Patellar tendon ruptures (PTR) are rare but highly disabling injuries. Surgical treatment is the standard approach. Postoperative patellar height (PH) is used to determine the success of the intervention, with various indices described in the literature. The objective of the study was to determine if there are differences in PH according to the Insall–Salvati index in the immediate postoperative period and at 4 months, between two groups of patients operated on for acute PTR: The first group underwent isolated repair techniques (IR) and the second group had biological augmentation with autograft or allograft added to the repair (BAR). Our hypothesis was that the BAR group would have lower PH in the immediate postoperative period and at 4 months.
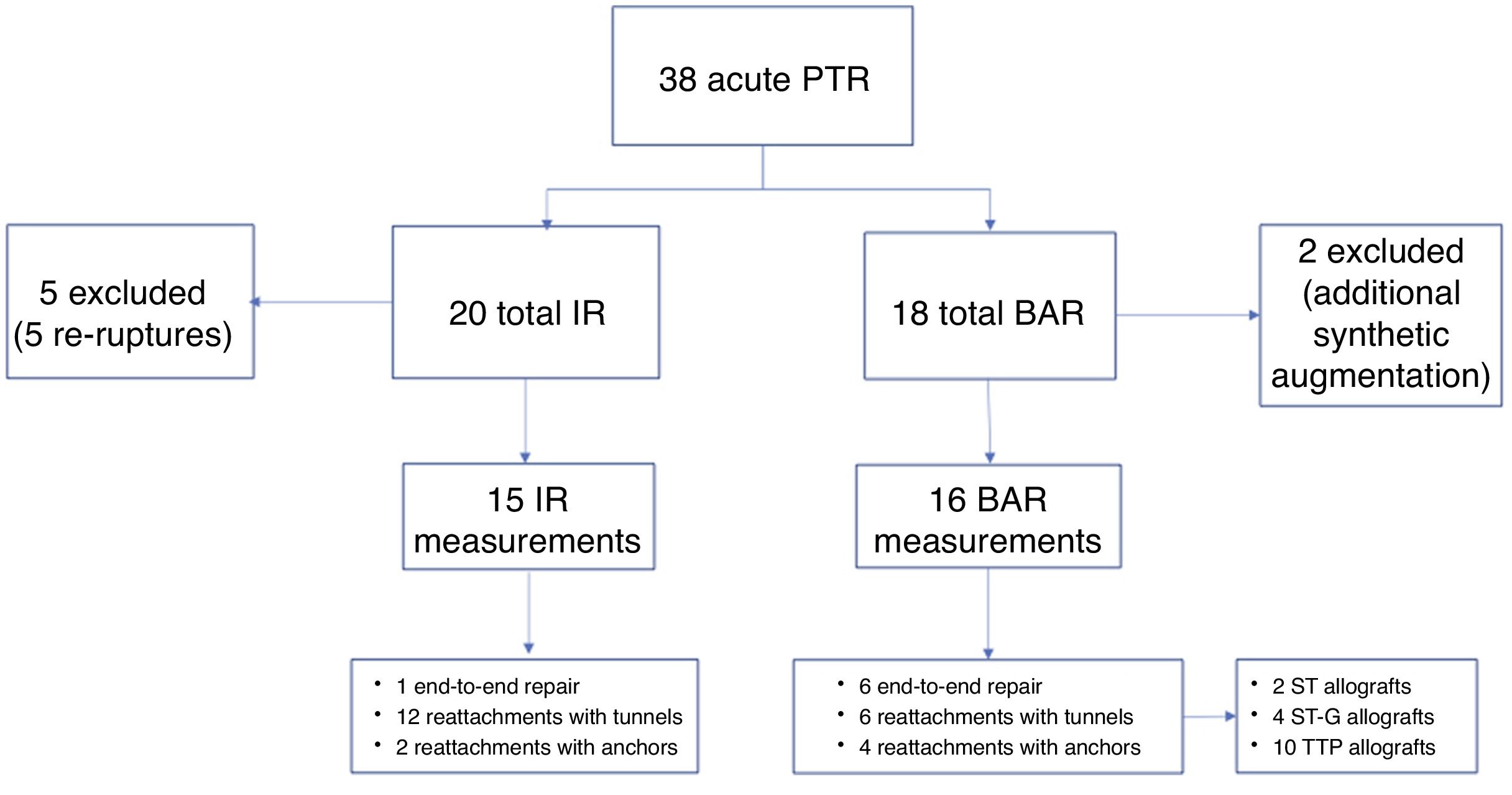
Materials and methodsAll patients with acute PTR treated at our centre between 2016 and 2022 were reviewed retrospectively. Patients with re-rupture of the operated tendon and those with non-biological augmentation were excluded. PH according to the Insall–Salvati index was measured in radiographs taken the day after surgery and at 4 months postoperatively by three orthopaedic surgeons with a subspecialty in knee surgery, independently. A fourth blind evaluator analysed the measurement results, determining the average PH and the intraclass correlation coefficient for absolute agreement among the three evaluators. The primary outcome was the difference in PH between both groups the day after surgery and at 4 months. The secondary outcome was the difference in PH between the immediate postoperative measurement and at 4 months in both groups.
