The FNS System DePuy Synthes® (EEUU, 2018) represents a recent alternative treatment for the fixation of femoral neck fractures, providing biomechanical advantages with respect to cannulated screws (3 CS). The objective of this study is to compare the clinical results of both fixation methods.
MethodA retrospective collection of the 36 subcapital fractures treated with the FNS system was carried out compared with a retrospective search of the last 35 patients treated with 3 CS. Age, sex, fracture pattern, delay until the intervention, length of intervention, hospital length stay, and haemoglobin loss were analysed. In addition, the rate of avascular necrosis, nonunion, symptomatic femoral neck shortening, and material protrusion with or without its removal were recorded during a minimum follow-up of 6 months.
ResultsNo significant differences were found in age (p-value 0.32), fracture patterns (p-value 0.77), surgical delay (p-value 0.28), surgical time (p-value 0.226), length of hospital stay (p-value 0.921) and blood loss (p-value 0.086) between the two groups.
A significantly higher overall complication rate was observed in the group treated with cannulated screws (p-value 0.004). Analysed separately, a higher rate of avascular necrosis, symptomatic shortening of the femoral neck, protrusion of the osteosynthesis material with or without removal was observed in the group treated with cannulated screws.
ConclusionsThe FNS system represents a safe and reproductible alternative for the fixation of femoral neck fractures, showing non-inferior outcomes to treatment with cannulated screws.
El sistema de cuello femoral «FNS» de DePuy Synthes® (EE. UU., 2018) representa una alternativa reciente para la fijación de las fracturas de cuello femoral, aportando aparentes ventajas biomecánicas con respecto a los tornillos canulados. El objetivo de este estudio es comparar los resultados clínicos de ambos métodos de fijación.
MétodoSe realizó un estudio retrospectivo comparativo entre 36 fracturas subcapitales tratadas mediante sistema FNS y 35 pacientes tratados con tornillos canulados. Se evaluó la edad, el sexo, el patrón fractuario, la demora hasta la intervención y su duración, la estancia hospitalaria y la pérdida de hemoglobina. Además, se analizó durante al menos 12 meses la tasa de necrosis avascular, seudoartrosis, acortamiento sintomático del cuello femoral y protrusión del material con o sin retirada de este.
ResultadosNo se hallaron diferencias significativas en cuanto a edad (valor de p=0,32), patrones de fractura (valor de p=0,77), demora quirúrgica (valor de p=0,28), tiempo quirúrgico (valor de p=0,226), duración de la hospitalización (valor de p=0,921) y pérdida sanguínea (valor de p=0,086) entre los 2 grupos.
Se observó una tasa de complicaciones significativamente superior en su conjunto en el grupo tratado con tornillos canulados (valor de p=0,004). Analizándolas por separado, se apreció una mayor tasa de necrosis avascular, acortamiento sintomático del cuello femoral, protrusión del material de osteosíntesis con o sin retirada en el grupo tratado con tornillos canulados.
ConclusionesEl sistema FNS supone una alternativa segura y reproductible para la fijación de las fracturas de cuello femoral, mostrando resultados no inferiores al tratamiento con tornillos canulados.
The incidence of femoral neck fractures is increasing, partly due to the ageing population. Because of the major socioeconomic impact on patients and their families, as well as on the healthcare system, they are now considered one of the major health threats to the elderly. However, they are not exclusive to this age group, as their incidence is also increasing in young adults, generally due to high-energy trauma.1
These fractures are classically staged according to the Garden classification,2 which assesses the displacement in the coronal plane of the femoral head, and the Pauwels classification,3 which assesses the direction of the fracture line.
