The objective of our study was to evaluate whether static or dynamic fixation mode in non-comminuted femoral shaft fractures treated with intramedullary nail (IMN) exhibits differences in terms of nonunion. We hypothesize that there is no difference between both groups.
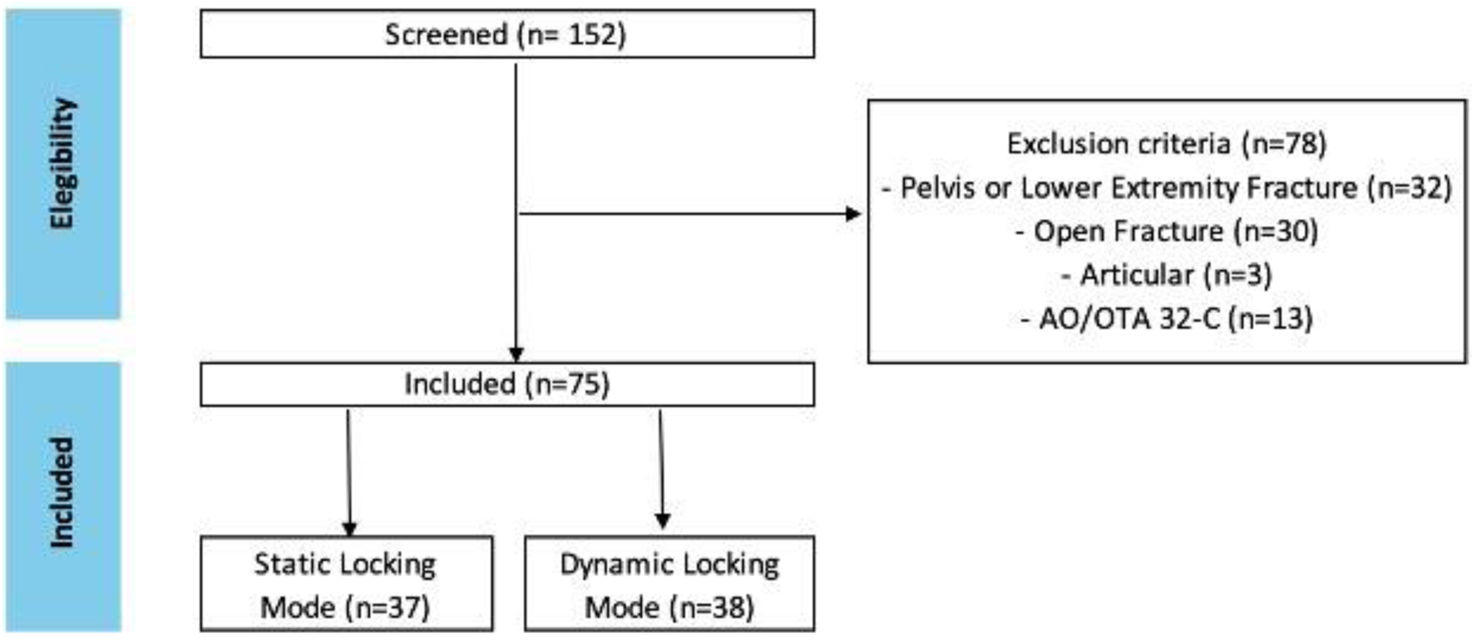
MethodsDesign: Retrospective. Setting: Level 1 trauma center. Patient selection criteria: Patients treated for femoral shaft fractures with IMN. Exclusion criteria included age under 18 years old, polytrauma patients, open fractures, periprosthetic fractures, pathologic fractures, associated lower extremity fractures, fractures involving joint extension, bilateral femoral fractures, or comminuted fractures. Outcome measures and comparisons: The primary outcome was the nonunion rate, defined as either a lack of progression in the radiographic femoral RUST score between two consecutive intervals starting at 6 months or a RUST score of less than 9 points at 12 months. The secondary outcome consists of nonunion rate analysis between groups based on AO/OTA classification subgroups.