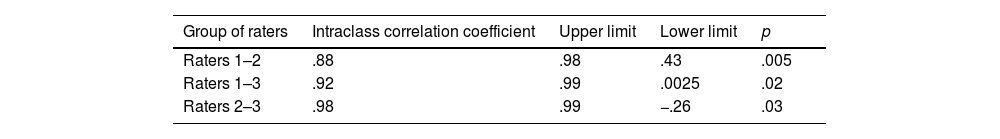
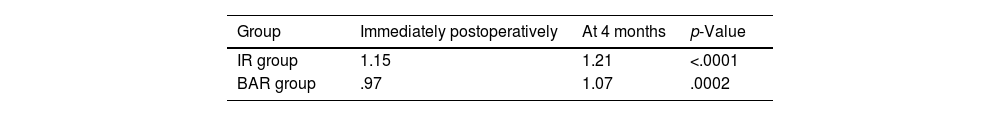
ResultsThis was a retrospective observational study. Thirty-one operated knees were included. IR was performed on 15 knees (48.38%), and biological augmentation was added in 16. The intraclass correlation coefficient between observer 1 and 2 was 0.88; between 2 and 3 it was 0.89; and between observers 1 and 3 it was 0.92, showing at least substantial agreement among observers. The average Insall–Salvati index the day after surgery and at 4 months was 1.15 and 1.21 for the IR group, and 0.97 and 1.07 for the BAR group, respectively. A statistically significant difference in the Insall–Salvati index was found between the two groups, both in the measurement taken the day after surgery (p<0.0001) and at 4 months (p=0.0002). Additionally, significant differences were observed indicating an increase in average PH when comparing the immediate postoperative measurement and at 4 months in each study group (for IR p=0.0016 and for BAR p<0.0001).
ConclusionsThe Insall–Salvati index was significantly lower in BAR cases both the day after surgery and at 4 months postoperatively. Additionally, a significant increase in PH was observed at 4 months, regardless of the surgical technique used. Substantial inter-observer agreement was achieved for PH measurement in this cohort.
Las roturas del tendón rotuliano (RTR) son lesiones infrecuentes pero altamente incapacitantes. El tratamiento quirúrgico es el estándar. La altura patelar (AP) postoperatoria es utilizada para determinar el éxito de la intervención, para lo que existen varios índices descritos en la literatura. El objetivo del estudio fue determinar si existen diferencias en la AP según el índice Insall-Salvati en el postoperatorio inmediato y a los 4 meses entre 2 grupos de pacientes operados de RTR aguda: el primero, resuelto con técnicas de reparación aislada (RATR) y, el segundo, en el que se agregó aumento biológico con auto- o aloinjerto a la reparación (ABTR). Nuestra hipótesis fue que el grupo ABTR tuvo una menor AP en el postoperatorio inmediato y a los 4 meses.
Materiales y métodosTodos los pacientes con RTR aguda intervenidos en nuestro centro entre 2016 y 2022 fueron revisados retrospectivamente. Se excluyeron pacientes con rerotura del tendón operado y con aumentación no biológica. La AP según el índice de Insall-Salvati fue medida en las radiografías tomadas al día siguiente de la cirugía y a los 4 meses de evolución por 3 ortopedistas con subespecialidad en cirugía de rodilla, de forma independiente. Un cuarto evaluador, ciego, analizó los resultados de las mediciones, determinando el promedio de AP y el índice de correlación intraclase de acuerdo absoluto para la media entre los 3 evaluadores. El resultado primario fue la diferencia de AP entre ambos grupos al día siguiente de la cirugía y a los 4 meses. El secundario fue la diferencia de AP entre la medición postoperatoria inmediata y a los 4 meses en ambos grupos.