Treatment of this type of fracture consists of arthroplasty or internal fixation, depending on the degree of displacement, the verticality of the fracture line, the progression time of the fracture, the bone quality, the clinical situation of the patient, or the experience of the surgeon.4 In general, and despite inconsistencies in the literature regarding the best treatment protocol, osteosynthesis is recommended in young patients, regardless of the degree of displacement and the verticality of the line, since preserving the femoral head is a priority objective,5 and in middle-aged or elderly patients with not very vertical lines (Pauwels I or II) and without displacement (Garden I or II).6
Achieving absolute stability against rotational and vertical shear forces is a challenge in the fixation of these fractures. Inverted triangular cannulated screws have been the most commonly used fixation system with generally satisfactory results. However, available meta-analyses, such as that by Xia et al.,7 report significant rates of nonunion (8.3%), fixation failure (8.4%), and need for revision (8.2%). Furthermore, Stockton et al.8 report a rate of varus collapse of 8% and Jansen et al.9 report a risk of peri-implant subtrochanteric fracture of between 2.5% and 5.7%.
This scenario has motivated the continuous search for a system that offers greater rotational control and stability in the sagittal and coronal planes, as well as a lower complication and revision rate, which, according to the literature, reaches 22% for cannulated screw osteosynthesis.10
In this sense, the Femoral Neck System (FNS) developed by DePuy Synthes® (USA, 2018) offers, in biomechanical studies, the advantages of combining the properties of interfragmentary compression and anti-rotation in internal fixation, as well as allowing immediate loading regardless of bone quality11 (Fig. 1). The aim of this study is to compare the clinical results of these two osteosynthesis methods in terms of intraoperative results, immediate postoperative results, and medium-term complication rates.
Material and methodA retrospective comparative study was conducted on 36 patients who underwent surgery for a femoral neck fracture using the DePuy Synthes FNS system between July 2020 and April 2023, and 35 patients who underwent surgery using osteosynthesis with 6.5mm diameter partial-thread cannulated steel screws in an inverted triangle position between July 2017 and June 2023. Cases that did not complete 12 months of follow-up due to death (2 patients in each group), loss to follow-up, or recent surgery were excluded.
The study was conducted in accordance with the ethical standards recognised by the Declaration of Helsinki and Resolution 008430 of 1993, and was approved by the Institutional Ethics Committee (internal code 2024/280), with the informed consent of all patients included in the study.
The mean follow-up was 24 months (12–40) in the FNS group and 23 months (12–34) in the cannulated screw group.
Females predominated in both the FNS treated group (58.3% females) and the cannulated screw treated group (74.3% females). The mean age of patients treated with the Synthes FNS system was 63.3 years (25–94) and 65 years (29–85) for patients treated with cannulated screws.
The mean time from arrival at the emergency department to surgery was 27h (2–90h) in the FNS group and 33h (3–96h) in the cannulated screw group.
All the patients were operated on by the same 6 surgeons from the centre's trauma unit. The first 32 patients in the cannulated screw group were consecutive, as this was the implant of choice for osteosynthesis of femoral neck fractures at the centre until July 2020. Since then, as the FNS system has become established in daily practice, one implant or the other has been used according to the surgeon's preference, with no additional criteria for implant selection that could distort the results.
Positioning on the operating table was in all cases using a traction table, with the appropriate manoeuvres to achieve a closed reduction if necessary. The postoperative protocol in both groups consisted of progressive partial weight-bearing from the first day after surgery, together with assisted hip and knee flexion-extension exercises supervised by a physiotherapist.
Data were obtained from electronic medical records and images from the radiology picture archiving and communication system (PACS). The following data were analysed: age, sex, hours of surgical delay, type of fracture according to the Garden and Pauwels classifications, duration of surgery, days of admission, decrease in haemoglobin values between preoperative and 24-hour postoperative analysis, and late complications (avascular necrosis, pseudoarthrosis, femoral neck shortening, discomfort related to the material and implant removal).
SPSS version 29.0 (SPSS Inc. Chicago, IL, USA) was used for statistical analysis. Fracture type according to Garden and Pauwels classifications, sex, rates of avascular necrosis, pseudarthrosis, femoral neck shortening, discomfort related to the material and implant removal were expressed as frequencies and analysed using the χ2 test. Age, delay until surgery, operative time, length of hospital stay, and haemoglobin loss were expressed as mean±standard deviation and analysed using Student's t-test for independent samples. Tests with a p-value≤.05 were considered statistically significant.
