Scaphotrapeziotrapezoid (STT) joint osteoarthritis may influence the outcome after trapeziometacarpal prosthesis (TMP) implantation. The literature regarding its clinical and radiological assessment is unclear. The aim of our study was to determine by means of a pre- and post-intervention CT study whether the degree of STT involvement influences the clinical–functional or radiological results after TMP implantation, and to establish whether or not STT osteoarthritis could be a contraindication for the use of these implants.
MethodsProspective study of 60 patients with trapeziometacarpal osteoarthritis grade III–IV operated between 2017 and 2022. The Van Cappelle functional test, pain, strength and mobility were evaluated. Simple radiology study and CT scan evaluating STT pre and post-surgery. The results were analysed in relation to the joint space. Recording of complications and statistics.
ResultsA total of 50 patients completed the study, mean age 59years, mean follow-up 56months, 36 Isis® and 14 Touch® were implanted. Significant improvement was observed in all variables. The STT joint space didn’t change after the intervention, and no statistical association was found between the STT joint space and the different clinical–functional variables. Three cases (6%) suffered STT pain and none required surgical revision. No infections, dislocations or loosening. Four De Quervain's tenosynovitis and two perimplant ossifications were observed. Survival of the implants was 100%.
ConclusionsThe use of TMP in patients with trapeziometacarpal osteoarthritis has excellent short and medium-term results, regardless of STT involvement, so it should not be a contraindication for osteoarthritis at this level.
La artrosis escafotrapeciotrapezoidea (ETT) puede influir en los resultados tras la implantación de una prótesis trapeciometacarpiana (PTM). La bibliografía en cuanto a su valoración clínica y radiológica es confusa. El objetivo de nuestro estudio fue determinar mediante estudio TC pre y postintervención si el grado de afectación de la ETT influye en los resultados clínico-funcionales o radiológicos, tras implantación de PTM, y establecer si la artrosis ETT podría ser contraindicación o no para el uso de estos implantes.
MétodosEstudio prospectivo sobre 60pacientes con artrosis trapeciometacarpiana gradoIII-IV intervenidos entre 2017 y 2022. Se evaluó el test funcional de Van Cappelle, dolor, fuerza y movilidad. Estudio radiológico simple y TC para evaluar la ETT pre y poscirugía. Se analizaron los resultados, relacionándolos con el espacio articular. Registro de complicaciones y estadística.
ResultadosCompletaron el estudio 50pacientes, edad media 59años, seguimiento medio 56meses. Se implantaron, 36 Isis® y 14 Touch®. Se observó mejora significativa en todas las variables. El espacio articular ETT no se modificó tras la intervención, sin encontrar ninguna asociación estadística entre el espacio articular ETT y las diferentes variables clínico-funcionales. Tres casos (6%) sufrieron dolor ETT y ninguno requirió revisión quirúrgica. No se observaron infecciones, luxaciones, aflojamientos. Cuatro tenosinovitis de De Quervain y dos osificaciones peri-implante. Supervivencia del 100% de los implantes.
ConclusionesEl uso de PTM en pacientes con artrosis trapeciometacarpiana tiene excelentes resultados a corto y a medio plazo, independientemente de la afectación ETT, por lo que no debería ser una contraindicación la artrosis a este nivel.
The presence of osteoarthritis in the scaphotrapeziotrapezoid joint (STT), in association with trapeziometacarpal osteoarthritis (TMO), known as peritrapezial osteoarthritis (PTO), presents a clinical challenge when conservative measures have failed in active, high-demand patients. Currently, trapeziometacarpal prostheses (TMP) are considered a first-line treatment option, offering faster and more satisfactory functional results than more traditional techniques1–4 and this has lead to an increase in their use. The presence of degenerative changes in the STT joint has traditionally been considered a contraindication, given its potential to cause persistent postoperative pain and unsatisfactory outcomes. However, Tchurukdichian et al.5 have recently challenged this, observing good results after TMP implantation even when the STT joint is affected.