ResultadosEstudio retrospectivo observacional. Se incluyeron 31 rodillas operadas. Se realizó RATR en 15 rodillas (48,38%) y en 16 se agregó aumento biológico. El índice de correlación intraclase entre el observador 1 y el 2 fue de 0,88; entre el 2 y el 3 fue de 0,89 y entre los observadores 1 y 3 fue de 0,92, con una correlación al menos sustancial entre observadores. El índice Insall-Salvati promedio al día siguiente y a los 4 meses de la cirugía fue de 1,15 y 1,21 para el grupo de RATR y de 0,97 y 1,07 en el grupo de ABTR, respectivamente. Se encontró una diferencia estadísticamente significativa en el índice Insall-Salvati entre ambos grupos, tanto en la medición al día siguiente (p<0,0001) como en aquella realizada a los 4 meses (p=0,0002). Además, se observaron diferencias significativas que evidenciaron un aumento de la AP promedio al comparar la medición realizada en el postoperatorio inmediato y los 4 meses en cada grupo de estudio (para RATR p=0,0016 y para ABTR p<0,0001).
ConclusionesEl índice Insall-Salvati fue significativamente menor en los casos de ABTR tanto al día siguiente como a los 4 meses después de la cirugía. Además, observamos un aumento significativo en la AP a los 4 meses de evolución, independiente de la técnica quirúrgica utilizada. Se obtuvo una concordancia interobservador al menos sustancial para la medición de la AP de esta cohorte.
Patellar tendon ruptures (PTR) are rare injuries but highly incapacitating due to the loss of active knee extension.1 The estimated incidence of this type of injury is .68/100,000 per year,2 with a marked predominance in men, 6 times more frequent than in women.3 Ruptures at the inferior pole of the patella are the most common type of PTR, followed by ruptures within the substance and, finally, at the distal insertion of the patellar tendon in the tibial tubercle.2,4
The most common mechanism of rupture is usually secondary to a sudden eccentric contraction of the quadriceps muscle with the knee in a flexed position, usually in a tendon previously damaged due to repetitive microtrauma, systemic comorbidities, or local corticosteroid injections.2,3,5,6
Surgical treatment has been defined as the gold standard for this type of injury, with the aim of restoring knee extension and obtaining good clinical and functional results.1 In 1999, Marder and Timmerman described excellent results using the classic PTR repair, which consists of repairing the ruptured tendon using Krackow columns that are anchored by three parallel transosseous vertical tunnels in the patella.7 Other authors have recommended isolated repair of the patellar tendon (IR) using anchors due to better biomechanical or clinical results.8,9 However, several researchers have proposed new augmentation techniques to increase the failure load and decrease the formation of gaps, with the aim of optimising clinical results and allowing more intensive rehabilitation protocols.4,5,10,11 These augmentation techniques can be divided into non-biological (cerclage wires, non-absorbable sutures, suture tapes, or synthetic ligaments, among others) and biological (autografts and allografts11–13). Biomechanical studies have indicated less gap formation with the use of augmentation compared to isolated repair.2,4,10 Some recommendations have been proposed, such as those listed by Gilmore et al. in their systematic review of the literature, advising acute tendon repair and augmentation to achieve better postoperative results and the use of autografts in poor quality and scarred tendons.1 On the other hand, the available literature on radiological results, in particular on postoperative patellar height (PH) in patients undergoing repair or augmentation after a PTR, is limited to synthetic or biological augmentation techniques in chronic patellar tendon ruptures.14,15 However, to date there is little evidence of postoperative radiological indices, particularly of PH in cases of acute injuries to the patellar tendon, and there is no consensus on which technique to use and when to use it.
The objective of the present study is to present a series of patients with PTR treated in a single trauma centre and to compare the radiological results, in particular of PH according to the Insall–Salvati index in the immediate postoperative period and at 4 months of follow-up, between 2 groups: IR vs. biological augmentation techniques with autografts or allografts (BAR). Our hypothesis is that the biological augmentation group will present better PH indices than the isolated repair technique in acute ruptures.
