is noteworthy the highest proportion of lesions (28.6%) were in quadrant 4, followed by quadrant 6 (21.4%), and lesions shared between quadrants 4 and 7 (16.7%). The remaining quadrants have lower percentages, 9.5% for quadrants 3 and 7, 4.8% for quadrant 9, 7.1% for lesions between quadrants 3 and 6, and only 2.4% for lesions located between quadrants 1 and 4 (Fig. 1).
During arthroscopy, a total of 28 patients were assessed as having an ATFL. Two patients had a calcaneofibular ligament injury. No other associated injuries were observed.
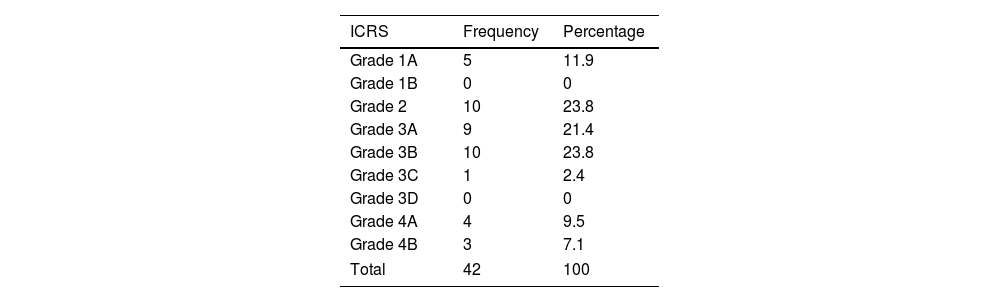
The assessment of the depth of the osteochondral lesion according to the ICRS classification system showed that 5 patients (11.9%) had grade 1A, 10 (23.8%) had grade 2, 9 (21.4%) had grade 3A, and another 10 (23.8%) had grade 3B. The least frequent grades were grade 3C in one patient (2.4%), grade 4A in 4 (9.5%), and grade 4B in 3 (7.1%). This highlights that grades 2 and 3B were the most prevalent, and grade 3C the most exceptional (Table 1).
Descriptive statistics of the frequency and percentage of the sample according to the depth of the osteochondral lesion, based on the ICRS classification system.
| ICRS | Frequency | Percentage |
|---|---|---|
| Grade 1A | 5 | 11.9 |
| Grade 1B | 0 | 0 |
| Grade 2 | 10 | 23.8 |
| Grade 3A | 9 | 21.4 |
| Grade 3B | 10 | 23.8 |
| Grade 3C | 1 | 2.4 |
| Grade 3D | 0 | 0 |
| Grade 4A | 4 | 9.5 |
| Grade 4B | 3 | 7.1 |
| Total | 42 | 100 |
When analysing BMI in relation to the location of the osteochondral lesion, a higher proportion of lateral involvement was observed in overweight patients (52.9%) than in normal-weight patients (25%) (p=.13). Similarly, no significant associations were found between BMI and severity according to the ICRS, nor with ATFL involvement.
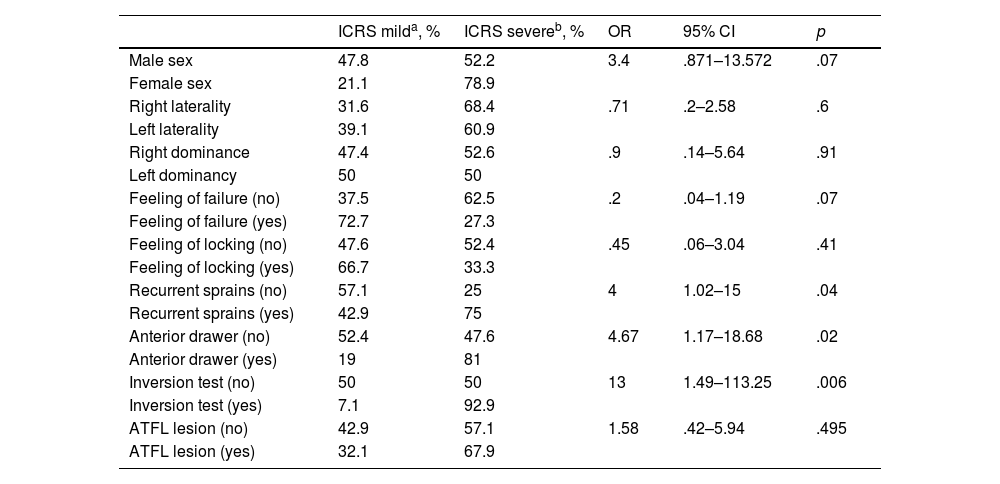
When the ICRS cartilage lesion classification was divided into mild (ICRS≤2) and severe (ICRS≥3) categories and their possible association with multiple variables was assessed, a greater tendency towards severe osteochondral lesions was observed in women (78.9%) than in men (52.2%) (p=.07). No significant differences were found when analysing the association between the degree of the lesion and variables such as laterality, dominance, topographical location, feeling of failure or locking. However, recurrent sprains (OR: 4; 95% CI: 1.02–15; p=.04), a positive anterior drawer test (OR: 4.6; 95% CI: 1.17–18.68; p=.02), and a positive inversion test (OR: 13; 95% CI: 1.49–113.25; p=.006) showed statistically significant associations with more severe lesions. This evidence suggests a strong relationship between functional or structural ankle instability and the degree of osteochondral involvement.