Clinically identifying a truly painful STT joint can be difficult, but it is crucial for the decision-making process. Furthermore, simple radiographic assessment of the STT joint can often be confusing and misleading, partly due to joint overlap, and even with the aid of specific radiographic views, its involvement is frequently underestimated. This applies to any of the available radiographic classifications, such as those of Crosby and Linscheid or Eaton-Glickel (EG).
Studies such as Brown's determined that the correlation coefficients between macroscopic visual pathology and radiographic evidence of osteoarthritis in the STT are unreliable, and their results indicated that radiography underestimates the true stage of STT osteoarthritis.6–8 The EG9 classification is one of the most widely used in the diagnosis and preoperative evaluation of TMO: grade IV corresponds to complete narrowing of the TMO joint space. Hansen and Kirkeby10 suggested the use of computed tomography (CT) to avoid this underestimation of STT involvement when evaluating the TMO. This led them to propose a new sub-classification within the EG scale: grade III+, corresponding to moderate but incomplete narrowing of the STT joint, for which these same authors claim to obtain good results after the implantation of a TMP.
The objective of our study (due to the confusion and limitations in radiological classifications) was to evaluate, using CT scans of the STT joint before and after the intervention, whether the degree of STT joint involvement had any influence on the clinical, radiological, or functional outcomes obtained after TMP implantation, and to establish whether STT osteoarthritis could be a contraindication for the use of the TMP.
Material and methodWe conducted a prospective study of 60 cases of EG grade III-IV TMO treated with TMP implantation between 2017 and 2022. All cases were operated on by the four attending surgeons of our institution's unit. The study was reviewed and approved as a research project by the Clinical Research Ethics Committee of our region, meeting all necessary requirements. The 60 patients initially selected for this study were fully informed and signed the corresponding informed consent forms.
Inclusion criteria included all patients diagnosed with grade III or IV TMO according to the EG classification, in whom a primary uncemented TMP was implanted. Patients were excluded if they presented with: less than one year of clinical and radiological follow-up; concomitant hand infections; a dysplastic trapezium or a trapezium height of less than 6 mm; a physically demanding profession, or they were elderly patients with low functional demands.
Demographic data such as age, sex; laterality; hand dominance; level of physical activity, and related surgeries were recorded. The functional scale score, described by J. Van Cappelle et al.11 (visual analogue scale for pain, functionality, Kapandji mobility test, grip strength, and pinch strength, with minimum and maximum scores of 0 and 40, respectively), was assessed preoperatively and postoperatively. The grind test and radial grind test7 were also assessed preoperatively and postoperatively at 1-year intervals. The SAEHAN® SH5001 hydraulic dynamometer was used to measure grip strength, and the SH5005® was used for pinch strength. Results were scored according to hand dominance, sex, and age, based on the dynamometric studies of the hand and thumb by Torres Coscoyuela et al.12
Regarding the radiographic study, plain radiographs (anteroposterior, lateral, and Roberts views) were taken before and after the procedure annually, and the following variables were recorded: TMO grade according to the EG classification, distance from the trapezium to the head of the first metacarpal (thumb length described by J. Van Cappelle et al.11), and presence of periprosthetic radiolucency. Additionally, the angle between the orientation of the trapezium cup and the proximal articular surface of the trapezium (PAST) was measured in the lateral projection to assess the suitability of its placement.
As the primary radiographic evaluation of the STT joint, helical computed tomography (CT) scans with .6mm slices were performed before and after the procedure, at least one year after the intervention. These measurements were taken by a radiologist specialising in musculoskeletal imaging. For calculating radiographic measurements, AWServer 3.2, software for visualising medical and radiological images for diagnostic use, was used. Reference values for a normal population were used from the work of Trentadue et al.13 The trapezioscaphoid (TS) and scaphotrapezoid (ST) joint spaces were measured independently at the joint centre, and the joint centre was calculated using MPR visualisation (a DICOM viewer for multiplanar reconstruction). To minimise intraobserver error, three measurements were taken for each joint, and the mean was calculated. Implant placement was also evaluated, and the presence of complications was recorded.