MethodsA retrospective observational study was conducted on patients with acute PTR, over the age of 18, who were treated and underwent surgery in a single trauma centre. The study was conducted in accordance with the ethical standards recognised by the Declaration of Helsinki and resolution 008430 of 1993, and has been approved by the institution's ethics committee (internal code CEC/01/2024), having obtained the informed consent of all patients participating in the study. This included a retrospective review of the medical records of patients who underwent PTR between 2016 and 2022, and a measurement of PH according to the Insall–Salvati index, which was performed on lateral knee radiographs taken the day after surgery and at 4 months post-surgery, by 3 orthopaedic surgeons with a subspeciality in knee surgery independently, with a 2-week interval between the first and second measurements. The order of the radiographs was randomly changed for the second measurement of each rater.
A fourth independent, blinded rater analysed the measurement results, determining the mean PH for the first and second measurements of each rater, and the intraclass correlation coefficient of absolute agreement with a two-way random effects model for the mean between the three raters.
All strict lateral knee radiographs were performed according to institutional protocol with the patient in a supine position, with the knee at 30° flexion, centred 7° cranial to the centre of the knee, with the posterior part of the femoral condyles overlapping at a distance of 110cm and including 15cm of tibia (Fig. 1).
The primary outcome was the difference in PH between the two groups the day after surgery and at 4 months. The secondary outcome was the difference in PH between the immediate postoperative measurement and at 4 months in both groups.
The exclusion criteria included: patients under 18 years of age, patients with acute PTR associated with total knee replacement or fractures around the knee requiring osteosynthesis, those with more than 42 days from the injury to the time of surgery, neurological injuries that prevented active mobilisation of the operated limb, repairs with non-biological augmentation, follow-up of less than the defined minimum period of 9 months and patients who presented with re-rupture or failure of the IR or the BAR. We defined 9 months as a safe period to identify re-rupture and other complications. All the surgeries were performed by 5 surgeons from our unit with fellowship training in knee surgery. The number of surgeries per specialist varied from 11 procedures by the specialist who performed the most to the 5 interventions by the 2 surgeons who performed the fewest.
The definition of acute PTR varies in the literature; however, several studies have defined it temporally as cases in which surgical resolution is achieved within 6 weeks from the date of rupture with adequate tissue remnant.3,9,16 This is the definition we have adopted for the present investigation.
The type of surgery for each treatment group was chosen according to the surgeon's preference, which determined 2 groups: IR (end-to-end or reattachment to the patella using transosseous tunnels or anchors) and, in cases where poor tendon quality was observed with highly irregular edges and ends, BAR was chosen using any of the techniques described in the first group associated with biological augmentation (autograft or allograft). The decision on the type of repair was made by each surgeon based on the location of the rupture and the macroscopic quality of the tendon.
End-to-end repair was performed using Krackow sutures with high-strength #2 FiberWire® (Arthrex, Naples, FL, USA) or #2 Ultrabraid® (Smith & Nephew, Andover, MA, USA). In cases of reattachment, this was carried out using high-strength #2 FiberWire® or #2 Ultrabraid® sutures and Krackow-type stitches at the end of the tendon and 3 transosseous tunnels, or with 2 Corkscrew® 5.0 titanium anchors (Arthrex, Naples, FL, USA.).
Augmentation was performed using an autograft (semitendinosus or semitendinosus-gracilis) or an allograft (tibialis posterior tendon), passing an 8-shaped loop through the patellar transverse tunnel and into the tibial tubercle using the modified technique of Ecker et al.12 described by Sundararajan et al.13 In either augmentation alternative, the loop was knotted on itself once reattachment of the tendon was completed (Fig. 2).
Augmentation performed using an autograft (semitendinosus) by passing a figure-of-eight suture through the transverse patellar tunnel and into the anterior tibial tubercle using the technique described by Sundararajan et al.13
In terms of the postoperative management and rehabilitation protocol, patients were initially immobilised with a knee brace in full extension until the skin sutures were removed, and then a progressive passive range of motion was initiated until full passive range was achieved at 6 weeks, followed by discontinuation of the knee brace. All patients received physiotherapy supervised by a physiotherapist 2–5 times a week according to the institutional protocol for a minimum of 20 sessions. This involved immobilisation with the knee brace, isometric exercises, and partial loading of the limb with 2 walking sticks for 3 weeks. Subsequently, a gradual increase in flexion of the operated knee was allowed, with the aim of achieving 90° of flexion at 6 weeks post-surgery with weight-bearing according to patient tolerance. After 6 weeks, the full range of motion and unrestricted weight-bearing were allowed.
Repair failure as an exclusion criterion was defined as the loss of the ability of the postoperative patient to perform active knee extension, associated with a radiographic image showing an increase in PH compared to a previous postoperative radiograph, or an MRI consistent with re-rupture of the repaired tendon.