Although ATFL lesions were more frequent in severe cases, they did not show a statistically significant association (p=.495). No significant associations were found when each specific ICRS grade was compared with the other variables, indicating that binary grouping may offer greater discriminatory power (Table 2).
Analytical statistics of ICRS cartilage lesion and its association with the other variables.
| ICRS milda, % | ICRS severeb, % | OR | 95% CI | p | |
|---|---|---|---|---|---|
| Male sex | 47.8 | 52.2 | 3.4 | .871–13.572 | .07 |
| Female sex | 21.1 | 78.9 | |||
| Right laterality | 31.6 | 68.4 | .71 | .2–2.58 | .6 |
| Left laterality | 39.1 | 60.9 | |||
| Right dominance | 47.4 | 52.6 | .9 | .14–5.64 | .91 |
| Left dominancy | 50 | 50 | |||
| Feeling of failure (no) | 37.5 | 62.5 | .2 | .04–1.19 | .07 |
| Feeling of failure (yes) | 72.7 | 27.3 | |||
| Feeling of locking (no) | 47.6 | 52.4 | .45 | .06–3.04 | .41 |
| Feeling of locking (yes) | 66.7 | 33.3 | |||
| Recurrent sprains (no) | 57.1 | 25 | 4 | 1.02–15 | .04 |
| Recurrent sprains (yes) | 42.9 | 75 | |||
| Anterior drawer (no) | 52.4 | 47.6 | 4.67 | 1.17–18.68 | .02 |
| Anterior drawer (yes) | 19 | 81 | |||
| Inversion test (no) | 50 | 50 | 13 | 1.49–113.25 | .006 |
| Inversion test (yes) | 7.1 | 92.9 | |||
| ATFL lesion (no) | 42.9 | 57.1 | 1.58 | .42–5.94 | .495 |
| ATFL lesion (yes) | 32.1 | 67.9 |
ATFL: anterior talofibular ligament; 95% CI: 95% confidence interval; OR: odds ratio.
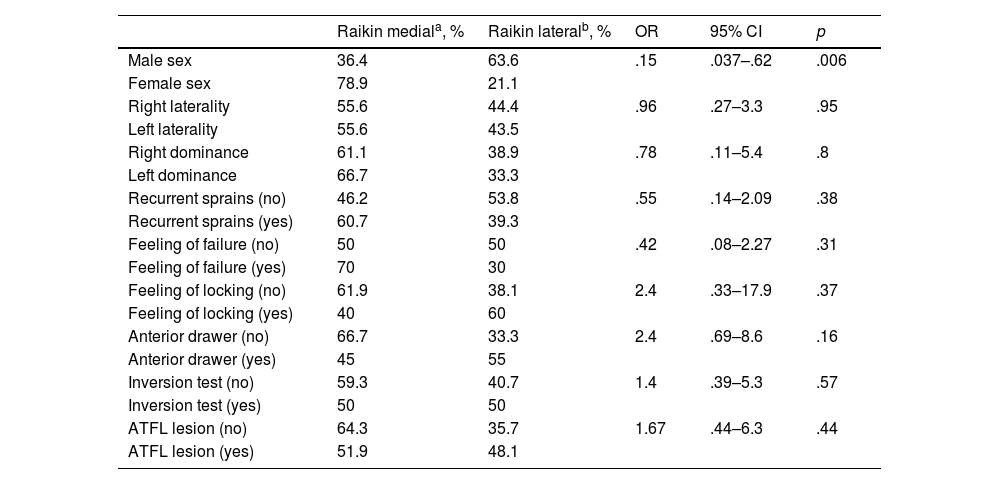
When the location of the osteochondral lesion was assessed according to Raikin's topographic classification, a statistically significant association was observed between sex and lesion location: the women had greater medial involvement (78.9%), while the men had greater lateral involvement (63.6%) (p=.006). However, no significant associations were found between the location of the lesion according to Raikin's classification and other variables, such as laterality, recurrent sprains, subjective symptoms, the results of physical examinations (e.g., anterior drawer or inversion tests), or the presence of partial or complete ATFL lesion (Table 3).