The two implants used are summarised and described below:
- •
ISIS® (Evolutis, Roanne, France): Porous titanium coating, threaded, truncated conical cup, semi-constrained with slight pistoning that reduces restriction on the trapezoidal component. Metal-polyethylene bearing surface.
- •
TOUCH® (Kerimedical, Route des Acacias, Les Acacias, Switzerland): Dual-mobility prosthesis, coated with porous titanium and hydroxyapatite. The cup is available in two designs: hemispherical or conical. Metal-polyethylene bearing surface.
All patients underwent surgery under locoregional anaesthesia. A dorsal approach was used, with a 5mm resection of the base of the first metacarpal, resection of peritrapezial osteophytes, and reaming of the trapezium using motorised cannulated reamers with the aid of a guide needle placed under fluoroscopic control and centred in all planes of the trapezium and perpendicular to the PAST. Implant stability was verified by ensuring there was no impingement between the neck and the cup at maximum range of motion. Prophylactic opening of the first extensor groove was not performed. Technical data on the implanted prostheses were also collected, including stem size, cup shape, and whether the neck was straight or angled. Any other procedures performed during the surgery were also recorded.
During the postoperative period, the thumb was immobilised in a plaster splint for three weeks, after which active movement was permitted according to a pre-established exercise programme. Patient satisfaction was assessed on a scale of 0–10, as well as whether they returned to their previous activities. All observed complications were recorded (dislocation; mobilisation; infection; periprosthetic ossification; wear; tenosynovitis; neuropathy; pain at the base of the thumb), paying particular attention to the presence of pain in the STT joint and whether additional treatment was required.
Statistical analysisThe normality and homogeneity of data variances were assessed. Once these assumptions were confirmed, parametric statistical analyses were used (paired t-test to analyse differences between preoperative and postoperative measurements and unpaired t-test for comparisons between groups): Otherwise, non-parametric analyses were used (Wilcoxon signed-rank test for paired data or Mann–Whitney U test). Correlations between joint distances and age with the various functional clinical variables were determined using Spearman's rank correlation coefficient (rs). All statistical analyses were performed using SPSS for Windows (version 26.0; IBM Corp., Armonk, NY, USA). Statistical significance was defined as p<.05. The sample size was limited by the availability of CT scan.
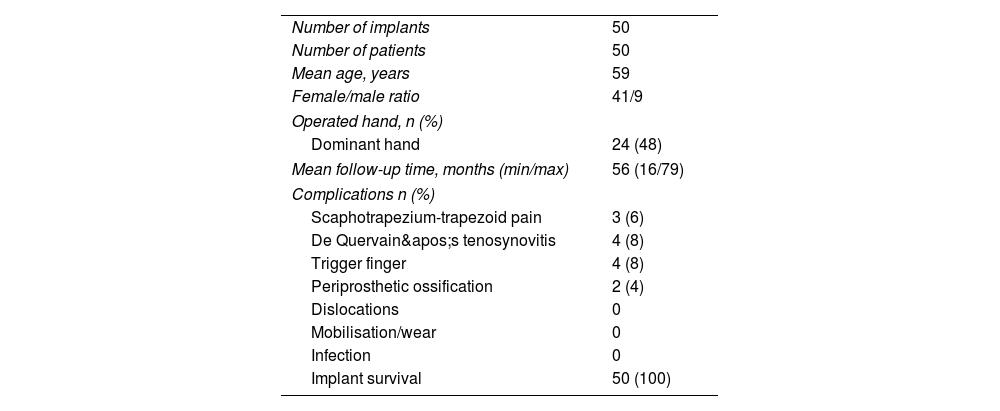