Demographic data on the patients were collected, as well as data related to the injury (laterality, location of the injury, time from injury to surgery), surgical data (surgical technique used, type of graft), and postoperative follow-up data (time from index surgery, re-rupture or failure, and PH according to the Insall–Salvati index the day after and 4 months after surgery).
All statistical analyses were performed using Stata 17 (StataCorp. 2021, College Station, TX, USA). No sample size calculation was performed due to the nature of this study. Normality was assessed using the Shapiro–Wilk test. For comparisons between continuous variables, the independent samples t-test was performed. We performed a χ2 test to compare categorical variables, and for the correlation between continuous and categorical variables, we performed Pearson's correlation test. We also calculated the odds ratios with their respective confidence intervals (CI) for the measure of association. The intra- and inter-observer correlation in the radiological measurements was determined using the intraclass correlation coefficient of absolute agreement with a two-way random effects model for the mean between the three raters.
A p-value of p<.05 (95% CI) was established to designate the level of statistical significance.
ResultsThis is a retrospective observational study.
Thirty-six patients with 38 cases of acute PTR who underwent surgery during the study period were identified (two patients had bilateral acute PTR). Five cases in the IR group were excluded due to surgical failure and two patients in the BAR group due to additional non-biological augmentation. After applying the exclusion criteria, a total of 29 patients with 31 operated knees (2 patients with acute bilateral IR) were included in this study, of which 27 were men (93.1%) (Fig. 3).
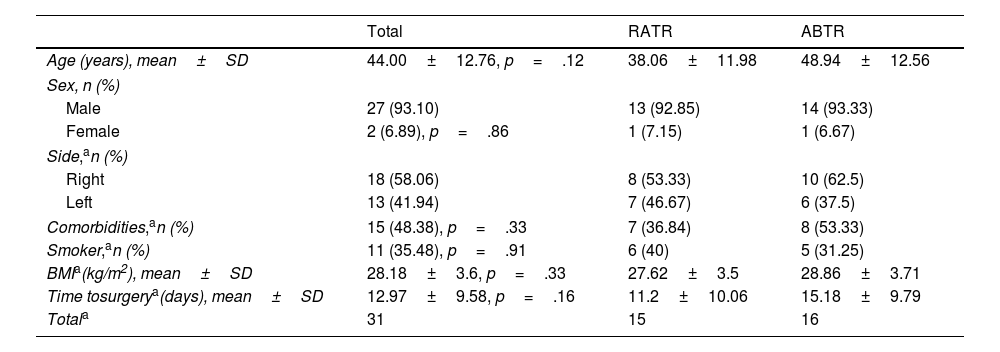
The mean age was 44.0 years (SD 12.56 years), and the mean body mass index was 28.18kg/m2 (SD 3.6kg/m2). In 18 knees (58.06%), the lesion was located on the right side. IR was performed on 15 knees (48.39%), and biological augmentation was added on 16 (51.61%) (Table 1).
Demographic characteristics.
| Total | RATR | ABTR | |
|---|---|---|---|
| Age (years), mean±SD | 44.00±12.76, p=.12 | 38.06±11.98 | 48.94±12.56 |
| Sex, n (%) | |||
| Male | 27 (93.10) | 13 (92.85) | 14 (93.33) |
| Female | 2 (6.89), p=.86 | 1 (7.15) | 1 (6.67) |
| Side,an (%) | |||
| Right | 18 (58.06) | 8 (53.33) | 10 (62.5) |
| Left | 13 (41.94) | 7 (46.67) | 6 (37.5) |
| Comorbidities,an (%) | 15 (48.38), p=.33 | 7 (36.84) | 8 (53.33) |
| Smoker,an (%) | 11 (35.48), p=.91 | 6 (40) | 5 (31.25) |
| BMIa(kg/m2), mean±SD | 28.18±3.6, p=.33 | 27.62±3.5 | 28.86±3.71 |
| Time tosurgerya(days), mean±SD | 12.97±9.58, p=.16 | 11.2±10.06 | 15.18±9.79 |
| Totala | 31 | 15 | 16 |
Age, sex, medical history, and follow-up refer to the patients. Side refers to the operated knee. p-Values for comparison between groups.
BMI: body mass index; SD: standard deviation.
There was a loss of radiographic follow-up of 6.06% (2 cases) in the first measurement and 18.18% (6 cases) in the second measurement.