Analytical statistics of cartilage lesion according to Raikin's topographical classification system divided into lateral and medial quadrants and its association with the other variables.
| Raikin mediala, % | Raikin lateralb, % | OR | 95% CI | p | |
|---|---|---|---|---|---|
| Male sex | 36.4 | 63.6 | .15 | .037–.62 | .006 |
| Female sex | 78.9 | 21.1 | |||
| Right laterality | 55.6 | 44.4 | .96 | .27–3.3 | .95 |
| Left laterality | 55.6 | 43.5 | |||
| Right dominance | 61.1 | 38.9 | .78 | .11–5.4 | .8 |
| Left dominance | 66.7 | 33.3 | |||
| Recurrent sprains (no) | 46.2 | 53.8 | .55 | .14–2.09 | .38 |
| Recurrent sprains (yes) | 60.7 | 39.3 | |||
| Feeling of failure (no) | 50 | 50 | .42 | .08–2.27 | .31 |
| Feeling of failure (yes) | 70 | 30 | |||
| Feeling of locking (no) | 61.9 | 38.1 | 2.4 | .33–17.9 | .37 |
| Feeling of locking (yes) | 40 | 60 | |||
| Anterior drawer (no) | 66.7 | 33.3 | 2.4 | .69–8.6 | .16 |
| Anterior drawer (yes) | 45 | 55 | |||
| Inversion test (no) | 59.3 | 40.7 | 1.4 | .39–5.3 | .57 |
| Inversion test (yes) | 50 | 50 | |||
| ATFL lesion (no) | 64.3 | 35.7 | 1.67 | .44–6.3 | .44 |
| ATFL lesion (yes) | 51.9 | 48.1 |
ATFL: anterior talofibular ligament; 95% CI: 95% confidence interval; OR: odds ratio.
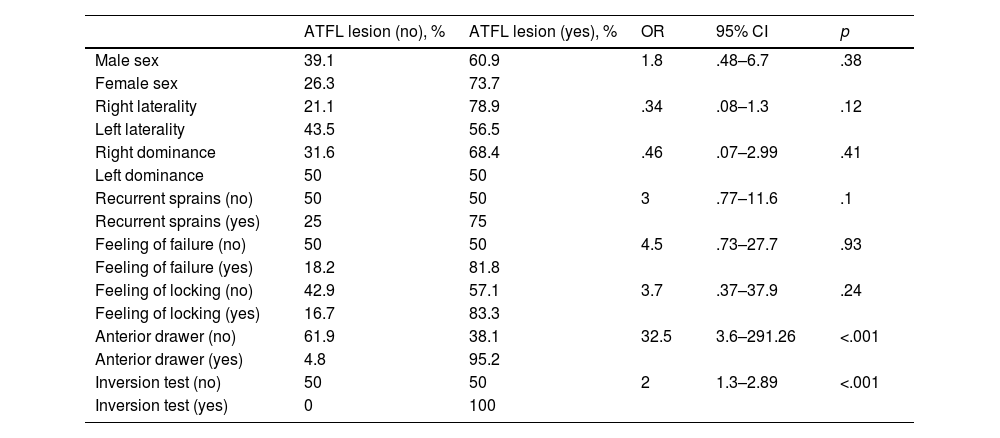
No statistically significant associations were found between ATFL lesion and variables such as sex, laterality, dominance, recurrent sprains, feelings of failure or locking. However, significant associations were observed in physical examination tests: a positive anterior drawer test was strongly associated with ATFL lesion (OR: 32.5; 95% CI: 3.6–291.26; p<.001), as was an inversion test (OR: 2.0; 95% CI: 1.3–2.89; p<.001). Previous analyses have examined associations with ICRS, Raikin, age, and BMI (Table 4).