ResultsA total of 50 prostheses in 50 patients completed the study. Ten patients were lost to follow-up due to lack of clinical or radiological follow-up, two patients due to intraoperative complications after placement of a cemented cup implant, and one patient who had suffered an ipsilateral humerus fracture. The other seven patients declined follow-up as they were clinically well and had no functional limitations according to telephone interviews. Of the patients ultimately included in our study, 41 were women and 9 were men, with a mean age of 59 years (range: 50–72 years). The mean follow-up time was 56 months (range: 16–79). Surgery was performed on the dominant hand in 48% (24) of cases, and all patients had work or leisure activities that they wished to maintain. Regarding the associated surgical interventions, 9 carpal tunnel syndrome surgeries were performed, along with one excision of a giant cell tumour located on the dorsal aspect of the thumb, one distal interphalangeal arthrodesis of the second finger, and 3 trigger finger surgeries (Table 1). According to the J. Van Capelle functional scale, the mean preoperative score was 20 points (interquartile range [IQR]: 17.5–22), and postoperatively, after a minimum of one year of follow-up, the score was 37 (IQR: 34–39), representing an improvement of 17 points (p<.001). Grip strength and pinch strength improved significantly, with a median increase of 3kg preoperatively versus 5kg postoperatively (p<.001) and 14kg postoperatively versus 20kg postoperatively (p<.001). A significant improvement in pain relief was also observed, as measured by the visual analogue scale (VAS), from 7.9 (range: 7–9) preoperatively to 0.7 (range: 0–1) postoperatively (p<.001). Mobility, as measured by the Kapandji test, improved from 9 (range: 8–10) to 10 (range: 10–10) postoperatively (p<.001).
Demographic characteristics and complications.
| Number of implants | 50 |
| Number of patients | 50 |
| Mean age, years | 59 |
| Female/male ratio | 41/9 |
| Operated hand, n (%) | |
| Dominant hand | 24 (48) |
| Mean follow-up time, months (min/max) | 56 (16/79) |
| Complications n (%) | |
| Scaphotrapezium-trapezoid pain | 3 (6) |
| De Quervain's tenosynovitis | 4 (8) |
| Trigger finger | 4 (8) |
| Periprosthetic ossification | 2 (4) |
| Dislocations | 0 |
| Mobilisation/wear | 0 |
| Infection | 0 |
| Implant survival | 50 (100) |
Regarding the plain radiographic evaluation, according to the EG scale, 7 patients (14%) were classified as grade IV, and the rest as grade III.
Thumb length increased from a median of 51mm (IQR: 49–55) preoperatively to 54mm (IQR: 53–57) postoperatively (p<0.001).
A guide needle placed under fluoroscopic control was used for cup implantation in 96% of cases (48). The mean angle between the cup and the PAST on the lateral projection was 3.2° (R: 0–11). No narrowing or progressive worsening of the STT joint space was observed on radiographic evaluation, nor were there any signs of periprosthetic osteolysis.
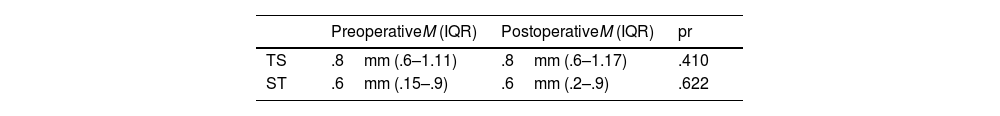
Regarding the CT scan evaluation: the median joint space in the trapezioscaphoid (TS) joint was .86mm (IQR: .6–1.11) preoperatively and .85mm (IQR: .6–1.17) postoperatively one year after the procedure. No statistically significant differences were found between the preoperative and postoperative TS joint space (p=.410).
At the scaphotrapezoid (ST) joint, the median preoperative joint space was .56mm (IQR: .15–.9) and remained at .56mm (IQR: .2–.9) postoperatively one year after surgery. No statistically significant differences were found in the ST joint space, either preoperatively or postoperatively (p=.622) (Table 2).