ResultsNo statistically significant differences were observed with respect to age (63.3±16.83 in the FNS treated group vs. 65.09±14.41 in the cannulated screw treated group, p-value=.32), sex (p-value=.155), follow-up time (p-value=.85), or surgical delay between the two groups (p-value=.28).
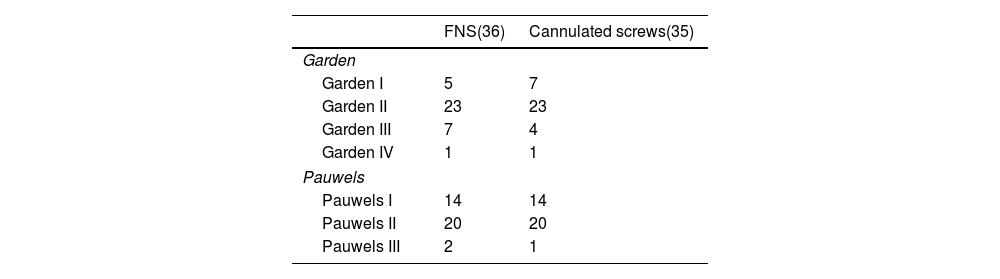
The number of fractures according to Garden and Pauwels classifications is shown in Table 1. Both samples were considered homogeneous as there was no statistically significant difference between the groups, with a value of p=.77 for the Garden classification and p=.86 for the Pauwels classification.
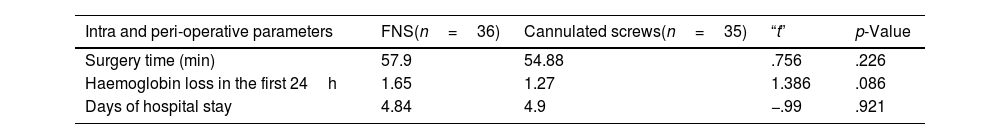
The data on surgical time, need for transfusion, and hospital stay are detailed in Table 2. Longer surgery time and greater haemoglobin loss were observed in patients treated with the FNS system, although this difference was not statistically significant. The length of hospital stay was comparable between the two groups.
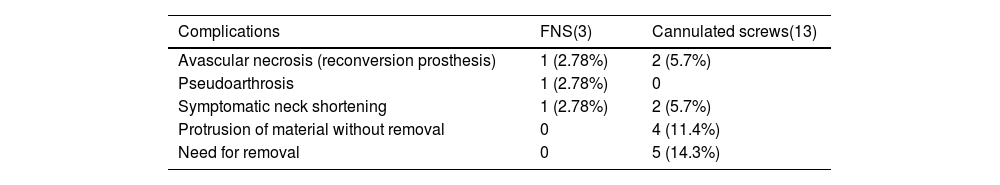
During the follow-up period, the following complications were observed in both groups, as summarised in Table 3. Combining the total number of complications for each group, there were three in the group treated with the FNS system (complication rate of 8.33%) and a total of 13 in the patients treated with cannulated screws (complication rate of 37.14%). A statistical comparison of the data showed a significant difference in overall complications between the two groups, with a p-value of .004.
Rate of late complications in both groups.
| Complications | FNS(3) | Cannulated screws(13) |
|---|---|---|
| Avascular necrosis (reconversion prosthesis) | 1 (2.78%) | 2 (5.7%) |
| Pseudoarthrosis | 1 (2.78%) | 0 |
| Symptomatic neck shortening | 1 (2.78%) | 2 (5.7%) |
| Protrusion of material without removal | 0 | 4 (11.4%) |
| Need for removal | 0 | 5 (14.3%) |
Looking at late complications individually, the rates of avascular necrosis requiring conversion to arthroplasty, symptomatic femoral neck shortening and nonunion were higher in the cannulated screw group, but the incidence was not high enough to be statistically significant. However, the rate of discomfort associated with osteosynthesis, with or without the need for its removal, was significantly lower in the FNS group (p-value<.001.