The intraclass correlation coefficient between observers 1 and 2 was .88 (95% CI .43–.98; p=.005), between 2 and 3 it was .89 (95% CI −.26–.99; p=.03) and between observers 1 and 3 it was .92 (95% CI .025–.99; p=.02), finding at least a substantial correlation between the observers (Table 2).
The average Insall–Salvati index the day after and 4 months after surgery was 1.15 and 1.21 for the IR group and .97 and 1.07 in the BAR group, respectively (Table 3).
A statistically significant difference was found in the Insall–Salvati index between the two groups, both in the measurement taken the following day (p<.0001) and in the one taken after 4 months (p=.0002), with a higher PH in the IR group in both cases.
However, significant differences were also observed with an increase in the mean PH when comparing the measurement taken in the immediate postoperative period with that taken in the radiograph taken at 4 months in each study group (for IR p=.0016 and for BAR p<.0001).
DiscussionThis retrospective study reports the radiological results of patellar tendon ruptures treated surgically with isolated repair or biological augmentation. To date, and to the best of our knowledge, this is the only study that reports radiological results on the first postoperative day and at 4 months follow-up. In addition, with measurements taken by 3 blinded observers.
Compared to previous studies,9,17 we observed a slightly higher average age (44 years) in our patient cohort, but with a similar male predominance (93.1%) to that previously observed.6,9 We also found an average body mass index of 28.18, in line with previous reports.17,18 In addition, a high frequency of smokers (35.48%) was observed. Since these variables, together with comorbidities, were evenly distributed among the groups, we did not consider them confounding factors.
Surgical repair of PTR, with or without augmentation, is considered the gold standard of treatment.19,20
PH has been proposed as an objective way of measuring radiological results of patellar tendon repair, and although there is controversy over the reliability of PH indices, the Insall–Salvati index is one of the methods with the highest interobserver correlation.21 In our study, the interobserver correlation results were at least substantial, with correlations of .88 or higher. This is similar to or higher than that reported in previously published studies.21,22
The radiological results of the PTR repairs at the end of patient follow-up have been published. Marder and Timmerman,7 Bhargava et al.,23 Chen et al.,24 and Otsubo et al.25 reported PH according to Insall–Salvati at the end of follow-up, with values between .96 and 1.19. Other authors have reported similar results using the Caton-Deschamps index, such as Roudet et al.6 and Belhaj et al.16 In 2020, Core et al.15 published their results with radiological follow-up at 3 and 12 months, with a median for the Caton–Deschamps index of 1 on both dates, and reporting only 2 patients with a high patella. In our study, the mean at 0 and 4 months of follow-up was 1.15 and 1.21 for the IR group and .97 and 1.07 for the BAR group, respectively, with significant differences for both measurements between groups and between both follow-up dates. This could imply that augmentation would better maintain the tension of the repaired tendon, which could prevent its elongation in the future.
We identified several limitations in our study. The first is its retrospective, uncontrolled, and single-centre nature. Furthermore, due to the low prevalence of the injury, the sample size is small, although similar in its characteristics. Another limitation is the use of only one type of radiological index for the measurement of PH, which could lead to a bias in the interpretation of the results. Also, the follow-up period was short, without reporting functional results to correlate with the radiographic results or comparison with the contralateral knee. However, we also found strengths that we can highlight, such as the fact that both groups are comparable in size and demographic characteristics, as well as the standardisation of the surgical techniques compared and the postoperative management. In addition, our study is the first to compare the results of radiological parameters in two different surgical techniques for the management of acute PTR.
Future prospective studies are needed, with longer follow-up and in which radiological results are contrasted with functional results to determine the real relevance of our results.
ConclusionsThe Insall–Salvati index was significantly lower in cases where biological augmentation was added to patellar tendon repair. This was consistent in the measurements taken from the radiographs taken both the day after and 4 months after surgery. Additionally, we observed a significant increase in PH at 4 months, irrespective of the surgical technique used.
The interobserver agreement was at least substantial for the measurement of the PH of this cohort, which reflects an adequate reproducibility of the Insall–Salvati index.
Level of evidenceLevel of evidence iii.
Ethical approval and consent to participateThe authors of this study declare that the ethics committee of our hospital (Clinical Ethics Committee of the Hospital del Trabajador) has approved the present work, and we agree to its publication.
FundingNo specific support from public sector agencies, commercial sector, or not-for-profit organisations was received for this research study.
Conflict of interestsThe authors have no conflict of interest to declare.