Difference between trapezioscaphoid (TS) and scaphotrapezoid (ST) joint spaces pre- and post-surgery, expressed as median (M) and interquartile range (IQR), measured by CT in millimetres (mm).
| PreoperativeM (IQR) | PostoperativeM (IQR) | pr | |
|---|---|---|---|
| TS | .8mm (.6–1.11) | .8mm (.6–1.17) | .410 |
| ST | .6mm (.15–.9) | .6mm (.2–.9) | .622 |
A significant difference (p<.001) was found in the TS joint space between grade III cases on the EG scale (mean: .94, SD: .32) and grade IV cases (mean: .43, SD: .26). The ST joint space was also statistically significantly smaller (p=.009) between grade III (median: .80; IQR: .30–.90) and grade IV (median: .00; IQR: .00–.35).
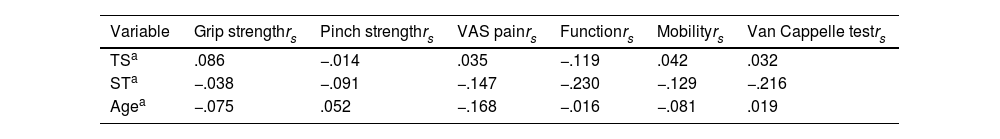
No statistically significant relationship was found postoperatively between TS and ST joint spaces, EG scale score, age; hand dominance, and the different functional clinical variables (grip strength, pinch strength, VAS pain, functionality, mobility according to the Kapandji test, and overall Van Cappelle test score) (Table 3). No cup or stem mobilization was observed.
No statistically significant association was found in the postoperative period between joint spaces (TS and ST), the grade on the EG scale, age, dominance and the different functional clinical variables (grip and pinch strength, pain, functionality, mobility according to the Kapandji test and overall result of the Van Cappelle test).
| Variable | Grip strengthrs | Pinch strengthrs | VAS painrs | Functionrs | Mobilityrs | Van Cappelle testrs |
|---|---|---|---|---|---|---|
| TSa | .086 | −.014 | .035 | −.119 | .042 | .032 |
| STa | −.038 | −.091 | −.147 | −.230 | −.129 | −.216 |
| Agea | −.075 | .052 | −.168 | −.016 | −.081 | .019 |
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | |
|---|---|---|---|---|---|---|
| EGscaleb | ||||||
| III | 20 (17–26) | 3 (2–4 | 0 (0–1) | 10 (9–10) | 10 (10–10) | 37 (34–39) |
| IV | 18 (14–24) | 3 (2–4) | 0 (0–1) | 10 (10–10) | 10 (10–10) | 38 (33–39) |
| Dominanceb | ||||||
| No | 20 (15–28) | 5 (4–6.5) | 0 (0–1) | 10 (9–10) | 10 (10–10) | 36 (33.5–39) |
| Yes | 20 (18–24) | 5 (4–6) | 0 (0–1) | 10 (10–10) | 10 (10–10) | 37 (34–40) |
EG: Eaton and Glickel; IQR: interquartile range; ST: scaphotrapezoid; TE: trapezioscaphoid.
Of the implants used, 14 were TOUCH® (28%) and 36 were ISIS® (72%). All cups had a diameter of 9mm, 50% (25) of the necks were short, and 80% (40) were straight. No statistically significant differences were found between the type of prosthesis and final function (p=.839), mobility (p=.491), grip strength (p=.674), pinch strength (p=.414), pain according to the VAS (p=.193), or the final Van Cappelle score (p=.564).
The mean patient satisfaction score was 9.3 (range: 6–10), and all patients returned to their previous activities.
Complications were few and infrequent: four cases of De Quervain's tenosynovitis were the most common, along with four cases of stenosing tenosynovitis of the long fingers. All cases resolved with conservative treatment, except for one case of De Quervain's tenosynovitis that required surgical opening of the first extensor compartment. We also encountered two cases of periprosthetic ossification, which we treated by osteophyte resection, leaving the implant in place. All patients presented with a painful preoperative grind test, which influenced the radial grind test, resulting in an inconclusive result.