ResultsIn total 75 patients with the same number of fractures were included with a mean age of 33.5 years (SD 13.11). Thirty-seven (49.3%) patients received statically locked fixation and 38 (50.7%) patients received dynamically locked fixation. The overall nonunion rate was 9.3%, with no significant differences between groups (p=0.219). Union rates across the AO/OTA classification groups showed statistically significant differences (p=0.036). However, no differences were observed for the AO/OTA-A (p=0.423) and AO/OTA-B (p=0.221) groups when subgroup analysis by locking mode was performed. Good interobserver (ICC=0.832; 95% CI=0.66–0.92) and intraobserver (ICC=0.881; 95% CI=0.79–0.93) reliability of femoral RUST score was found.
ConclusionNo significant differences were found in overall nonunion rates between static and dynamic locking IMN fixation in non-comminuted femoral shaft fractures. Similarly, no differences were observed in fixation type when analyzing the AO/OTA-A or -B subgroups separately.
El objetivo de nuestro estudio fue evaluar si el modo de fijación estática o dinámica en fracturas no conminutas del diáfisis femoral tratadas con clavo endomedular (CEM) exhibe diferencias en términos de seudoartrosis. Nuestra hipótesis es que no hay diferencias entre ambos grupos.
MétodosDiseño: Retrospectivo. Entorno: Centro de traumatología de Nivel 1. Criterios de selección de pacientes: Pacientes tratados por fracturas del eje femoral con CEM. Los criterios de exclusión incluyeron edad inferior a 18 años, pacientes politraumatizados, fracturas abiertas, fracturas periprotésicas, fracturas patológicas, fracturas asociadas de extremidades inferiores, fracturas que involucran extension articular, fracturas femorales bilaterales o fracturas conminutas. Medidas de resultado y comparaciones: El resultado primario fue la tasa de no unión, definida como la falta de progresión en la puntuación RUST femoral radiográfica entre dos intervalos consecutivos a partir de los 6 meses o una puntuación RUST inferior a 9 puntos a los 12 meses. El resultado secundario consistió en el análisis de la tasa de seudoartrosis entre grupos basado en los subgrupos de clasificación AO/OTA.
ResultadosEn total, se incluyeron 75 pacientes con el mismo número de fracturas, con una edad media de 33,5 años (DE 13,11). 37 (49,3%) pacientes recibieron fijación con bloqueo estático y 38 (50,7%) pacientes recibieron fijación con bloqueo dinámico. La tasa global de no unión fue del 9,3%, sin diferencias significativas entre los grupos (p=0,219). Las tasas de consolidación entre los grupos de clasificación AO/OTA mostraron diferencias estadísticamente significativas (p=0,036). Sin embargo, no se observaron diferencias para los grupos AO/OTA-A (p=0,423) y AO/OTA-B (p=0,221) cuando se realizó el análisis de subgrupos por tipo de bloqueo. Se encontró una buena fiabilidad interobservador (ICC=0,832; IC 95%=0,66-0,92) e intraobservador (ICC=0,881; IC 95%=0,79-0,93) de la puntuación RUST femoral.
ConclusiónNo se encontraron diferencias significativas en las tasas globales de no unión entre la fijación con clavo endomedular con bloqueo estático y dinámico en fracturas no conminutas del eje femoral. De manera similar, no se observaron diferencias en el tipo de fijación al analizar los subgrupos AO/OTA-A o B por separado.
Intramedullary nailing (IMN) fixation is considered the gold standard for osteosynthesis of femoral shaft fractures. Despite advancements in implant design, significant nonunion rates are reported in the literature, remaining an important issue for trauma surgeons with a high financial impact.1,2
Modern intramedullary nails allow two locking fixation modes, static or dynamic. Dynamic fixation aims to promote contact between bone fragments and has been widely proposed as a treatment for nonunion. Although some authors have reported favorable outcomes with its use, there is a lack of studies in the literature comparing the fixation mode in terms of union in primary femoral fixation.3,4
The objective of our study was to evaluate whether static or dynamic fixation mode in non-comminuted femoral shaft fractures treated with IMN exhibit differences in terms of nonunion. We hypothesize that there are no differences in bone healing rate between both groups.