Analytical statistics of ATFL lesion and its association with other variables.
| ATFL lesion (no), % | ATFL lesion (yes), % | OR | 95% CI | p | |
|---|---|---|---|---|---|
| Male sex | 39.1 | 60.9 | 1.8 | .48–6.7 | .38 |
| Female sex | 26.3 | 73.7 | |||
| Right laterality | 21.1 | 78.9 | .34 | .08–1.3 | .12 |
| Left laterality | 43.5 | 56.5 | |||
| Right dominance | 31.6 | 68.4 | .46 | .07–2.99 | .41 |
| Left dominance | 50 | 50 | |||
| Recurrent sprains (no) | 50 | 50 | 3 | .77–11.6 | .1 |
| Recurrent sprains (yes) | 25 | 75 | |||
| Feeling of failure (no) | 50 | 50 | 4.5 | .73–27.7 | .93 |
| Feeling of failure (yes) | 18.2 | 81.8 | |||
| Feeling of locking (no) | 42.9 | 57.1 | 3.7 | .37–37.9 | .24 |
| Feeling of locking (yes) | 16.7 | 83.3 | |||
| Anterior drawer (no) | 61.9 | 38.1 | 32.5 | 3.6–291.26 | <.001 |
| Anterior drawer (yes) | 4.8 | 95.2 | |||
| Inversion test (no) | 50 | 50 | 2 | 1.3–2.89 | <.001 |
| Inversion test (yes) | 0 | 100 |
ATFL: anterior talofibular ligament; 95% CI: 95% confidence interval; OR: odds ratio.
No statistically significant associations were found between age and the presence of ATFL lesion, the severity of osteochondral lesion according to the ICRS or medial or lateral location according to Raikin's classification. The age differences between the compared groups were minimal and not clinically relevant.
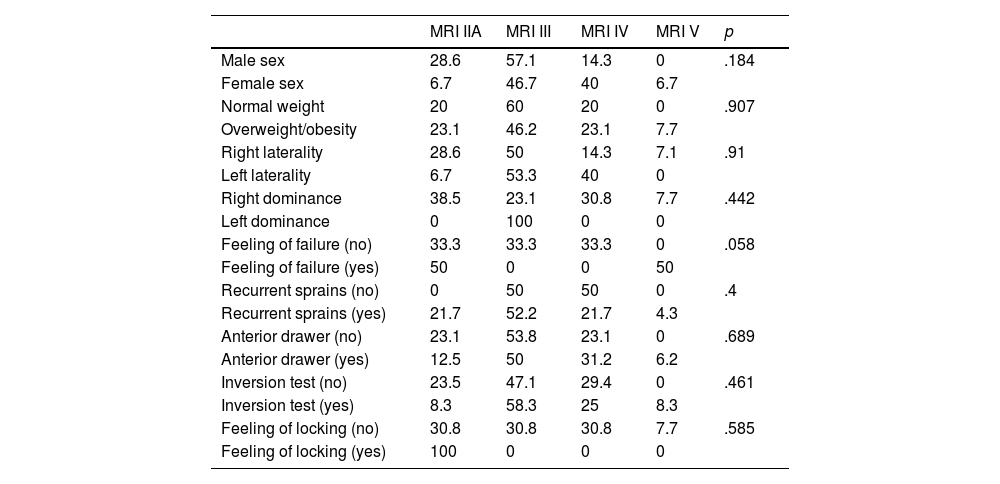
Assessment of the sample according to the Hepple classification system showed no statistically significant associations with any of the analysed variables, including the ICRS classification (p=.10) (Table 5).