DiscussionOsteosynthesis of femoral neck fractures remains a surgical challenge because of the consequences of a poor clinical outcome for the patient, their family, and the healthcare system. Although a number of factors have been defined to predict a good surgical outcome, such as early fixation, it has been shown that anatomical and stable reduction is the most important factor, allowing immediate mobilisation and ambulation and reducing the risk of late complications.12
With regard to fixation methods, they should allow implantation in a short surgery time, provide a stable construct that allows immediate weightbearing and controlled fracture collapse, cause the least radiation to the patient and surgical team, cause little soft tissue aggression and therefore reduce blood loss, and be reproducible to minimise the influence of the surgeon factor in the placement of the material.
Osteosynthesis with three percutaneous cannulated screws in an inverted triangle poses a number of problems in some of the aspects mentioned above. On the one hand, freehand placement means longer intraoperative fluoroscopy time,13 and increases the likelihood of surgical errors. For example, placing the lower screw distal to the lesser trochanter may predispose to the occurrence of a subtrochanteric peri-implant fracture, as mentioned above. On the other hand, in patients with poor bone quality, posterior comminution or vertical features (Pauwels III), the stability of the assembly is compromised as the system cannot control vertical shear forces. Furthermore, significant rates of marked shortening of the femoral neck due to fracture collapse have been reported,14 which is a reason for loss of hip abductor torque and a relatively common cause of dissatisfaction and pain.15
These limitations, among others, have led to the search for new systems that improve the results of traditional fixation systems. In this sense, the Synthes FNS system consists of a lateral plate that provides angular stability, a bolt that allows controlled collapse and an anti-rotation screw that provides rotational stability. In addition, the fact that the bolt is inserted by impaction avoids the risk of head rotation associated with cannulated screws or classic screw-plate systems.16
Biomechanical studies performed on cadavers to validate the FNS system have shown that its structural stability is greater than that of cannulated screws,17 and that this implant is less sensitive to variations in placement.18 Studies based on finite element analysis, such as the one developed by Huang et al.,19 show that the FNS system has a greater anti-slip capacity than cannulated screws at 55°, 65°, and 75° angulation lines in the coronal plane, i.e., Pauwels II and III fractures.
With regard to daily clinical practice, the FNS system has confirmed the results of biomechanical analyses, showing better control of shear forces in Pauwels II and Pauwels III fractures,20 and a shorter time to fracture healing.21 Lin et al.22 found a significantly lower complication rate in patients treated with the FNS system (14.8%) compared to those treated with cannulated screws (38.7%) for Pauwels III fractures.
In addition, as a fully guided implantation system, the final configuration is more predictable than when 3 cannulated screws are inserted using a freehand technique. This has been associated with fewer technique related errors and less use of intraoperative fluoroscopy.23
Fixation with cannulated screws is a percutaneous technique, whereas implantation of the FNS system requires a lateral incision of approximately 6cm, resulting in greater exposure of soft tissue. However, this does not appear to correlate with a statistically higher risk of intra-operative bleeding,24 a circumstance also observed in the current study as the differences in haemoglobin loss between the two groups did not reach statistical significance.
The duration of surgery with this new implant has also been the subject of controversy in the literature. On the one hand, authors such as Nibe et al.25 report that the duration of surgery in patients treated with the FNS system is significantly shorter than in those treated with cannulated screws, because it is a practically guided system. However, other authors such as Tang et al.26 suggest similar data to cannulated screw treatment or even a longer surgery time, attributing this to the learning curve required to place this new implant.
The data from this study show a longer surgery time in the FNS group, although this difference is not statistically significant. The average duration of FNS implantation is at the upper end of that reported in similar studies (Fig. 2).
In terms of length of hospital stay, similar comparative studies have suggested that the FNS system does not result in longer hospital stays, despite the greater soft tissue dissection required for implantation,27 and this was confirmed in this study. The results obtained in patients treated with the FNS system in terms of total days in hospital are in line with recently published results in this area (Fig. 3).