Material and methodsStudy designThis study was an institutional review board-approved retrospective review of a consecutive series of patients admitted with femoral shaft fracture (AO/OTA 32) under workers’ compensation insurance treated with intramedullary nailing at a level I trauma center between 2014 and 2021. Exclusion criteria included age under 18 years old, polytrauma patients, open fractures, periprosthetic fractures, pathologic fractures, associated lower extremity fractures, fractures involving joint extension, bilateral femoral fractures, or comminuted fractures (AO/OTA 32-C).
Grouping and baseline variablesPatients were grouped based on the locking mode of the interlocking screw, being either dynamic or static. Dynamically locked IMNs were defined as having ≥2mm available for the collapse in the elongated screw slot in the immediate post-operative X-ray. Those having less than 1mm of available collapse or with a second static adjacent screw were considered to be statically locked.5
Clinical data were collected from electronic medical records, including patient demographics, locking mode, the time interval between injury and definitive surgery, use of external fixator, nail diameter, need for open reduction, and chosen surgical technique (anterograde or retrograde IMN). All patients participated in the same rehabilitation program regardless of the surgical technique, consisting of partial to full weight bearing with crutches and physiotherapy starting the day after surgery.
Radiographic evaluationPostoperative radiographs were collected, deidentified, and individually evaluated by two orthopaedic trauma surgeons (X.X and X.X). All patients underwent anteroposterior and lateral femur radiographs at 3, 6, 9, and 12-month intervals or until bone healing was achieved.
Bone healing was defined as a Radiographic Union Score for Tibia (RUST) score greater than or equal to 9 and nonunion was defined as either a lack of progression of the RUST score between two consecutive intervals starting at 6 months or a RUST score of less than 9 at 12 months.6
Statistical analysisContinuous variables were expressed as means±standard deviation where appropriate, while the dichotomous variables were expressed as the number and percentage of patients. The Shapiro–Wilk normality test was used to assess the normality of distributions.
The independent samples t-test was used to compare measurements between cohorts. Categorical variables were analyzed using the chi-square test. Logistic regression was used to assess the effect of age on bone healing. Reliability was tested using the intraclass correlation coefficient (ICC) via a two-way mixed model. SPSS (v25; IBM) was used to perform these statistical analyses and statistical significance was set at a p-value of less than 0.05.
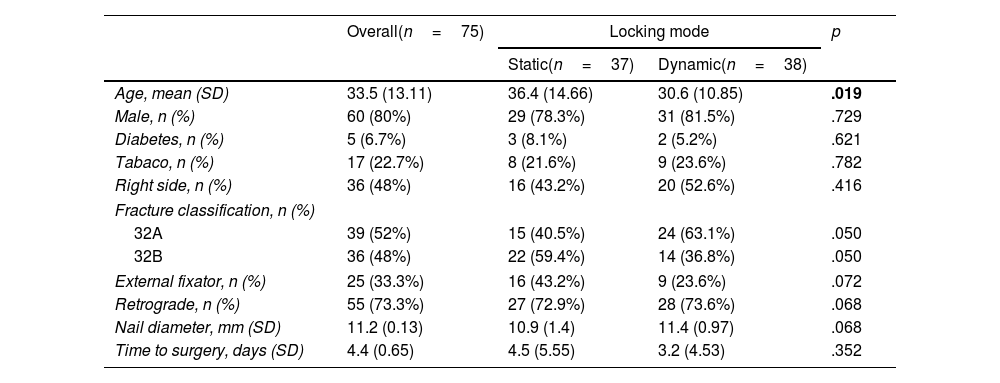
ResultsSeventy-five patients with the same number of femoral shaft fractures were included (Fig. 1). No bilateral, pathologic, or periprosthetic AO/OTA 32 fractures were observed during this study, none of them required open reduction, and all patients were over 18 years old. Demographic and radiographic characteristics are presented in Table 1.