Analytical statistics between the association of osteochondral lesion according to the Hepple classification system and the rest of the variables.
| MRI IIA | MRI III | MRI IV | MRI V | p | |
|---|---|---|---|---|---|
| Male sex | 28.6 | 57.1 | 14.3 | 0 | .184 |
| Female sex | 6.7 | 46.7 | 40 | 6.7 | |
| Normal weight | 20 | 60 | 20 | 0 | .907 |
| Overweight/obesity | 23.1 | 46.2 | 23.1 | 7.7 | |
| Right laterality | 28.6 | 50 | 14.3 | 7.1 | .91 |
| Left laterality | 6.7 | 53.3 | 40 | 0 | |
| Right dominance | 38.5 | 23.1 | 30.8 | 7.7 | .442 |
| Left dominance | 0 | 100 | 0 | 0 | |
| Feeling of failure (no) | 33.3 | 33.3 | 33.3 | 0 | .058 |
| Feeling of failure (yes) | 50 | 0 | 0 | 50 | |
| Recurrent sprains (no) | 0 | 50 | 50 | 0 | .4 |
| Recurrent sprains (yes) | 21.7 | 52.2 | 21.7 | 4.3 | |
| Anterior drawer (no) | 23.1 | 53.8 | 23.1 | 0 | .689 |
| Anterior drawer (yes) | 12.5 | 50 | 31.2 | 6.2 | |
| Inversion test (no) | 23.5 | 47.1 | 29.4 | 0 | .461 |
| Inversion test (yes) | 8.3 | 58.3 | 25 | 8.3 | |
| Feeling of locking (no) | 30.8 | 30.8 | 30.8 | 7.7 | .585 |
| Feeling of locking (yes) | 100 | 0 | 0 | 0 |
MRI: magnetic resonance imaging.
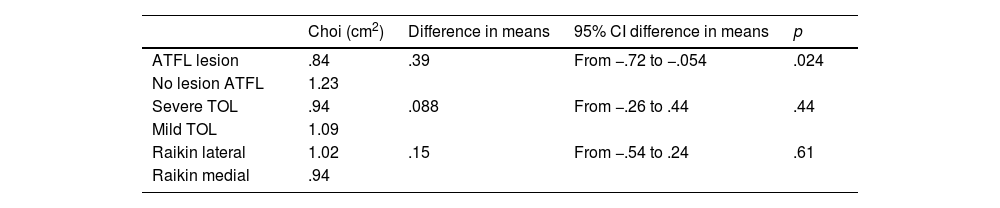
The extent of the osteochondral lesion showed no significant association with Raikin's or the ICRS classifications. However, patients without ATFL lesion had a larger lesion area (1.23cm2 vs. .84cm2), and this difference was statistically significant (p=.024). This indicates greater cartilage involvement in the absence of ligament damage (Table 6).
Analytical statistics. The association between the extent of osteochondral lesion and the other variables is described.
| Choi (cm2) | Difference in means | 95% CI difference in means | p | |
|---|---|---|---|---|
| ATFL lesion | .84 | .39 | From −.72 to −.054 | .024 |
| No lesion ATFL | 1.23 | |||
| Severe TOL | .94 | .088 | From −.26 to .44 | .44 |
| Mild TOL | 1.09 | |||
| Raikin lateral | 1.02 | .15 | From −.54 to .24 | .61 |
| Raikin medial | .94 |
ATFL: anterior talofibular ligament; 95% CI: 95% confidence interval; TOL: talar osteochondral lesions.
The main objective of our study was to confirm the potential link between chronic lateral ankle instability (CLAI) and talar osteochondral lesions (TOL). Previous studies have shown that persistent instability, particularly in patients with chronic lesions, is associated with a higher prevalence of osteochondral damage. Taga et al.6 reported an increase in TOL from 29% in acute lesions to 95% in chronic lesions, and DiGiovanni et al.7 and Hintermann et al.8 also provided supporting evidence for this association. In line with this, Komenda and Ferkel,9 and Ogilvie-Harris et al.10 described arthroscopic findings associated with chronic instability and persistent pain following ankle sprains, thereby strengthening the hypothesis that these lesions frequently occur alongside osteochondral damage. Together with clinical and diagnostic experience using arthroscopy, these findings support the hypothesis that poorly managed or recurrent CLAI promotes the development of osteochondral lesions.
As a secondary objective, we evaluated whether the association between CLAI and TOL varies according to the location of the lesion on the talar surface. Using Raikin's model, we identified a predominant pattern in medial quadrants (approximately 57.2% in our sample), similar to that described in previous studies (Raikin et al.,11 Verhagen et al.12). This finding suggests that forced inversion mechanics could favour the development of TOL in this particular area by generating greater axial load in the medial area, although methodological variability between studies prevents definitive conclusions from being drawn.