After clinical examination for postoperative pain in the STT joint, 94% (47) of the patients were pain-free (Figs. 1 and 2), while 6% (3) of the patients presented with pain at this level, along with a painful radial grind test. Of these, one patient presented with eccentric placement of the cup and trapezoidal impaction. This corresponded to one of the two implants we placed without the aid of a guide needle and fluoroscopy. Of the two remaining patients, one experienced mild pain that resolved without intervention, while the other had moderate pain that required steroid injections with significant improvement (Fig. 3). No major complications such as infections, dislocations, loosening, or implant wear were recorded. Implant survival was 100% at the last follow-up.
Patients who reported STT joint pain. Images 1 and 2: Radiograph and CT scan of eccentric placement of a Touch® prosthesis. Images 3 and 4: Post-intervention CT scan of an Isis® prosthesis with mild pain at the STT joint. Images 5 and 6: Radiograph and CT scan of a patient with STT joint impingement and moderate pain.
At the time of writing this article, we have not found a clear indication in the literature regarding the tolerable degree of STT involvement, or whether, it could lead to residual symptoms after the placement of a TMP and if this represents a formal contraindication for its implantation. In recent decades, authors such as Glickel et al.14 have questioned the usefulness of trapeziectomy in patients with PTO given its limited impact on the STT joint. Glickel, in his 1992 study, concluded that moderate involvement of the STT did not affect functional outcomes over a mean follow-up of 8 years. Following ligament reconstruction and tendon interposition (LRTI), he classified these cases as grade III+: moderate degenerative changes, to distinguish it from the completely narrowed joint space present in grade IV. He concluded that complete trapeziectomy should be reserved for patients with severe STT involvement, given the aggressive nature of this procedure. He also recommended intraoperative STT arthrotomy to provide more accurate staging and facilitate the selection of the most appropriate procedure, due to the high degree of clinical–radiological incongruity found when performing plain radiographic evaluation.
Other authors15 have also emphasised the importance of maintaining the integrity of the trapezium whenever possible, even modifying existing surgical techniques to preserve it, hoping to improve thumb function by preventing metacarpal collapse and other potential complications.
More recent reviews on the treatment of PTO, such as that by Bridgforth and Ross,16 maintain that STT involvement may play a role in residual pain after arthroplasty, but offer no clarification regarding its optimal treatment. Other authors suggest that LRTI is an effective option in treating isolated STT osteoarthritis, without requiring associated partial trapezoid excision, essentially ignoring half of the problem (an affected scaphotrapezoid joint), without any apparent negative impact on outcomes.17
Other studies, such as that by Wollstein et al.18 observed that STT pain on clinical examination was not associated with the presence of osteoarthritis, supporting the suspicion of a significant clinicopathological discrepancy when evaluating this joint. Furthermore, Fouasson-Chailloux et al.19 concluded in their study that the lower pain tolerance of the TMO compared to the STT joint could not be attributed to increased innervation of the joint capsule in the former, as a higher rate of myelinated tissue was observed in the STT joint, suggesting that other nociceptive pathways may be involved. A biomechanical study performed on cadavers after TMP implantation showed no changes in pressure at the STT joint compared to preoperative measurements, suggesting that TMP implantation may not negatively affect the STT joint.20
This collection of studies raises multiple questions about the origin of STT joint pain and its behaviour. In fact, it can be suggested that trapeziectomy may not be necessary in the treatment of most cases of PTO and that, instead, these patients could benefit from the advantages offered by a TMP. The aforementioned study by Hansen and Kirkeby10 from 2016 supports this idea by implanting TMPs in patients with moderately affected STT joints. They observed good functional results but did not include patients with a grade IV or clear STT impingement.
Our study goes a step further by including all patients with a grade III or IV EG classification without exception, the main exclusion criterion being a trapezium too small for cup implantation. In our results, of the three patients who presented with localised pain over the STT joint, one was attributed to eccentric placement of the cup (Fig. 3) with impaction on the adjacent trapezoid bone, while the other two experienced resolution of their pain after conservative treatment, even though one of them presented with clear STT impingement. After a mean follow-up of almost 5 years, patient satisfaction remains very high, with no additional significant complications.