Comparison between total days of hospital stay of the FNS sample and those reported in the literature.28,29
The available literature suggests that the use of the FNS system generally seems to correlate with fewer complications, always with the caution implied by the short follow-up period given the recent introduction of this implant. This is also evident in the data of the series, as the pooled complication rate is significantly lower in the group of patients treated with the FNS system. The reoperation rates for this implant in recent publications range from 9.2% as reported by Davidson et al.30 to 18% as reported by Obey et al.31 The 2 cases of surgical revision in the FNS group represent a revision rate of 5.56%, which is significantly lower than that reported in the aforementioned studies. The reoperation rate reported in this study for cannulated screw osteosynthesis (20%) is similar to that published in the literature (22%10).
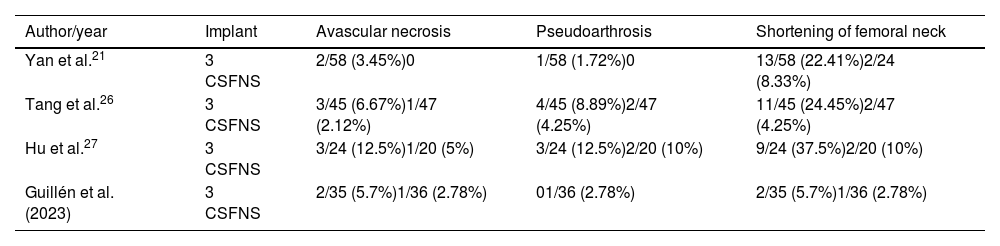
Looking at complications separately, the literature suggests that cannulated screw fixation correlates with a higher rate of nonunion, avascular necrosis and need for removal of material, in addition to the already mentioned significant fracture collapse. In the study population, all of the aforementioned complications are more common in the cannulated screw group, with the exception of nonunion (Table 4), although a larger sample size is required for the difference in the percentage of complications such as nonunion, avascular necrosis, or symptomatic neck shortening to be considered relevant.
Comparison of the complications of the FNS system in this study with similar studies.
| Author/year | Implant | Avascular necrosis | Pseudoarthrosis | Shortening of femoral neck |
|---|---|---|---|---|
| Yan et al.21 | 3 CSFNS | 2/58 (3.45%)0 | 1/58 (1.72%)0 | 13/58 (22.41%)2/24 (8.33%) |
| Tang et al.26 | 3 CSFNS | 3/45 (6.67%)1/47 (2.12%) | 4/45 (8.89%)2/47 (4.25%) | 11/45 (24.45%)2/47 (4.25%) |
| Hu et al.27 | 3 CSFNS | 3/24 (12.5%)1/20 (5%) | 3/24 (12.5%)2/20 (10%) | 9/24 (37.5%)2/20 (10%) |
| Guillén et al. (2023) | 3 CSFNS | 2/35 (5.7%)1/36 (2.78%) | 01/36 (2.78%) | 2/35 (5.7%)1/36 (2.78%) |
As shown in Table 4, the rate of avascular necrosis and nonunion in both groups in this study is significantly lower than in most similar studies. However, further follow-up of recent cases and a larger sample size will be required to confirm these data.
ConclusionsThe FNS Synthes® system represents a safe and reproducible alternative for the osteosynthesis of femoral neck fractures, with postoperative results comparable to those of osteosynthesis with cannulated screws and promising results regarding a lower complication rate.
Limitations of this studyThis study has the following potential limitations. Firstly, it is a retrospective study. However, the different degree of initial displacement and the verticality of the fracture line affect the incidence of postoperative complications. Therefore, we can conclude that there is a slight heterogeneity between the two groups and also in comparison with other studies with regard to the classifications of Pauwels and Garden, which could cause a bias in the incidence of complications. In addition, a larger sample size and longer follow-up of patients would be desirable to confirm the low rate of complications that develop with this new implant.
Furthermore, the lack of randomisation of treatments could have introduced a kind of selection bias.
Level of evidenceLevel of evidence ii.
Informed consentThe authors hereby declare that the Centre's Ethics Committee has approved the writing of this scientific article.
We also declare that, as is standard practice, informed consent was obtained from the patients for the scientific and informative use of all personal data and images.
FundingNo specific support from public sector agencies, commercial sector, or not-for-profit organisations was received for this research study.
Conflict of interestsThe authors have no conflict of interests to declare.
None.