Another secondary objective was to determine whether the degree of involvement, as classified according to the ICRS, correlates with the presence of instability. Our analysis differentiated between mild and severe lesions, and found a tendency towards greater severity in some subgroups (e.g., a higher percentage of lesions ICRS lesions ≥grade 3A in patients with positive anterior drawer and inversion test results, with p≤.04). However, other comparisons, such as the association between ATFL and TOL severity, did not reach statistical significance (OR: 1.58; 95% CI: .42–5.94; p=.495). This highlights the need for larger and more ambitious studies that allow for a more statistically powerful evaluation in order to detect less apparent associations.
Apart from the main association between CLAI and TOL, the study presents other findings that are relevant to our understanding of the pathogenesis and characteristics of osteochondral lesions of the talus. For example, there is a statistically significant association between female sex and a higher frequency of medial lesions in the talus (p≤.006). It is hypothesised that greater ligamentous hyperlaxity in women, influenced by hormonal factors (especially the oestrogen cycle, which affects collagen synthesis and organisation), could predispose them to a higher risk of ligament complex damage, as reported in anterior cruciate ligament injury studies by Hewett et al., Renström et al., and Sutton and Bullock.13–15
However, although it was expected that the severity of the lesion, as assessed arthroscopically using the ICRS classification system, would correlate directly with structural damage evidenced on MRI (Hepple classification), the study found no significant correlation (p=.10). This has previously been observed in studies showing that the correlation between the Hepple classification system and histological or arthroscopic reality may be limited.16
Paradoxically, patients with ATFL involvement had less extensive osteochondral lesions than those with intact ATFL (OR: 1.58; 95% CI: .42–5.94; p=.495). It has been suggested that the redistribution of biomechanical load in the presence of chronic ATFL rupture could produce repetitive microtrauma, resulting in less concentrated lesions. This is in contrast to single traumatic episodes involving greater energy.
Finally, we compared other epidemiological variables, such as the topographical location of the osteochondral lesion, age, BMI, and the results of instability tests reported in studies by Raikin et al., Verhagen et al., and Kim et al.,11,12,17 which confirmed similar data to that in our sample.
ConclusionThis analysis confirms the significant association between chronic lateral ankle instability and osteochondral lesions of the talus. According to the ICRS classification system, patients with clinical signs of instability, such as recurrent sprains and positive anterior drawer and inversion tests, have greater chondral involvement. However, those without ATFL involvement show greater lesion extension. This suggests that osteochondral damage may depend not only on ligament instability, but also on complex lesion mechanisms that are not yet fully understood.
According to Raikin's classification, a higher frequency of medial lesions was observed in terms of topographical distribution, especially in the women. This could be related to hormonal factors or ligamentous hyperlaxity. However, the location and ligamentous involvement did not significantly correlate with the severity of the chondral lesion on arthroscopy. Similarly, the lack of concordance between the Hepple classification system on MRI and arthroscopic evaluation highlights the diagnostic limitations of MRI imaging in accurately assessing the severity of osteochondral damage. This emphasises the clinical value of functional tests in diagnosing CLAI.
In summary, the relationship between CLAI and TOL is a complex, multifactorial clinical challenge that is not yet fully understood. The low frequency with which both conditions coexist and are diagnosed together, combined with variability in their clinical and biomechanical expression, as well as in imaging tests, makes diagnosis even more challenging.
Level of evidenceLevel II evidence.
Right to privacy and informed consentThe authors obtained informed consent from all patients and/or subjects referred to in the article. This document is held by the corresponding author.
Protection of individualsThe authors declare that no experiments involving humans or animals were conducted for this research study.
Data confidentialityThe authors declare that they have adhered to their workplace's protocols for publishing patient data, and that all patients included in the study were provided with sufficient information and gave their informed written consent to participate.
Ethics committeeThis study complies with essential ethical standards and deontological criteria, meeting the necessary methodological requirements and internal operating standards of the Research Ethics Committee of Hospital 12 de Octubre.
FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to express our sincere gratitude to Dr Vilá y Rico for his invaluable help with this work. His knowledge, dedication and support have been fundamental to its completion.