Recent reviews on the treatment of isolated STT osteoarthritis or osteoarthritis associated with TMO, such as those by Wu or Alder, or more specifically on the treatment of PTO, such as that by Bridgforth et al.,16 do not even mention TMP as a treatment option.7,21 Conversely, other authors5,22 report that TMP implantation may be sufficient to relieve pain in PTO, as in Cootjan's 5-year review of 166 Arpe® implants, of which only one patient (.6%) required salvage trapeziectomy due to persistent STT joint pain. Another review evaluated the incidence of major complications in 224 implants of various models and observed only one case (.44%) of persistent STT joint pain, which was salvaged with resection of the distal pole of the scaphoid and interposition of the palmaris longus tendon, with good results and continued implant use.23
If we examine systematic reviews on the use of TMPs and their complications, we find no specific mention of STT joint pain,24,25 except in the review by Remy et al.26 where they describe a complication rate due to STT joint pain even lower than the .23% attributed to infections. Only the review by Obert et al.27 refers to the use of TMPs in patients with PTO, even recommending their use as a way to relieve pressure on the STT joint. This same author also reports that performing ultrasound-guided sequential corticosteroid injections in the trapeziometacarpal and STT joints in patients with PTO demonstrates that in up to 90% of patients, the pain is due to the trapeziometacarpal joint and not the STT.
To our knowledge, our study is the only prospectively designed one specifically focused on the effects of TMP implantation on the STT joint, regardless of its degree of impingement. In our series, 94% of patients did not present pain at the level of the STT joint; in addition, the results obtained were satisfactory and even comparable to specific reviews of the TOUCH® or ISIS® prostheses, where patients with PTO28,29 were excluded. Direct measurement of the STT joint space, with pre- and postoperative CT scan, allows for a more accurate assessment of the behaviour of this joint and its relationship with functional results and complications, while avoiding the inherent subjectivity associated with a classification based on simple radiographic evaluation.
The recent pioneering morphometric study by Trentadue et al.13 on the healthy STT joint, performed using PCD-CT (photon-counter-detector), determined that the mean joint space of the TS was 1.39mm, and that of the ST, 1.42mm, with no significant differences between them. In our study, we report mean joint spaces of the TS and ST of .86mm and .56mm, respectively, before surgery and .85mm and .56mm, respectively, after the intervention, illustrating that the STT joint was more constricted compared to a healthy joint. Furthermore, there were no significant changes in joint space after implantation of the TMP, and this was independent of the results obtained. Complications were few, and those that occurred were resolved without the need to remove the implant. Furthermore, only one patient with pain in the STT joint presented with clear impingement (Grade IV on the EG scale), while the other two patients maintained joint space (Grade III on the EG scale). We believe, as other authors have suggested,30–32 that the few complications we observed may also be secondary to the correct placement of the implant itself, possibly thanks to the use of a guide needle and fluoroscopy, evidenced by a mean cup placement angle of 3.2° with respect to the PAST in the lateral view.
We are aware that the limitations of our study, such as the small number of cases in the series, the fact that we evaluated only two types of prosthesis (one semi-constrained with single mobility and the other with dual mobility), and the lack of a control group comparing other surgical techniques such as LRTI or STT interposition prosthesis, prevent us from making definitive statements about the expansion of the use of these implants. The inconclusive assessment of pain at the preoperative STT level may also be a confounding factor in accurately evaluating outcomes. Larger studies are therefore needed to support our results before we can make a clear statement regarding expanding the indications for total trapeziometacarpal joint replacements.
ConclusionsThe use of TMP in patients with EG grade III-IV trapeziometacarpal osteoarthritis has excellent short- and medium-term results. We believe that STT joint involvement should not contraindicate the use of implants in these patients. Further studies are required to support our findings.
Level of evidenceLevel of evidence iii.
FundingThis research did not receive specific funding from public sector agencies, commercial sector entities, or non-profit organisations.
Conflict of interestsThe authors have no conflict of interests to declare.