Demographic and radiographic characteristics.
| Overall(n=75) | Locking mode | p | ||
|---|---|---|---|---|
| Static(n=37) | Dynamic(n=38) | |||
| Age, mean (SD) | 33.5 (13.11) | 36.4 (14.66) | 30.6 (10.85) | .019 |
| Male, n (%) | 60 (80%) | 29 (78.3%) | 31 (81.5%) | .729 |
| Diabetes, n (%) | 5 (6.7%) | 3 (8.1%) | 2 (5.2%) | .621 |
| Tabaco, n (%) | 17 (22.7%) | 8 (21.6%) | 9 (23.6%) | .782 |
| Right side, n (%) | 36 (48%) | 16 (43.2%) | 20 (52.6%) | .416 |
| Fracture classification, n (%) | ||||
| 32A | 39 (52%) | 15 (40.5%) | 24 (63.1%) | .050 |
| 32B | 36 (48%) | 22 (59.4%) | 14 (36.8%) | .050 |
| External fixator, n (%) | 25 (33.3%) | 16 (43.2%) | 9 (23.6%) | .072 |
| Retrograde, n (%) | 55 (73.3%) | 27 (72.9%) | 28 (73.6%) | .068 |
| Nail diameter, mm (SD) | 11.2 (0.13) | 10.9 (1.4) | 11.4 (0.97) | .068 |
| Time to surgery, days (SD) | 4.4 (0.65) | 4.5 (5.55) | 3.2 (4.53) | .352 |
Bold figures indicate statistical significance (p<.05).
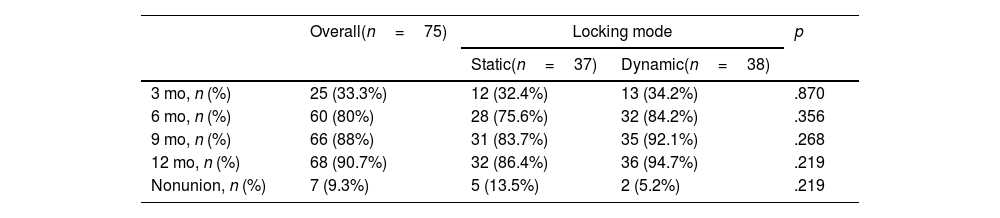
We observed an overall nonunion rate of 9.3%, with no differences between the static and dynamic groups (p=.219). See Table 2.
Time to bone healing and nonunion by locking mode.
| Overall(n=75) | Locking mode | p | ||
|---|---|---|---|---|
| Static(n=37) | Dynamic(n=38) | |||
| 3 mo, n (%) | 25 (33.3%) | 12 (32.4%) | 13 (34.2%) | .870 |
| 6 mo, n (%) | 60 (80%) | 28 (75.6%) | 32 (84.2%) | .356 |
| 9 mo, n (%) | 66 (88%) | 31 (83.7%) | 35 (92.1%) | .268 |
| 12 mo, n (%) | 68 (90.7%) | 32 (86.4%) | 36 (94.7%) | .219 |
| Nonunion, n (%) | 7 (9.3%) | 5 (13.5%) | 2 (5.2%) | .219 |
mo, months. p-Value <0.05.
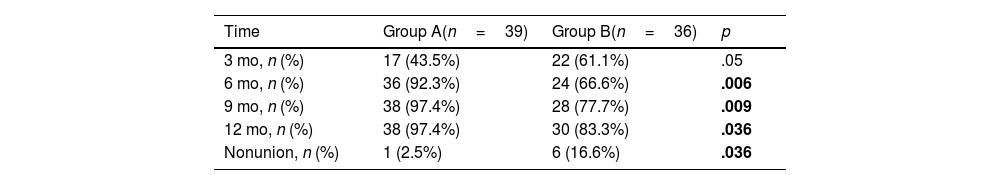
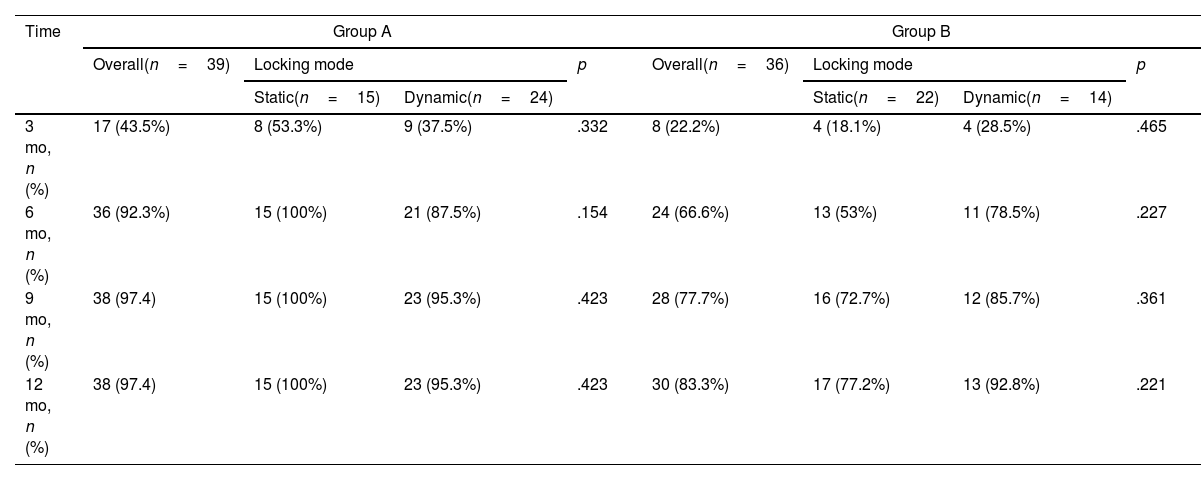
Differences in terms of age between groups were noted (p=.019). However, logistic regression did not reveal an effect of age on bone healing rate (p=.888). When comparing the groups in terms of AO/OTA classification, they were found to be approaching statistically significant differences (p=.050). Therefore, to further explore this finding, we assessed the bone healing rates among AO/OTA classification groups, finding statistically significant differences (p=0.036). However, the analysis by locking mode did not show statistically significant differences for the AO/OTA-A (p=.423) and AO/OTA-B (p=.221) groups. See Tables 3 and 4.
Time to bone healing by AO/OTA classification group.
| Time | Group A(n=39) | Group B(n=36) | p |
|---|---|---|---|
| 3 mo, n (%) | 17 (43.5%) | 22 (61.1%) | .05 |
| 6 mo, n (%) | 36 (92.3%) | 24 (66.6%) | .006 |
| 9 mo, n (%) | 38 (97.4%) | 28 (77.7%) | .009 |
| 12 mo, n (%) | 38 (97.4%) | 30 (83.3%) | .036 |
| Nonunion, n (%) | 1 (2.5%) | 6 (16.6%) | .036 |
mo, months. Bold figures indicate statistical significance (p<.05).
Time to bone healing by AO/OTA classification group and locking mode.
| Time | Group A | Group B | ||||||
|---|---|---|---|---|---|---|---|---|
| Overall(n=39) | Locking mode | p | Overall(n=36) | Locking mode | p | |||
| Static(n=15) | Dynamic(n=24) | Static(n=22) | Dynamic(n=14) | |||||
| 3 mo, n (%) | 17 (43.5%) | 8 (53.3%) | 9 (37.5%) | .332 | 8 (22.2%) | 4 (18.1%) | 4 (28.5%) | .465 |
| 6 mo, n (%) | 36 (92.3%) | 15 (100%) | 21 (87.5%) | .154 | 24 (66.6%) | 13 (53%) | 11 (78.5%) | .227 |
| 9 mo, n (%) | 38 (97.4) | 15 (100%) | 23 (95.3%) | .423 | 28 (77.7%) | 16 (72.7%) | 12 (85.7%) | .361 |
| 12 mo, n (%) | 38 (97.4) | 15 (100%) | 23 (95.3%) | .423 | 30 (83.3%) | 17 (77.2%) | 13 (92.8%) | .221 |
mo, months. p-Value <0.05.
The ICC for the interobserver and intraobserver agreement was 0.832 (95% CI, 0.66–0.92) and 0.881 (95% CI, 0.79–0.93), respectively.
DiscussionThe main finding of our study was that nonunion rates for non-comminuted femoral shaft fractures treated with static versus dynamic locking fixation mode IMNs showed no differences.
Our study along with others, demonstrated a higher percentage of nonunion in the AO/OTA-B group compared to the AO/OTA-A group.7,8 However, no differences were found in each group regarding nonunion rates when evaluated by locking mode. Despite not reaching statistically significant differences, fractures in the AO/OTA-B group fixed dynamically achieved higher union rates than those fixed statically (92.8% vs. 77.2%) suggesting a potential benefit of dynamic locking mode in this specific group. Conversely, in the AO/OTA-A group, a slightly higher consolidation rate at final follow-up was observed in the static fixation cohort (100% vs. 95.3%).
Numerous studies have evaluated the effect of secondary dynamization for the treatment of nonunion or delayed union. In one randomized study of 50 patients with femoral fractures treated with IMN in static locking mode, the effect of secondary dynamization in 26 cases showed a shorter bone healing time without differences in the nonunion rate.3 Conversely, in a non-randomized study, Tigani et al. (n=179) evaluated the effect of secondary dynamization in 75 patients and found that patients with static locking mode fixation were associated with a shorter union time (14.9 vs. 18 weeks, p=0.005).4 However, the literature lacks studies evaluating the effect of primary dynamic fixation. A recent multicenter study evaluating the effect of fixation mode in atypical femoral fractures published by Fang et al. showed that the dynamic locking mode of IMNs is associated with a faster time to union, a lower rate of nonunion, and fewer treatment failures.5
We found an overall nonunion rate of 9.3%, consistent with previous reports in the literature.9,10 While there is no clear consensus on which method most precisely represents radiographic union, a femoral RUST score of 9 points has been proposed as bone healing.6,11,12 Consistent with previous studies, we found excellent inter-observer reliability and intra-observer reliability for the femoral RUST score.13
We decided to exclude lower limb-associated injuries, bilateral fractures and fractures with joint extension to isolate the effect of limb non-weight bearing on bone healing. Similarly, we excluded factors previously described as major risk factors for nonunion, such as open femoral fractures and polytrauma patients.7 Patients with other less determinant risk factors, such as the use of external fixators, smoking, and the time between the accident and surgery, were included in our study; however, no differences were found between both groups.7
AO/OTA-C fractures were not considered in this study due to their comminution, making them unsuitable for dynamic fixation, and they were not performed at our center during this time period.14 Since our patients were treated under workers’ compensation insurance, we had no loss to follow-up of patients until their bone healing or completion of nonunion treatment.
We acknowledge some limitations in this study. Firstly, it was a retrospective study from a prospective series and is subject to the limitations and biases inherent in such studies. There were age differences between groups. To address this, we confirmed that age was not correlated with union rate. Finally, as an image-based study, we only report radiographic outcomes and do not correlate these radiographic findings to clinical results.
ConclusionNo significant differences were observed in overall nonunion rates between static and dynamic locking mode IMN fixation in non-comminuted femoral shaft fractures. While no differences were observed in the AO/OTA-A or AO/OTA-B subgroups either, the AO/OTA-B group fixed dynamically showed a higher tendency towards bone healing. These findings suggest that static and dynamic fixation modes may be equally effective for these fractures. Further studies with larger sample sizes in each fracture type group are necessary to determine if one fixation mode is superior to the other.
Level of evidenceTherapeutic level III.
Patient dataThis article contains no sensitive patient data.
Ethics committee approval codeCEC/02/2020.
FundingNone declared.
Conflicts of interestNone declared.